Abstract
Objective
To examine the effect of rural hospital closures on the local economy.
Data Sources
U.S. Census Bureau, OSCAR, Medicare Cost Reports, and surveys of individuals knowledgeable about local hospital closures.
Study Design
Economic data at the county level for 1990–2000 were combined with information on hospital closures. The study sample was restricted to rural counties experiencing a closure during the sample period. Longitudinal regression methods were used to estimate the effect of hospital closure on per-capita income, unemployment rate, and other community economic measures. Models included both leading and lagged closure terms allowing a preclosure economic downturn as well as time for the closure to be fully realized by the community.
Data Collection
Information on closures was collected by contacting every state hospital association, reconciling information gathered with that contained in the American Hospital Association file and OIG reports.
Principal Findings
Results indicate that the closure of the sole hospital in the community reduces per-capita income by $703 (p<0.05) or 4 percent (p<0.05) and increases the unemployment rate by 1.6 percentage points (p<0.01). Closures in communities with alternative sources of hospital care had no long-term economic impact, although income decreased for 2 years following the closure.
Conclusions
The local economic effects of a hospital closure should be considered when regulations that affect hospitals' financial well-being are designed or changed.
Keywords: Hospital closure, community economy, economic development
Hospitals are generally considered to be the locus of rural health care systems. Not only are important health services based at hospitals, but many of a community's health care personnel are either directly employed by or supported by the local hospital. Further, hospitals are often considered vital to local economies as they bring outside dollars into the communities via third-party payors, provide jobs, stimulate local purchasing, and help attract industry and retirees (Doeksen et al. 1997). As such, the closure of a hospital can have detrimental effects on a rural community. The rapid succession of hospital closures throughout the 1980s and 1990s helped stimulate legislation, such as creation of Critical Access Hospitals (hospitals that accept certain restrictions and are reimbursed 101 percent of cost from Medicare), designed to ensure the financial viability of small rural hospitals.
The number of small rural hospitals that have chosen to convert to CAH status has risen beyond expectations; as on August 2004, 959 small rural hospitals (over 40 percent of all rural hospitals) have opted out of Prospective Payment System by converting (Flex Monitoring Team 2005). In some policy circles, concern has been expressed about the effect on the Prospective Payment System of so many hospitals taking advantage of the protection of cost-based reimbursement (MEDPAC 2003). In light of these concerns, this is an opportune time to more accurately assess the economic importance of small rural hospitals to their communities, and to estimate the potential impact of their closure, should favorable reimbursement policies be changed.
The effect of hospital closures on the health of community members has been relatively well documented and is not the focus of this study. For example, Reif, Des Harnais, and Bernard (1999) study six communities experiencing a hospital closure and conclude that hospital closures decrease access to health care, whereas Rosenbach and Dayhoff (1995) find that per-capita Medicare expenditures grew at a slower rate in communities experiencing a closure. Fleming et al. (1995) find that residents of communities with a hospital closure experienced a mean increase in travel time to care of about 30 minutes. Rather, we are concerned with the relationship between a hospital closure and the local economic conditions before and after the closure. In general, hospital closure is perceived to have negative economic effects on a rural community (Hart, Pirani, and Rosenblatt 1991a), although few studies have directly measured the effect. A number of studies have attempted to estimate the role of hospitals in their local economies as evidence of the direct and indirect impact a closure would have, by either comparing the closure communities' economies to those of control groups, or through input/output (I/O) analysis.
In one of the earliest studies, Christianson and Faulkner modeled the contribution of rural hospitals to local economies and found an estimated $686,405 to $1,083,282 (US$ in 1978) in community income was generated directly and indirectly by hospital expenditures; income multiplier estimates were less than 2 for 90 percent of the communities (Christianson and Faulkner 1981). McDermott et al. (1991) used hospital survey data to estimate the economic impact of a hospital on its host community and found that the combined induced and direct effects, on average, were $54,739 per hospital bed (1991). Studies using I/O analysis, which uses observed data on business and consumer purchase patterns to estimate the direct and indirect/induced effects of a change in one sector of the economy on others, have found similar results. For example, Doeksen, Gerald, and Altobelli (1990) simulated the effect of a hospital closure in rural Oklahoma and estimated that over a 5-year period approximately 78 jobs, $1.7 million in income, $452,100 in retail sales, and $9,100 in sales tax revenue would be lost because of the closure. Similar conclusions were reached using data from three Texas communities (Doeksen, Loewen, and Strawn 1990). Cordes et al. (1999) extended the literature by examining the role of the hospital in the economy and differentiating hospitals by bed size. They found that the estimated economic multipliers increased in magnitude with hospital bed size, but did not specifically estimate the effect of closure using I/O analysis.
While each of these studies suggests that a hospital closure would have negative economic consequences for rural communities, other research has indicated little to no effect on the rural community because of hospital closure. Pearson and Tajalli (2003) found that hospital closure does not appear to cause short- or long-term harm to the economies of their rural host communities. Their findings were based on a pretest/posttest model of data for 24 Texas rural communities where a hospital closed and a group of control communities. Five economic indicators were examined for trends and none were found to have had a statistically significant change following closure of the hospital. Similarly, Probst et al. (1999) compared economic indicators in closure communities to a control group of nonclosure communities and failed to find a statistically significant difference in income trends in the closure counties relative to the comparison counties. Stensland et al. (2002) examined the effect of 42 hospital closures in rural Appalachian communities and concluded that the closure had no effect on short-term or long-term economic growth of those areas.
Predominantly, the literature on the economic effects of hospital closures has relied on I/O analysis. Whereas I/O analysis has been useful in furthering the methodology of measuring hospital closure effects to include spending induced by the hospital business, the technique is limited in many ways. First, it is not designed to calculate “amenity” effects of a hospital closure—the absence of a local hospital may discourage retirees and businesses from moving into the community. Secondly, because of a lack of data on these small rural markets, I/O analysis for rural areas often relies on national purchasing trends, rather than local purchasing patterns, to calculate economic multipliers. Third, I/O treats the study region (often a county) as an isolated economy and tends to ignore market area considerations, which may lead to over- or under-estimation of the effects. Finally, I/O analysis does not offer measures of precision in the estimates. The concept of standard errors (SEs) is critical in ascertaining the degree of confidence one has in the results, and I/O has no such ability.
In this paper, we estimate the effect of hospital closure on the local economy using multivariate regression methods that do not require the use of a control group consisting of communities not experiencing a hospital closure. We posit that the closure of a hospital negatively affects the economic health of a community, and we extend the hospital closure literature in two new dimensions. First, we differentiate between the impact of a hospital closure in a community where another hospital remains open and closure in a community with no other proximal access to hospital services. This distinction is important because many of the ways that a closure can affect local economies, such as the amenity effect, can be mitigated by the presence of a near-by alternative hospital. Second, our analysis considers whether the economic conditions in communities where a hospital has closed can be attributed to the closure, or whether poor economic conditions preceded (and perhaps contributed to) the closure. Our methodology allows this assessment without the necessity of identifying appropriate controls, a difficult task as there may be intrinsic differences between financially struggling communities where hospitals ultimately close and those where they remain open.
METHODOLOGY
Data Sources
A variety of data sources were used for the study. Information on hospital closures was obtained from a database we have constructed and maintained that includes hospital closures from 1990 to the present. The database identified closures by reconciling information from a number of sources, including CMS's Online Survey, Certification and Reporting system (OSCAR) Provider of Service File, the HHS Office of the Inspector General (OIG), and the American Hospital Association (AHA). Closures reported in any of these sources were verified by state hospital contacts through telephone surveys. For the purpose of this study, a hospital is considered closed if short-term acute care services provided by that entity cease in a community. For example, if a hospital builds a new plant within the same zip code and relocation to the new facility does not result in interruption of services, we do not consider that event as a closure. Other sources, such OIG, concentrate more on bricks and mortar rather than a community's access to a hospital, and would consider that event to include one closure and one new opening; thus the number of hospital closures may vary dependent on the source of information.
The database contains, among other information, the name and location of the hospital, the year it closed, and information detailing the closure, when available (e.g., whether it reopened as another type of health care facility, such as a long term care hospital, or whether the building was left unoccupied by the closure). The year of closure was verified and occasionally modified to reflect the date of the hospital's final Medicare cost report. For this study, we define a hospital as rural according to the 1993 MSA status as defined by the Office of Management and Budget and we only include hospital closures that occurred in nonmetropolitan counties.
Hospital data were obtained from the AHA's annual survey of hospitals, OSCAR and Medicare Cost Reports. These files provide information on the hospital utilization, costs and revenues, staffing, total wages and salaries, and the geographic location of the hospital. We also obtain information on communities from sources such as the area resource file (ARF) and the U.S. Census Bureau. Because of data limitations, we define communities as counties. Although finer geographic measures would be preferred, economic outcome data are difficult to obtain longitudinally at the sub-county level.
The study data are longitudinal and consist of all counties for the years 1990–2000. Although some county characteristics are not available in every year, the most critical elements for our analysis are. Various measures of economic health of the county are used as dependent variables, including per-capita income (PCI), unemployment rates, the size of the labor force, and the population in the county. Each of these measures is expected to reflect the overall economic health of a community.
Measures
There are at least three ways that a hospital closure can adversely affect the economic health of the community: direct, indirect/induced, and amenity. For the purpose of this study, we define these as follows:
Direct
The closure of a hospital generates job loss. While some employees may find alternative employment within the community, other workers (especially health professionals) must depart the community to find employment. The exodus of these workers decreases the total value of goods and services produced in the community. To the extent that health professionals have incomes above the average income in the community, the average income will fall if health professionals leave. It is also possible that many of the former employees of the hospital would find employment at wages lower than those previously earned at the hospital.
Indirect and Induced
Hospitals can be major purchasers of goods and services within the community such as laundry services or construction. Thus, hospital closure has an indirect effect on community business' production and employment, which further reverberates as those businesses and their employees reduce consumption of other goods and services and other firms throughout the local economy are affected. Second, the hospital provides an incentive for nonresidents to visit the community, whether to receive treatment or to visit a patient. These individuals will likely purchase some products or services in the community during their visit (for example, a hotel room, meals, flowers).
Amenity
For some businesses and retirees, proximity to a hospital may be an important consideration in deciding where to locate, and the absence of a hospital may discourage businesses or retirees from locating in a community, retarding future economic development.
Analytic Approach
We posit that the economic health of the community can be specified as a linear function of community characteristics. In the discussion that follows, we use per-capita income as the outcome variable, but analogous models are used for the other outcomes considered.
| (1) |
where subscripts c and t denote county and time, respectively. Indicator Hct equals one if and only if county c has a hospital in time t. Xct is a vector of county characteristics. Unobservable (to the analyst) terms τt and μc allow time-specific and county-specific shocks, respectively.
Estimation of the effect of a hospital closure (i.e., when ΔHct=Hc,t−Hc,t−1=−1) is achieved by exploiting the longitudinal data structure to control for unobserved time-invariant factors affecting the economic health of the community. Operationally, we specify a fixed effects model. The parameter α is identified by variation in Hct over time within a county. That is, the model estimates the effect of hospital closure by comparing the economic health of the community before the closure with the economic health after the closure. This method is preferred to a cross-sectional approach that compares communities with hospital closures to communities without hospital closures if counties experiencing a closure are unobservedly different from those counties that did not experience a closure. One advantage of a fixed effect model is that the hospital closure indicator is allowed to be correlated with county-specific time-invariant factors (μc) unobserved by the analyst.
We allow the effect of the closure to vary based on the number of years since closure. In the index year (the year in which the hospital closes), the effect may be different from subsequent years for two reasons. First, the closure likely does not occur on January 1, so the measured economic effect will be less than that if the hospital were closed the entire year. Second, the amenity effect may not fully manifest in the first year. Operationally, we account for this by including lagged terms of the closure effect.
One concern may be that random shocks to the economic health of the community (ɛ) may adversely affect the financial viability of the hospital and lead to a hospital closure. Formally, we might expect E(H′ctɛc,t−1) ≠ 0. For example, a bad economic year in the community may induce the hospital to close in the next year. Failure to control for this may lead to spurious findings of an effect when none exists. We examine this potential bias by including an indicator for whether the hospital closes in the subsequent year. If this condition, commonly known in labor economics as an Ashenfelter Dip from Ashenfelter (1978), holds, then the parameter estimate on this indicator will be statistically significant.
We include a series of indicator variables to allow the effect of a hospital closure to vary depending on the number of years since the hospital closed. There are two types of variables. The first is a state variable that captures the overall effect of closure. This variable is positive if and only if the hospital has closed. Thus, in a county where a hospital closed in 1995, this variable is 0 until 1994 and 1 from 1995 until the end of the sample period. We also include a series of dummy variables for each year pre- and postclosure. The “short run” effect—the effect in the first couple years—is the sum of the overall closure variable with the current year. Thus, in 1996, the effect of a hospital closure is the sum of the “overall” effect and the “hospital closed last year” coefficients. We expect a negative coefficient on the “has no hospital” or “a hospital closed” variables, as the closure should negatively affect the economy. We expect a negative coefficient on the leading year indicator to capture the preclosure dip in the economy. We expect the current and lagged terms to be positive and of shrinking value as the effect of the closure is not fully realized for a couple years.
We include two measures of hospital closures. The first is an indicator for the closure of any hospital (“Number of Hospital Closures”), which captures the direct and indirect effects of the closure. The second measure indicates the closure of the only hospital (“County Has No Hospital”) in the community. This variable captures the amenity effect that the “Closure of Any Hospital” measure does not include. We specify two years of lagged effects. The model includes both year and county-specific fixed effects, though these estimates are not presented. SEs are corrected for heteroskedasticity using the White (1980) formula.
To measure further the amenity effect of a hospital closure, we calculate the proportion of the county population that is located within 15 miles of a hospital, before and after closure, using census tract estimates of population. This approach allows for cross-county effects in that the 15 mile radius is drawn irrespective of county borders. If a hospital closure reduces the proportion of the county located within 15 miles of a hospital by only 1 percentage point, the amenity effect should be small. Conversely, a hospital closure that decreases the proportion within 15 miles by 80 percentage points would be expected to have a large amenity effect.
Closure Effect
Ultimately, the goal of the paper is to estimate the difference between the observed economy of a county and the economy that would have been, absent the hospital closure. The difficulty, of course, is that the counterfactual is not observed for counties that do not experience a closure; this must be estimated. If hospital closures are not correlated with unobserved factors, then one could estimate models using, for example, a propensity-score approach as used by Probst et al. (1999). An alternative method (Stensland et al. 2002), is to use a longitudinal approach and compare the outcomes for closure counties with the outcomes of nonclosure counties (used as the estimate of the counterfactual). Although this approach is appealing in its simplicity, it could produce biased estimates if nonclosure counties are systematically different than closure counties. In preliminary analyses, we found that closure counties have a lower average per capita income throughout the study period (both preclosure and postclosure) compared with nonclosure counties. These results suggest that in our data the nonclosure counties may not be a meaningful comparison group. Therefore, we restrict our sample to those counties experiencing a closure at least once in the sample time period (1992–1998 because of the requirements of leading and lagged closure terms). In our approach, in any given year counties that eventually will experience a closure but have not yet experienced one serve as the estimate of what economy of the closure county would have been in the absence of a closure.
The final sample includes 134 counties and the economy of each county is measured at seven points in time (once per year 1992–1998); thus the total sample size is 938. The number of counties experiencing a closure in each year is presented in Table 1. The shaded rows represent the years included in the sample. The nonshaded rows are not included in the study sample per se but contribute to the estimation because closures in these years contribute to the identification of the model. That is, although 1992 is the first year included in the sample, closures in 1991 affect the estimates because the once-lagged closure term is positive for that county in 1992. Note that the total number of closures in the sample is 140 as some counties experienced multiple closures. Forty-two hospitals that were the only hospital in the county closed in the 1990–1999 period. The remaining 98 hospitals that closed were located in counties with at least one other hospital when the hospital closed. Table 2 presents the mean, minimum, and maximum values of population, per capita income, and the unemployment rate for the study sample counties in 1992. The average county had a population of 26,766, a per capita income (US$ 1990) of 14,119 and an unemployment rate of 8.12 percent. Compared with counties without a closure, at the beginning of the study period (1992) the closure counties had a larger population (not shown, p=0.02) but were statistically identical in income and unemployment rate. The geographical distribution is also presented. Most of the sample is located in the Midwest and South census regions, although the distribution of sample counties is statistically equal to the distribution of nonmetropolitan counties (not shown, p=0.13).
Table 1.
Number of Closures
| Year | Number ANY Closures | Number ONLY Closures |
|---|---|---|
| 1990 | 24 | 5 |
| 1991 | 31 | 8 |
| 1992 | 20 | 6 |
| 1993 | 16 | 7 |
| 1994 | 3 | 0 |
| 1995 | 10 | 4 |
| 1996 | 9 | 4 |
| 1997 | 8 | 3 |
| 1998 | 7 | 1 |
| 1999 | 12 | 4 |
| 1992–1998 | 73 | 25 |
| 1990–1999 | 140 | 42 |
N=134 counties.
Only years 1992–1998 (shaded) are included in the model; closures in the other years contribute due to lagged and leading terms. That is, a 1990 closure contributes to the model because in 1992 the twice-lagged term is nonzero.
Table 2.
Summary Statistics
| Variable (1992 Value) | Mean | Range |
|---|---|---|
| Population | 26,766 | (1,939, 176,452) |
| Per capita income ($1990) | 14,119 | (8,952, 22,959) |
| Unemployment rate | 8.12 | (2.70, 28.70) |
| Census region | Number in sample | |
| Midwest | 47 | |
| Northeast | 5 | |
| South | 70 | |
| West | 12 | |
| Total | 134 |
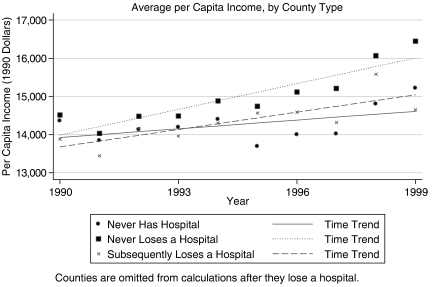
Figure 1 presents the average per capita income (adjusted to US$1990) for three groups of counties. The first group consists of counties that never had a hospital during the time period under observation. The second group is the set of counties that have hospitals but did not lose any. The third group is the set of hospitals that lose a hospital over the time frame. Counties in this group are omitted from the calculations once they lose a hospital. This implies that the any change in the averages are not caused by hospital closures. Any difference in time trend, therefore, captures underlying differences in the counties not directly caused by a hospital closure because we omit counties that experienced a closure. Note that although the average incomes are similar in 1990, counties losing a hospital have a slower rate of income growth than counties not losing a hospital. This suggests that including “nonclosure” counties as a control group may bias the estimate of the estimated effect of the closure.
Figure 1.
Mean per Capita Income and Time Trend, by County Type
RESULTS
Fixed effect regression models were estimated using various economic indicators as dependent variables (Table 3). The estimates suggest that hospital closures have a negative direct effect on the economic health of the county only if the hospital is the only hospital in the community. Model 1 shows that counties losing the only hospital in the county experience a long term decrease in real PCI of roughly $703 (in 1990 currency). The lagged term is insignificant, which indicates that the effect of the closure is fully manifested in the first year of the closure. Although this is inconsistent with the amenity hypothesis which postulates the loss of the amenity (hospital) acts as an impediment to economic growth, the pattern of the magnitudes and signs of the coefficients is consistent with a phasing in of the effect. It is possible that the addition of more data might lead to statistically significant estimates. Although not marked in the table, by dividing the coefficient by the SE and using t-statistic tables, one can see the once-lagged estimate here is significant at the 10 percent level (p=0.06). This pattern tends to hold in the models with other outcomes as well. Model 2 indicates that closure of the only hospital leads to a 4 percent decrease in PCI, again fully realized in the first year of closure. Unemployment increases by 1.6 percentage points as a result of the closure, with only about half of that effect in the year of the closure. Neither the population nor the labor force appears to be affected by the hospital closure.
Table 3.
Regression Results
| Model | (1) PCI | (2) Log(PCI) | (3) Unemployed | (4) Log(Pop) | (5) Log(Labor) |
|---|---|---|---|---|---|
| Closure of ANY hospital | |||||
| Had ANY hospital closure | 323.167 (235.101) | 0.025 (0.016) | −0.011 (0.396) | −0.007 (0.007) | 0.002 (0.014) |
| Leading and lagged terms | |||||
| Any closure in t+1 | −79.538 (141.722) | −0.006 (0.009) | 0.000 (0.209) | 0.001 (0.004) | 0.001 (0.010) |
| Any closure in t | −270.827* (129.525) | −0.017* (0.008) | −0.129 (0.262) | −0.006 (0.006) | −0.005 (0.009) |
| Any closure in t−1 | −278.276* (119.209) | −0.017* (0.008) | −0.151 (0.239) | −0.003 (0.004) | −0.004 (0.008) |
| Any closure in t−2 | −203.355* (98.105) | −0.013* (0.006) | 0.004 (0.181) | −0.001 (0.003) | −0.005 (0.006) |
| Closure of ONLY hospital | |||||
| County has no hospital | −702.670* (290.032) | −0.040* (0.020) | 1.615** (0.510) | 0.003 (0.010) | −0.021 (0.020) |
| Leading and lagged terms | |||||
| Sole closure in t+1 | 323.167 (235.101 | 0.025 (0.016) | −0.011 (0.396) | −0.007 (0.007) | 0.002 (0.014) |
| Sole closure in t | 681.266** (189.553) | 0.043** (0.013) | −0.874* (0.425) | −0.006 (0.009) | 0.035* (0.016) |
| Sole closure in t−1 | 445.511 (241.013) | 0.027 (0.017) | −0.262 (0.423) | −0.005 (0.007) | −0.004 (0.023) |
| Sole closure in t−2 | 295.916 (244.821) | 0.019 (0.017) | −0.445 (0.292) | −0.001 (0.006) | 0.005 (0.014) |
| Constant | 14,196.278** (154.176) | 9.551** (0.010) | 6.090** (0.282) | 9.839** (0.004) | 9.100** (0.009) |
| Observations | 938 | 938 | 938 | 938 | 938 |
| R2 | 0.92 | 0.93 | 0.88 | 1.00 | 1.00 |
Significant at 5%.
Significant at 1%.
Estimated White (1980) standard errors in parentheses.
Year and county fixed effects also included but not listed here.
Overall, while the loss of the sole hospital imparts a significant negative effect on the county economy, there is little evidence that a hospital closure when another institution remains open affects the county's economy in the long run. Income (whether measured in levels or logs) does diminish with the closure of any hospital, but again the pattern (as well as the insignificance on the “Had ANY Hospital Closure” variable) suggests that the effect is short-lived. Indeed, in models in which we use three lagged terms, the third lag was statistically insignificant.
It is instructive to compare our results to estimates from I/O models. Recall that I/O models contain no uncertainty measures, so it is difficult to compare the models statistically. Furthermore, I/O models use aggregate measures (total income of the community) while we are using average measures (PCI). A quick back-of-the-envelope comparison is instructive, however. Doeksen, Loewen, and Strawn (1990) estimate a decrease of $901,400 in income for the year following closure. Assuming that population is unchanged during that year, this decrease translates (using their county) to a 0.8 percent change in income compared with our estimate of 0.5 percent (computed as 0.025 − 0.017 − 0.040 + 0.027 = 0.5 for the Log(PCI) model in Table 3). Given the different approaches, the similarity in our findings is striking.
As mentioned previously, we explore an alternative measure of the economic impact of hospital closures by calculating the proportion of a county's population that resides within 15 miles of an operating short-term general hospital. This method helps compensate for some of the specificity lost by our inability to construct models at the community-, rather than county-level.
GIS software allows the drawing of 15-mile-radius circles around a hospital; these circles are then mapped onto census tracts to estimate the proportion of county population located within 15 miles of a hospital. We estimate population-weighted measures at the census tract level, using the 2000 census, to provide a more appropriate estimate of “hospital coverage.” The closure of a hospital serving much of a county's land area but a small proportion of the population may have less effect than the closure of a hospital serving a small land area but a large population. We use the population measure as the treatment variable in the regressions in this subsection, although the area-weighted measure yielded similar but slightly less significant results. This class of models is comparable with those of the previous subsection in simplicity, but uses a continuous measure of hospital closure rather than a simple dichotomous measure. Table 4 presents the results of these models. The anticipated sign is opposite that of the previous models; an increase in the proportion of a county served by a hospital should increase the economic health of the community.
Table 4.
Radii Measures
| Model Variable | (6) PCI | (7) Log(PCI) | (8) Unemployed | (9) Log(Pop) | (10) Log(Labor) |
|---|---|---|---|---|---|
| Pct of population within 15 miles of hospital | 1,299.8632 (403.76)** | 0.0869** (0.03) | −3.0812** (0.74) | 0.0108 (0.02) | 0.0748* (0.04) |
| Leading and lagged terms | |||||
| Change in population within 15 miles of hospital in t+1 | −988.2268** (357.41) | −0.0624* (0.02) | 1.4454* (0.70) | 0.0076 (0.01) | −0.0426 (0.04) |
| Change in population within 15 miles of hospital in t | 82.7858 (210.75) | 0.0047 (0.01) | −0.9063* (0.41) | 0.0135 (0.01) | 0.0062 (0.01) |
| Change in population within 15 miles of hospital in t−1 | −769.3062* (370.98) | −0.0528 (0.03) | 0.7791 (0.58) | 0.0005 (0.01) | −0.0283 (0.03) |
| Change in population within 15 miles of hospital in t−2 | −774.8735* (318.76) | −0.0520* (0.02) | 0.7208 (0.47) | −0.0047 (0.01) | −0.0118 (0.02) |
| Constant | 13,012.5105** (333.69) | 9.4689** (0.02) | 10.6298** (0.66) | 9.8078** (0.01) | 8.9770** (0.03) |
| Observations | 938 | 938 | 938 | 938 | 938 |
| R2 | 0.92 | 0.93 | 0.88 | 1.00 | 1.00 |
Significant at 5%.
Significant at 1%.
Estimated White (1980) standard errors in parentheses.
Year and county fixed effects also included but not listed here.
In general, results match our expectations. A 10 percent decrease in the coverage of a county (about half the average change for a county losing its sole hospital) leads to a $130 (or about 0.9 percent as estimated by the model with log PCI) decrease in per capita income, and a 0.3 percent point increase in the unemployment rate. The leading terms here are statistically significant, suggesting that a negative shock to the unemployment rate of a county may be associated with future closures. What is noteworthy in these results is that even when using a completely different metric of hospital closure we find statistically significant effects of the anticipated sign. Although the magnitudes are slightly smaller, this is not surprising because our radii measure is a “noisy” estimate of the true coverage of the hospital. Thus, these models provide additional support for our main finding that a closure of the sole hospital affects the economy of the county.
CONCLUSION AND POLICY IMPLICATIONS
Although we find that a hospital closure per se does not negatively affect the long-run economic health of a community, losing the sole hospital in the county results in a considerable negative effect on the economy. We account for endogenous closure by including leading terms of closures and find little evidence of an Ashenfelter Dip; this may be because of our careful construction of a control group. Although there are no guarantees that it is the hospital closure per se that led to the economic decline of the county, our estimates reconcile with previous work and seem reasonable.
The results presented here suggest that the closure of a rural county's sole hospital decreases the economic well-being of the community and likely places the local economy in a downward cycle that may be very difficult to recover from. This effect was not only statistically significant but policy significant as well. For example, we estimate a long run decrease in the per capita income of 1.5 percent. The finding that the economic impact is an issue in communities where the sole hospital closed, an event that would almost always occur in rural areas, suggests important considerations for policy makers involved with hospital regulation. The traditional charge of health care regulators has been to increase economic efficiency, which places a particularly acute financial pressure on small rural hospitals. Because of low volumes it is difficult for these facilities to manage profitability under fixed reimbursement systems such as Medicare's PPS, as they experience significantly greater variability in inpatient demand across years, with a resultant instability in average costs per discharge (Dalton, Holmes, and Slifkin 2003a, b).
Thus, regulations imposed to increase hospital efficiency may have spillover effects; the economy is affected if the regulations induce the hospital to close. These economic effects, of course, compound any negative effects on health and health care access in rural communities because of the closure. Assessments of the impact of hospital closure have found that closures have created barriers to receipt of crucial emergency services (Reif, Des Harnais, and Bernard 1999), increased travel time to inpatient care with substantial effect on outcomes in the case of certain clinical conditions (Fleming et al. 1995; Reif, Des Harnais, and Bernard 1999), and resulted in decreased utilization (Rosenbach and Dayhoff 1995) and a loss of access to a proximate source of primary health care (Bindman et al. 1990). Combined with the decrease in physician supply because of hospital closure (Hart, Pirani, and Rosenblatt 1991b) and the economic downturn demonstrated in this paper, access to primary health care would likely continue to decrease.
It should be noted, however, that the closure of a hospital is not a random event. Hospitals that closed tend to have had a small number of beds, low volumes, were in poor financial condition, and had for-profit ownership (McKay and Coventry 1995; Rosenbach and Dayhoff 1995). It is reasonable to ask whether hospitals that close because of low volumes are necessary providers that simply cannot compete in a market system because they serve a small population base, or are providers that are not utilized by their communities, and so are appropriately closed. To the extent that the latter is true, one perspective is that a hospital closure, while painful for a community, is the market's mechanism for enforcing minimum quality standards. There is, however, almost no evidence regarding the quality of care in hospitals that have closed, just as there is almost no research on quality of care in small rural hospitals generally (IOM 2005). One study that interviewed physicians in closure communities found that over three-quarters of those interviewed felt that the quality of care in the closed hospital was average or better (Pirani et al. 1993).
Although it was beyond the scope of our analysis to examine the quality of the hospitals that closed, consideration of the potential role of quality in these hospital closures allows for discussion of appropriate policies to protect health care access in rural America. Policy makers have shown that they are willing to accept a certain degree of inefficiency and/or economic risk, such as that associated with the Critical Access Hospital designation, in order to avoid the negative spiral associated with a hospital closure. In the absence of empirical work, one can make the assumption that the universe of closed hospitals includes both high-quality institutions with an insufficient population base in their community to be able to financially survive, as well as institutions that were underutilized by their community because of perceptions of low quality. It would be difficult, if not impossible, to create reimbursement policy that helped sustain all necessary providers with adequate quality of care, while allowing those of low quality to close. An implicit choice when designing reimbursment policy is whether it is preferable to preserve access for as many rural communities as possible, recognizing that some institutions will be kept open that possibly should have closed, or whether it is preferable to allow the market to dictate closure of low quality institution, knowing that some hospitals with adequate or better quality will also close because of the financial realities of operating in a sparsely populated area.
Factors that are associated with closures, such as quality concerns, can also be addressed by policy makers. Consistent with national quality improvement efforts, the CAH enabling legislation also created the medicare rural hospital flexibility program, which supports quality initiatives in rural hospitals by requiring CAHs to have a credential and quality assurance mechanism and state certification before conversion, as well as provides funds for quality-related activities (Casey and Moscovice 2004). The linking of the financial protection of cost-based reimbursement with a program to improve quality of care shows recognition of both the importance of small hospital survival to rural communities as well as the need to provide support for improvement in services. The findings from this analysis support the continuation of such initiatives.
Acknowledgments
This research was funded by the Federal Office of Rural Health Policy, cooperative agreement #6U1CRH00027-03. All opinions expressed here are those of the authors and are not necessarily those of ORHP. Helpful comments provided by participants at the 2003 National Rural Health Association and Southern Economic Association annual meetings and the Sheps Center Work in Progress Lunch, two anonymous referees, and Catherine McLaughlin. All remaining errors are, of course, our own.
REFERENCES
- Ashenfelter O. “Estimating the Effect of Training Programs on Earnings.”. Review of Economics and Statistics. 1978;60:47–57. [Google Scholar]
- Bindman AB, Keane D, Lurie N. “A Public Hospital Closes: Impact on Patients' Access to Care and Health Status.”. Journal of the American Medical Association. 1990;264((22)):2899–904. doi: 10.1001/jama.264.22.2899. [DOI] [PubMed] [Google Scholar]
- Casey MM, Moscovice I. “Quality Improvement Strategies and Best Practices in Critical Access Hospitals.”. Journal of Rural Health. 2004;20((4)):327–34. doi: 10.1111/j.1748-0361.2004.tb00046.x. [DOI] [PubMed] [Google Scholar]
- Christianson JB, Faulkner L. “The Contribution of Rural Hospitals to Local Economies.”. Inquiry. 1981;18:46–60. [PubMed] [Google Scholar]
- Cordes S, Van der Sluis E, Lamphear C, Hoffman J. “Rural Hospitals and the Local Economy: A Needed Extension and Refinement of Existing Empirical Research.”. Journal of Rural Health. 1999;15((2)):189–201. doi: 10.1111/j.1748-0361.1999.tb00739.x. [DOI] [PubMed] [Google Scholar]
- Dalton KD, Holmes GM, Slifkin RT. “Unstable Demand and Cost per Case in Low-Volume Hospitals.”. 2003a. NC Rural Health Research and Policy Analysis Center Findings Brief.
- Dalton KD. “Unpredictable Demand and Low-Volume Hospitals.”. 2003b. NC Rural Health Research and Policy Analysis Center Findings Brief.
- Doekson GA, Altobelli J. The University of North Dakota Rural Health Research Center; 1990. “The Economic Impact of Rural Hospital Closure: A Community Simulation.”. [Google Scholar]
- Doeksen GA, Johnson T, Willoughby C. Mississippi State University, Southern Rural Development Center; 1997. “Measuring the Economic Importance of the Health Sector on a Local Economy: A Brief Literature Review and Procedures to Measure Local Impacts.”. SRDC 202. [Google Scholar]
- Doeksen GA, Loewen RA, Strawn DA. “A Rural Hospital's Impact on a Community's Economic Health.”. Journal of Rural Health. 1990;6((1)):53–64. doi: 10.1111/j.1748-0361.1990.tb00190.x. [DOI] [PubMed] [Google Scholar]
- Doelker RE, Bedics BC. “Impact of Rural Hospital Closings on the Community”. Social Work. 2001;(November 1989):541–3. [PubMed] [Google Scholar]
- Fleming ST, Williamson HA, Jr, Hicks LL, Rife I. “Rural Hospital Closures and Access to Services.”. Hospitals and Health Services Administration. 1995;40((2)):247–62. [PubMed] [Google Scholar]
- Flex Monitoring Team. “Implementation Status by State”. [February 23];2005 Available at http://www.flexmonitoring.org/surveygrid.
- Hart GL, Pirani MJ, Rosenblatt RA. “Rural Hospital Closure and Local Physician Supply.”. Journal of Rural Health. 1991a;7((3)):222–45. doi: 10.1111/j.1748-0361.1991.tb00725.x. [DOI] [PubMed] [Google Scholar]
- Hart GL, Pirani MJ, Rosenblatt RA. “Causes and Consequences of Rural Small Hospital Closures from the Perspective of Mayors.”. Journal of Rural Health. 1991b;7((3)):222–45. doi: 10.1111/j.1748-0361.1991.tb00725.x. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine of the National Academies. Quality through Collaboration: The Future of Rural Health. Washington, DC: The National Academy Press; 2005. [Google Scholar]
- McDermott RE, Cornia GC, Parsons RJ. “The Economic Impact of Hospitals in Rural Communities.”. Journal of Rural Health. 1991;7((2)):117–132. doi: 10.1111/j.1748-0361.1991.tb00714.x. [DOI] [PubMed] [Google Scholar]
- McKay NL, Coventry JA. “Access Implications of Rural Hospitals Closures and Conversions.”. Hospitals and Health Services Administration. 1995;40((2)):227–46. [PubMed] [Google Scholar]
- Medicare Payment Advisory Committee. Washington, DC: 2003. [on March 4, 2005]. “Public Meeting.”; p. 231. 12/04/2003, Available at http://www.medpac.gov. [Google Scholar]
- Pirani MJ, Hart LG, Rosenblatt RA. “Physician Perspectives on the Causes of Rural Hospital Closure.”. Journal of the American Board of Family Practice. 1993;6((6)):556–562. [PubMed] [Google Scholar]
- Pearson DR, Tajalli H. “The Impact of Hospital Closure on the Economic Health of the Local Communities.”. Texas Journal of Rural Health. 2003;21((3)):46–51. [Google Scholar]
- Probst JC, Samuels ME, Hussey JR, Berry DE, Ricketts TC. “Economic Impact of Hospital Closure on Small Rural Counties,1984 to 1988: Demonstration of a Comparative Approach.”. Journal of Rural Health. 1999;15((4)):375–88. doi: 10.1111/j.1748-0361.1999.tb00761.x. [DOI] [PubMed] [Google Scholar]
- Reif SS, Des Harnais S, Bernard S. “Community Perceptions of the Effects of Rural Hospital Closure on Access to Care.”. Journal of Rural Health. 1999 Spring;15((2)):202–9. doi: 10.1111/j.1748-0361.1999.tb00740.x. [DOI] [PubMed] [Google Scholar]
- Rosenbach ML, Dayhoff DA. “Access to Care in Rural America: Impact of Hospital Closures.”. Health Care Financing Review. 1995;17((1)):15–37. [PMC free article] [PubMed] [Google Scholar]
- Stensland J, Mueller C, Sutton J. Washington, DC: 2002. “An Analysis of the Financial Conditions of Health Care Institutions in the Appalachian Region and Their Economic Impacts.”. Final Report to the Appalachian Regional Commission. [Google Scholar]