Abstract
We describe the use of telemedicine by the Biobehavioral Service at the University of Iowa Hospitals and Clinics to conduct brief functional analyses for children with developmental and behavioral disorders who live in rural areas of Iowa. Instead of being served at our outpatient facility, participants received initial behavioral assessments in their local schools or social service agencies via videoconference. Case descriptions for 2 participants whose evaluations were conducted via telemedicine, and a brief summary of all outpatient assessments conducted over a 4-year period by the Biobehavioral Service, are provided. This report extends previous applications of functional analysis procedures by examining brief behavioral assessments conducted via telemedicine.
Keywords: brief functional analysis, severe problem behavior, telemedicine
As described by Northup et al. (1991) and summarized by Derby et al. (1992), brief functional analysis procedures have proven useful for evaluating severe problem behaviors (e.g., self-injury) in outpatient clinic settings. The brief functional analysis is based directly on functional analysis procedures described by Iwata, Dorsey, Slifer, Bauman, and Richman (1982/1994) and involves the rapid presentation of test and control conditions within a limited time period (e.g., 90 min). Typically, sessions are conducted for 5 min and yield a single data point per test condition. Brief functional analyses have clinical utility because the assessment can be conducted in time-limited settings such as outpatient clinics, and treatment can be matched to maintaining reinforcement contingencies. This has led to multiple applications and extensions of brief functional analyses (e.g., Cooper, Wacker, Sasso, Reimers, & Donn, 1990; Cooper et al., 1992; Harding et al., 1999), and subsequent studies (Kahng & Iwata, 1999; Wallace & Knights, 2003) have demonstrated a high correlation between the outcomes of brief and extended functional analyses.
In outpatient clinics such as the Biobehavioral Service (BBS) at the University of Iowa, the brief functional analysis has been used extensively in clinical evaluations (Wacker et al., 1994). Most of these evaluations involve using parents or other care providers as therapists, because the procedures are relatively easy to conduct with coaching from staff. These practical benefits of brief functional analyses make them ideally suited for other applications, such as telemedicine.
Previous studies of other health care disciplines have shown that telemedicine can be a cost-effective service-delivery model. For example, Morrison, Bergauer, Jacques, Coleman, and Stanziano (2001) evaluated the cost effectiveness of telemedicine consultation compared with a conventional outpatient consultation (the control group) to monitor and consult with women who had been diagnosed with preterm labor. Their results showed that the mean cost per pregnancy for the telemedicine group was approximately one third of the cost of the control group. These results suggest that telemedicine may be a cost-effective method of providing frequent monitoring and consultation, thereby reducing the cost of more intensive intervention in an outpatient or inpatient clinic. Based on similar rationales, telemedicine services have expanded to include a wide variety of medical and behavioral consultation services, including applied behavior analysis. For example, groups such as Advoserv and C-Now Inc. support the use of interactive video technology to provide services such as applied behavior analysis and special education to children with behavior problems in foster care settings in the state of Florida (McGimsey, Baker, & Favell, 2004).
In 1987, the state of Iowa established the Iowa Communications Network (ICN), which is a 2,800-mile fiber-optic telecommunications system (the University of Iowa's National Laboratory for the Study of Rural Telemedicine). With the establishment of the ICN, telemedicine in Iowa was made possible because the fiber-optic cable system connected most hospitals and high schools throughout the state. Located in all 99 counties in Iowa, the ICN was primarily intended for educational purposes. However, in 1994, medical and health care facilities were given access to the ICN with the hope of enhancing and supporting rural medical institutions. In 1996, the United States National Library of Medicine awarded 19 multiyear grants to projects in rural, inner city, and suburban areas across the United States to evaluate the impact of telemedicine on ”cost, quality, and access to health care„ (NLM National Telemedicine Initiative; Kienzle, 2000).
At the University of Iowa, telemedicine services were initiated with funding from the National Library of Medicine, with initial projects in pediatrics including the divisions of cardiology (e.g., to evaluate echocardiograms) and developmental disabilities (e.g., to evaluate the swallowing skills of children with disabilities and oral motor problems associated with eating). The telemedicine service in developmental disabilities was conducted at the Center for Disabilities and Development (CDD) at the University of Iowa Hospitals and Clinics (UIHC). As part of this telemedicine service in developmental disabilities, the BBS clinic began to provide telemedicine services. The reason for initiating telemedicine services through the clinic was based solely on practical needs. Iowa is largely a rural state, and the average family travels approximately 145 km one way to receive services at the clinic. The need to travel long distances and, in some cases, the lack of local trained personnel often preclude the provision of behavioral services to individuals and their care providers and can make follow-up visits difficult and costly.
In this article, we provide two case examples that illustrate how telemedicine has been used to conduct brief functional analyses for children who exhibit severe problem behavior. Both participants were individuals who resided in rural settings and for whom travel to the CDD was difficult, and both participants received services solely via the ICN. In addition, a brief summary of all cases conducted by the BBS clinic via the ICN during the 1997–2000 project period is provided (these were the first 4 years for which the BBS clinic provided statewide consultation via the ICN service).
Case Examples
Participants
Charlie was a 5-year-old boy who had been diagnosed with autism and who received services through a community special education preschool located approximately 193 km from the CDD. Daisy was a 1-year-old girl who had multiple disabilities, including vision and hearing impairments, and severe mental retardation. She had been diagnosed with neurogenic dysphagia, DiGeorge syndrome, cleft lip and palate, and seizure disorder. At the time of this study, Daisy was in foster care, lived approximately 145 km from the CDD, and received in-home services through the Iowa Department of Human Services (DHS). She had recently undergone surgery for cleft palate repair, and her self-injury (nose flicking) was causing damage to the area recently reconstructed by surgery. Both children had been referred for clinical evaluation of severe problem behavior (i.e., disruption and self-injury), and their families elected to participate in the telemedicine project rather than travel to the CDD.
Settings and Materials
For each evaluation, consultation was conducted between the host site (the telemedicine studio located at the CDD at UIHC) and a remote site located in the participants' home communities. The consulting clinicians were located at the host site, and evaluations were conducted by care providers and local service teams at the remote sites (described below). The host and remote sites were connected via the ICN and were equipped with television monitors, a camera that transmitted and recorded audio and visual information between the sites, microphones, and a multimedia projector. The main camera used at the host site responded to infrared signals that were activated by the touch-to-speak microphones used by the speakers in the studio. Therefore, when a speaker pushed the button to speak, the camera zoomed in on that person. A desktop computer was available to deliver presentations using Microsoft PowerPoint® and to show digital pictures, graphs, and other electronic media. A touchscreen monitor was used to switch between the sites and among the various media available in the studio. A videotape recorder was also available at the host studio to record observations transmitted from the remote sites. (For more detailed information regarding the equipment used in the studios, the Distance Learning Classroom Basics Handbook can be downloaded from www.k12connections.iptv.org/pdfs/ICNBasics.pdf.)
The remote site for Charlie's assessment was the conference room of a local elementary school. The conference room had an attached observation room and was equipped with a one-way mirror and the video-conferencing equipment. Charlie's assessment was conducted by his classroom teacher with on-site coaching from the school psychologist. The first and second authors were present at the CDD (the host site). Data were collected at the host site, and graphic displays of data were reviewed via the multimedia projector with the school team at the remote site following each 5-min session.
During Daisy's assessment, two remote sites were connected to the host site: One studio was located at the local DHS office and the other at the local school that provided consultation services to the family. Several members of the local team who worked with Daisy's family (e.g., social worker, early childhood special education teacher, physical therapist, nurse practitioner, pediatrician), her foster mother, and her biological mother were present at the DHS office during the assessment. In addition, a vision specialist provided consultation during the assessment from the second remote site located at the school. All of Daisy's assessment conditions were conducted by her foster mother and her physical therapist.
Response Measurement and Reliability
Charlie had been referred by his school for a brief functional analysis of disruptive behavior, which included screaming (defined as loud vocalizations above the intensity of normal speech), noncompliance (defined as saying “no” and pushing the task away when demands were presented), and destruction (defined as throwing objects). All target responses were recorded using a frequency measure and were converted to a response rate (responses per minute) for the purpose of data analysis.
Daisy had been referred by her pediatrician for assessment and treatment of severe self-injury. Self-injury included hand biting (defined as contact of her hand with her teeth) and nose flicking (defined as touching her nostril or septum or inserting her fingers in her nostril). Data on self-injury were collected using a 6-s partial-interval recording system. Data were analyzed by calculating the percentage of 6-s intervals in which the target response occurred (i.e., number of intervals with the target response divided by total number of intervals, multiplied by 100%).
During the functional analyses for Charlie and Daisy, data were collected by the first or second author at the host site. During 100% of the functional analysis sessions for Charlie and 33% of all sessions for Daisy, a second observer independently but simultaneously collected data. For both participants, interobserver agreement data were collected on the occurrence of target behaviors using exact frequency or interval calculation procedures. Interobserver agreement for frequency measures was calculated by dividing the smaller number of occurrences by the larger number of occurrences within each session and multiplying the resulting quotient by 100%. Interobserver agreement for 6-s interval data was calculated by dividing the number of intervals with agreement on the occurrence of a response by the number of intervals with agreement on the occurrence of a response plus the number of intervals with disagreements on the occurrence of a response multiplied by 100%. Mean agreement for Charlie was 95% (range, 75% to 100%) and for Daisy was 96% (range, 93% to 100%).
Experimental Design and Procedure
The functional analysis was based on procedures described by Iwata et al. (1982/1994) and Northup et al. (1991) and was conducted within a multielement design for both participants. Each session of the functional analysis lasted 5 min, and all conditions were conducted in a counterbalanced fashion.
Prior to conducting Charlie's functional analysis, the school staff completed and mailed a Motivation Assessment Scale (MAS; Durand & Crimmins, 1992), and a descriptive observation (Bijou, Peterson, & Ault, 1968) was conducted in Charlie's classroom by the local school psychologist. The descriptive observation and MAS results were reviewed by the first and second authors, and based on these measures, it was hypothesized that Charlie's disruptive behavior was maintained by negative reinforcement (escape from demands) or automatic reinforcement. A brief functional analysis was designed to test these hypotheses and was conducted across three conditions: (a) free play, (b) escape, and (c) alone. During free play, Charlie was allowed continuous access to preferred activities and his teacher's attention. All occurrences of disruptive behavior were ignored. During the escape condition, Charlie's teacher instructed him to work on an academic task. Contingent on the occurrence of disruptive behavior, Charlie was given a brief break of approximately 20 s. During the alone condition, all activities were removed and Charlie was left alone in the conference room.
Prior to Daisy's evaluation, the first author conducted a phone interview with Daisy's foster mother to develop hypotheses regarding the environmental variables that maintained Daisy's self-injury. Although her foster mother reported that Daisy engaged in self-injury that occurred at high levels throughout the day, based on information provided during this interview we hypothesized that self-injury was maintained by escape from demands and, specifically, from physical therapy exercises. Daisy's functional analysis was conducted across three conditions: (a) free play, (b) escape, and (c) attention. The free play condition was identical to that described above; however, Daisy was placed on a blanket in the middle of the room throughout the session. The escape condition for Daisy was similar to that conducted for Charlie, except that the demands consisted of her physical therapist conducting range-of-motion exercises. During the attention condition, Daisy was left on the blanket with her toys. Contingent on the occurrence of self-injury, she was provided with 20 to 30 s of attention in the form of a mild reprimand and was redirected to her toys.
Specific Procedures for Conducting Assessments Using the ICN
The school psychologist who worked with Charlie had previously observed evaluations at the outpatient clinic housed at the CDD and was familiar with functional analyses and visual inspection of data. However, she was not formally trained in conducting functional analyses or visual interpretation of data, and no preassessment meetings were conducted prior to the telemedicine evaluation. The school psychologist consulted with the clinicians at the host site during the evaluation, and the teacher conducted all sessions of the functional analysis. During Charlie's functional analysis, a clip microphone was affixed to a table in the center of the room, which allowed continuous audio transmission to the host site. In addition, the consultants at the host site reviewed the graphic displays of the occurrence of target behavior via the data projector. The order of conditions was based on visual inspection of graphs. Thus, if changes in the target behavior occurred during a test condition, a condition that resulted in low levels of behavior was repeated and was followed by the test condition.
Prior to Daisy's functional analysis, the first author reviewed the purpose and procedures of the functional analysis with Daisy's foster mother via telephone. Written instructions on how to conduct each condition were also mailed to her. During the functional analysis, a touch-to-speak microphone was placed near the mat on which Daisy was placed. These microphones at the host and remote sites had a button that the user depressed for the duration of speaking. As a result, audio communication via microphones between the host and remote sites were mutually exclusive. During each session of Daisy's functional analysis, a weight was placed on the button of the microphone at the remote site to allow continuous audio transmission during each 5-min session. At the beginning of each session, the consultant at the host site held up a placard with the name of the condition (free play, attention, escape). If the procedures had required adjustment (none were needed), the consultants at the remote site would have raised their hands, the button on the microphone at the remote site would have been released, and feedback would have been provided. The end of each 5-min session was indicated when a consultant at the host site held up a card with “5 minutes” printed on it.
Results
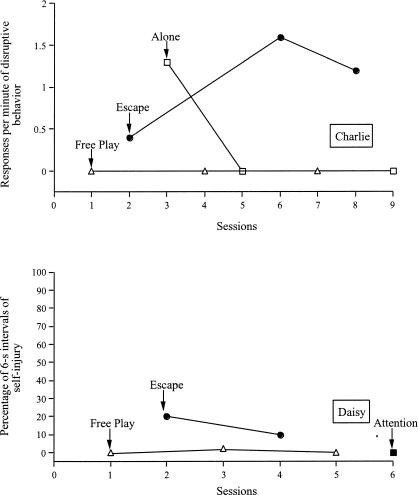
Charlie's results are shown in Figure 1 and suggest that his disruptive behavior was maintained by negative reinforcement in the form of escape from demands. Problem behavior occurred initially during the first alone condition, but decreased to zero in the next two sessions. The results of Daisy's functional analysis are also shown in Figure 1. Her self-injury occurred at the highest levels during the escape condition, suggesting that this behavior was maintained by negative reinforcement (escape from physical therapy exercises). Although a decline in the percentage of self-injury occurred between the first and second sessions, her local team indicated that they were convinced by the findings and expressed concern over the severity of her self-injury during the two escape sessions.
Figure 1. Responses per minute of disruptive behavior during functional analysis for Charlie (top) and percentage of 6-s intervals of self-injury during functional analysis for Daisy (bottom).
Discussion
These results showed that functional analyses were successfully conducted using telemedicine technology. The brief functional analyses were completed in the children's local environments. Moreover, the children's primary care providers conducted the analyses. Based on recent legislation (Part C of the Individuals with Disabilities Education Act, PL 105-17, 1997) requiring that early intervention services be provided in the child's natural environment, the use of telemedicine may increase the social validity of the applied behavior analysis service delivery as well as the efficiency of the procedures.
For each child, involvement of the local team during the functional analysis was important because the results obtained were different than what they had expected. It is possible that the results would not have been as convincing for the local team had we obtained them in our clinic without the team's participation. For example, the local team hypothesized that Charlie's disruptive behavior was maintained by automatic reinforcement. This was not supported by the obtained functional analysis results, which showed a negative reinforcement (escape) function. For Daisy, the local team was surprised that she engaged in self-injury to escape physical therapy. Because the physical therapist conducted the assessment, no concerns were raised regarding the physical therapy procedures employed.
These results are similar to those of earlier reports (Harding et al., 1999; Iwata et al., 2000) that showed that functional analysis procedures are not overly difficult to learn or to administer. The advantage of telemedicine is that necessary consultation can be provided in a cost-effective manner (e.g., there are no travel or time expenditures). During both evaluations, intermittent consultation, mostly in the form of reassurance that the procedures were being conducted correctly, was needed.
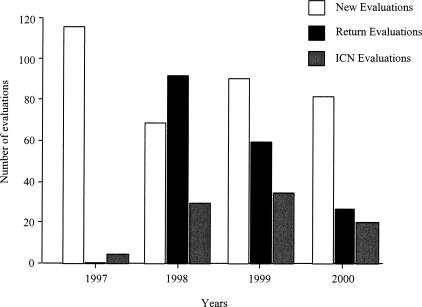
Throughout the project period (1997 to 2000), the BBS completed over 75 telemedicine evaluations such as those described above. A summary of initial and follow-up evaluations in the BBS clinic as well as telemedicine evaluations conducted by the service during this 4-year period is shown in Figure 2. New evaluations conducted in the outpatient clinic comprised the majority of cases, followed by follow-up clinic evaluations, and finally ICN evaluations. Throughout this period, the number of return evaluations conducted in the clinic decreased. This decrease may be accounted for by the increase in the number of ICN evaluations, which suggest that follow-up services may be a practical use of telemedicine. For example, assessments such as functional analyses that are conducted in clinic settings can be described to an entire local service team in an efficient manner via telemedicine during a follow-up evaluation. In addition, the ICN is applicable to initial screening and follow-up consultation. In approximately 25% of referred cases, we were able to provide sufficient initial and follow-up consultations to avoid costly trips to the clinic for the children and their families.
Figure 2. Summary of new and return evaluations conducted in clinic and ICN evaluations conducted during the 1997–2000 period.
At present, the UIHC holds a multiyear contract with the Iowa Department of Education to provide ICN consultations for teachers, childhood service providers, and families both prior to and following initial clinic evaluations. During 2005, the BBS conducted 200 telemedicine consultations, with the majority being descriptive assessments and initial screenings. In almost half these cases, we were able to forgo subsequent clinic visits through treatment recommendations that were directed via the ICN and implemented by the local teams.
In summary, the use of telemedicine by experienced applied behavior analysts appears to be an efficient method for conducting brief functional analyses, follow-up consultations, and descriptive screenings to assess severe behavior disorders. Telemedicine services permit experts in functional analysis and function-based treatments to consult directly with local service teams and care providers in the assessment and treatment of problem behavior. Presently, insurance companies have not covered telemedicine evaluations conducted by behavior analysts in Iowa. However, contracts through agencies such as the Iowa Department of Education have been successfully obtained to fund these services. As technologies expand to include systems such as Web-based interactive video, even more options will be available to expand the delivery of functional analysis and function-based treatment services for children with behavior problems.
Acknowledgments
This study was funded by the National Library of Medicine and the National Institute of Child Health and Human Development. However, the opinions expressed in this article do not necessarily express the opinions of either agency. We express our gratitude to the local service teams for their efforts.
References
- Bijou S.W, Peterson R.F, Ault M.H. A method to integrate descriptive and experimental field studies at the level of data and empirical concepts. Journal of Applied Behavior Analysis. 1968;1:175–191. doi: 10.1901/jaba.1968.1-175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper L.J, Wacker D.P, Sasso G.M, Reimers T.M, Donn L.K. Using parents as therapists to evaluate appropriate behavior of their children: Application to a tertiary diagnostic clinic. Journal of Applied Behavior Analysis. 1990;23:285–296. doi: 10.1901/jaba.1990.23-285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper L.J, Wacker D.P, Thursby D, Plagmann L.A, Harding J, Millard T, et al. Analysis of the effects of task preferences, task demands, and adult attention on child behavior in outpatient and classroom settings. Journal of Applied Behavior Analysis. 1992;25:823–840. doi: 10.1901/jaba.1992.25-823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derby K.M, Wacker D.P, Sasso G, Steege M, Northup J, Cigrand K, et al. Brief functional assessments techniques to evaluate aberrant behavior in an outpatient setting: A summary of 79 cases. Journal of Applied Behavior Analysis. 1992;25:713–721. doi: 10.1901/jaba.1992.25-713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durand V.M, Crimmins D.B. The motivation assessment scale (MAS) administration guide. Topeka, KS: Monaco & Associates; 1992. [Google Scholar]
- Harding J.W, Wacker D.P, Berg W.K, Cooper L.J, Asmus J, Mlela K, et al. An analysis of choice making in the assessment of young children with severe behavior problems. Journal of Applied Behavior Analysis. 1999;32:63–82. doi: 10.1901/jaba.1999.32-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- lwata B.A, Dorsey M.F, Slifer K.J, Bauman K.E, Richman G.S. Toward a functional analysis of self-injury. Journal of Applied Behavior Analysis. 1994;27:197–209. doi: 10.1901/jaba.1994.27-197. (Reprinted from Analysis and Intervention in Developmental Disabilities, 2, 3–20, 1982) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iwata B.A, Wallace M.D, Kahng S, Lindberg J.S, Roscoe E.M, Conners J, et al. Skill acquisition in the implementation of functional analysis methodology. Journal of Applied Behavior Analysis. 2000;33:181–194. doi: 10.1901/jaba.2000.33-181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahng S, Iwata B.A. Correspondence between outcomes of brief and extended functional analyses. Journal of Applied Behavior Analysis. 1999;32:149–159. doi: 10.1901/jaba.1999.32-149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kienzle M. Rural-academic integration: Iowa's National Laboratory for the Study of Rural Telemedicine. 2000. Retrieved November 3, 2003 from http://telemed.medicine.uiowa.edu/TRCDocs/publications.html. [Google Scholar]
- McGimsey J, Baker L, Favell J. Examining the application of interactive video in foster home settings. In: Barretto (Chair) Anjali., editor. The application of telehealth to behavioral assessment and rehabilitation services. 2004. May, In. Paper presented at the annual conference of the Association for Behavior Analysis, Boston. [Google Scholar]
- Morrison J, Bergauer N.K, Jacques D, Coleman S.K, Stanziano G.J. Telemedicine: Cost-effective management of high-risk pregnancy. 2001. Retrieved July 3, 2005, from http://www.managedcaremag.com/archives/0111/0111.peer_highrisk.html. [PubMed] [Google Scholar]
- Northup J, Wacker D, Sasso G, Steege M, Cigrand K, Cook J, et al. A brief functional analysis of aggressive and alternative behavior in an outclinic setting. Journal of Applied Behavior Analysis. 1991;24:509–522. doi: 10.1901/jaba.1991.24-509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The University of Iowa's National Laboratory for the Study of Rural Telemedicine. Retrieved November 3, 2003, from http:/www.janela1.com/vh/docs/v0001535.htm. [Google Scholar]
- Wacker D.P, Berg W.K, Cooper L.J, Derby K.M, Steege M.W, Northup J, et al. The impact of functional analysis methodology on outpatient clinic services. Journal of Applied Behavior Analysis. 1994;27:405–407. doi: 10.1901/jaba.1994.27-405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallace M.D, Knights D.J. An evaluation of a brief functional analysis format within a vocational setting. Journal of Applied Behavior Analysis. 2003;36:125–128. doi: 10.1901/jaba.2003.36-125. [DOI] [PMC free article] [PubMed] [Google Scholar]