Abstract
Objectives
To analyze vulnerability as a profile of multiple risk factors for poor pediatric care based on race/ethnicity, poverty status, parent education, insurance, and language. Profiles are used to examine disparities in child/adolescent health status and primary care experience.
Data Sources
Cross-sectional data on 19,485 children/adolescents 0–19 years of age from the 2001 California Health Interview Survey.
Study Design
Multiple logistic regression models are used to examine risk profiles in relation to health status and three aspects of primary care: access (physician and dental visit; access surety), continuity (regular source of care), and comprehensiveness (i.e., health promotion counseling).
Principal Findings
About 43 percent of (or 4.4 million) children in California have two or more risk factors (RF). Controlling for age and gender, more RFs is associated with poorer health status (i.e. percent reporting “excellent/very good” health: no RFs=81 percent, 1=71 percent, 2=57 percent, 3=45 percent, 4=35 percent, 5=28 percent, all p<.001). Controlling for health status, higher risk profiles is associated with poorer primary care access and continuity, but greater comprehensiveness of care. For example, higher risk profile children are less likely to have a regular source of care: one RF (prevalence ratio [PR]=0.92, confidence interval [CI]: 0.86–0.98), two (PR=0.77, CI: 0.69–0.84), three (PR=0.55, CI: 0.46–0.65), and four or more (PR=0.31, CI: 0.22–0.44), all p<.001.
Conclusions
This study demonstrates a dose–response relationship of higher risk profiles with poorer child health status, access to, and continuity of primary care. Having gained access, however, adolescents with higher risk profiles are more likely to receive health promotion counseling. Higher profiles appear to be associated with greater barriers to accessing primary care for children in “fair or poor” health, suggesting that vulnerable children who have the greatest health care needs also have the greatest difficulty obtaining primary care.
Keywords: Children, primary care, health care quality, access to care, health disparities
Primary care is a cornerstone of the U.S. child health system (Donaldson et al. 1996; Starfield 1998). While many definitions of primary care exist, there is a general consensus on at least four defining features to assess its performance: accessibility, continuity, comprehensiveness, and coordination (Starfield 1994). As the receipt of high quality primary care has been associated with improved health (e.g., lower morbidity and mortality) (Lurie et al. 1984; Franks and Fiscella 1988; Shi 1994; Chande and Kinnane 1996; Safran et al. 1998; Shi, Green, and Kazakova 2004), and lower health care costs (e.g., fewer hospitalizations and emergency visits) (Bindman et al. 1995; Blumenthal, Mort, and Edwards 1995; Forrest and Starfield 1996; Gill, Mainous, and Nsereko 2000; Christakis et al. 2001), it is a major focus of national aims to reduce disparities and improve child health outcomes (U.S. Department of Health and Human Services 2000).
Despite its value, many children do not receive adequate primary care. Children in lower socioeconomic status (SES) families, the uninsured, and racial/ethnic minorities frequently have been reported to have poorer primary care experiences (Newacheck, Hughes, and Stoddard 1996; Ortega et al. 2000; Weech-Maldonado et al. 2001; Newacheck et al. 1998, 2002; Stevens and Shi 2002; Elster et al. 2003; Lurie et al. 2003; Seid, Stevens, and Varni 2003), and poorer health status (Montgomery, Kiely, and Pappas 1996; Brooks-Gunn and Duncan 1997; Lave et al. 1998; Goodman 1999; Flores et al. 1999; DiLiberti 2000; Holl et al. 2000; Bradley and Corwyn 2002; Wood et al. 2002; Fox et al. 2003; Newacheck et al. 2003). Given weakening state budgets across the nation, access to needed high quality primary care for these vulnerable children may be further compromised. Public health insurance and public health care delivery programs that provide essential primary care services to many children—and account for nearly one-third of the state budget in California—continue to teeter on the edge of the political chopping block, threatening the viability of these safety-net programs for children. Children in noncitizen families and those residing in rural areas (both prominent issues in California) are at even higher risk for poor primary care, as even safety-net delivery programs often overlook rural areas and noncitizens are generally excluded from state insurance programs (Inkelas et al. 2003).
Children served by public programs are considered vulnerable because they frequently have multiple risk factors for poor health status and poor primary care (e.g., living in poverty and not having health insurance) (Aday 2001). Previous research on child health and health care disparities has primarily focused on identifying and delineating the individual effects of these risk factors. Such an approach is important to identify new relationships and derive causal mechanisms, and forms the basis of most of our understanding of child health disparities.
Since risk factors often cluster together, however, e.g., parents who did not graduate high school (one risk), are more likely to work in low-wage jobs (a second risk) and not have health insurance (a third risk)—understanding how multiple risk factors combine to influence primary care is an important next step. One alternate approach builds on existing knowledge to describe individuals according to risk profiles that allow the reader to explore the influence of multiple risk factors in a more explicit and interpretable way (Shi and Stevens 2005).
Previous studies that have used this risk profile technique have shown that vulnerability to poor health is not defined by a single demographic, social, behavioral, or financial risk. In many instances, poor health outcomes have been associated with the multiplicity of risk factors a child or adolescent has. Sameroff et al. (1987) have shown an additive association between the number of family risk factors (e.g., minority status, low maternal education, poor maternal mental health) and child social-emotional health and IQ. Furstenberg et al. (1999) has demonstrated that family factors (e.g., single-parenting), community risks (e.g., neighborhood safety), and peer influences (e.g., antisocial peers) combine to influence adolescent social health and performance in school. More recent studies by Starfield, Robertson, and Riley have also combined both parent education and employment status to reveal an association between higher social class and child health status (Starfield, Robertson, and Riley 2002; Starfield et al. 2002).
Single risk factor focused assessments have some limitations in informing interventions, since they may tend to lead to more narrowly focused approaches to resolving disparities rather than more integrated, multisector interventions to improving child health. Understanding how risk factors combine to influence child health status and primary care and how such risk profiles are distributed in the population may provide better guidance in where to intervene to achieve the greatest results. Few studies assess how combinations of risk factors are distributed in the child population, and those few studies mentioned do not explicitly examine the combined influences of risk factors on disparities in child health status or primary care (Shi and Stevens 2005).
Understanding vulnerability in terms of multiple, overlapping risk factors for inadequate primary care is an important next step. Policy makers and those charged with monitoring access to care for vulnerable children might benefit from using this multiple risk factor approach to identify children who have the greatest health care needs and are least likely to obtain care. Even though more complex statistical techniques are available to describe the combined influences of multiple risk factors (i.e., multiple interaction terms), they create challenges in interpretation for policymakers. A more straightforward assessment of child vulnerability using risk profiles, particularly when combined with detailed analyses of the various common combinations, may help to better guide the allocation of resources, interventions, or outreach to improve the delivery of primary care at the population, health plan, or individual clinic level.
This study uses data on children and adolescents ages 0–19 from the 2001 California Health Interview Survey (CHIS) to construct a vulnerability risk profile for each child based on five factors: child race/ethnicity, household poverty status, parent education, health insurance coverage, and primary language. The prevalence of these profiles is presented overall and then according to two family factors (immigration status and geographic residence) that have been the focus of recent policy debates about access to care in California, including new legislation to cover all children regardless of immigration status through expansions of county-based health insurance programs into geographic areas with high rates of uninsurance. The profiles are used to examine disparities in child health status and three aspects of primary care (i.e., access, continuity, and comprehensiveness of care). To provide the most policy-relevant results, the relationship of risk profiles with primary care access is examined by child health status (i.e., health need).
METHODS
Study Design and Sampling
This study analyzes data on 19,485 children and adolescents (ages 0–19) from the state-representative 2001 CHIS, conducted by the UCLA Center for Health Policy Research in collaboration with the California Department of Health Services, and the Public Health Institute. The CHIS was completed with about 55,000 randomly selected households drawn from each county in California. In each household, one adult was randomly selected for interview. In households with children, the CHIS also interviewed one adolescent age 12–17, and obtained information for one child under age 12 by interviewing the adult who was most knowledgeable about the child. Telephone interviews were conducted between November 2000 and October 2001 in six languages: English, Spanish, Chinese (Mandarin and Cantonese dialects), Vietnamese, Korean, and Khmer (Cambodian). Response rates are reported for adults (37.7 percent), children (33 percent), and adolescents (23.9 percent) and are calculated as the product of the screener completion rate (59.2 percent), adult interview completion rate (63.7 percent), and the child and adolescent interview completion rates (87.6 and 63.5 percent, respectively). More information on the design of CHIS is available online (www.chis.ucla.edu). The study was approved by the UCLA Center for Health Policy Research and the Office for Protection of Research Subjects.
Conceptual Framework
Five risk factors were identified from the literature as the strongest and most consistent predictors of poor primary care, and were included in the vulnerability risk profile. Risk factors included minority child race/ethnicity, household income less 200 percent of poverty, parent education of less than high school, child uninsurance, and non-English language spoken at home. Selection of these risk factors was informed by a heuristic model developed by Stevens and Shi (2003) reviewing demographic, SES, cultural, and health care system correlates of poor pediatric primary care. Except for race/ethnicity, the risk factors in this study reflect primarily SES and cultural factors amenable to policy intervention for improving primary care for vulnerable children.
Household income and health insurance coverage reflect financial resources that enable the attainment of primary care services, while education reflects a health or health care literacy level needed to navigate obtaining health services. Not speaking English (a cultural factor) is a communication barrier to accessing health services if linguistically appropriate services are not available. Language barriers may create particular difficulties in accessing and/or developing a relationship with a provider and receiving comprehensive care (e.g., preventive counseling). Race and ethnicity in this study does not imply any biological disadvantage, and is used in most other studies as a proxy for factors such as SES or language (LaVeist 1994). As SES and language are included in this analysis, race/ethnicity may reflect barriers related to the experience of bias in the receipt of health care services, cultural differences in care seeking, or other factors not in this study (Smedley, Stith, and Nelson 2002).
The selected vulnerability risk factors are hypothesized to be both independently and additively associated with reduced health status and poorer primary care access, continuity, and comprehensiveness. As vulnerable children experience a “double jeopardy” in that they have poorer health and poorer access to health care (Starfield 1982; Parker, Greer, and Zuckerman 1988), we hypothesize that the risk factors in this study may pose greater barriers to accessing needed primary care for children in “fair or poor” health than for children in “excellent or very good” health.
Measures
The study independent variables are child race/ethnicity, household poverty status, parent education, health insurance coverage, and primary language spoken at home. Race/ethnicity was self-reported and coded as White, African-American, Asian/Pacific Islander, Latino, and “other.” Family income was analyzed categorically as a percentage of the Federal Poverty Level (FPL), less than 100 percent FPL, 100–199 percent FPL, 200–299 percent FPL, and 300 percent+FPL—based on family size and household income. Education of the adult respondent (i.e., the person most knowledgeable about the child—the parent in 87 percent of cases) was coded as less than high school, high school graduate, some college, or college degree or higher. Adolescents ages 18 and 19 self-reported educational level. Child health insurance was coded as private employer-based, Medicaid, Healthy Families or rather the California's State Children's Health Insurance Program (SCHIP), other coverage, or uninsured. Language spoken at home was based on the adult respondent for children ages 0–11 and based on adolescent self-report for ages 12–19. Responses are dichotomized (any English versus non-English) dependent on whether English was at least one of the languages reported.
The categories selected as risk factors are minority race/ethnicity, household income of less 200 percent of poverty, parent education less than high school, child uninsurance, and non-English language spoken at home. These independent risk factors are also combined into a vulnerability risk profile accounting for the combined influence of co-occurring or multiple risk factors. This profile counts the number of co-occurring risk factors, such that a child who is uninsured, has a household income less than 200 percent of the FPL, and has a responding parent with less than a high school education, would have a vulnerability risk profile of three risks. A child/adolescent with none of these risk factors is considered to have a risk profile of zero.
Differential weighting of the risk factors in the risk profile scale was considered, but not done because without prior knowledge from existing research about the relative, simultaneous contributions to the given outcomes of each of the risk factors that we include in our study, we would have to weight the risk profile scale based on our own analyses, which runs the potential for over-fitting the scale to our specific data, potentially biasing the results. The results of this study, however, could serve to weight the factors within risk profiles in future analyses.
The study dependent variables reflect three aspects of primary care: (1) access to care, (2) continuity, and (3) comprehensiveness of care. Accessibility is measured by both the report of a physician visit and dental visit in the past year. For adolescents, accessibility is further assessed through one question in CHIS about self-reported “surety” in accessing health care (i.e., “How sure are you that you can access health care when you need it?”). Responses are dichotomized as “very/somewhat sure” versus “somewhat unsure/not at all sure.”Continuity of care is measured by reporting a regular source of care, defined as a “health care source (your child/you) usually visit(s) if sick or if advice is needed about (his or her/your) health.” Children seeking care from emergency departments were considered to not have a regular source.
Comprehensiveness is assessed in CHIS for adolescents ages 12–17 who reported having routine physical exam or check-up in the past year. It is measured by the self-reported receipt of physician counseling at the last check-up on eight health promotion topics that are recommended for adolescent counseling by Bright Futures and the American Academy of Pediatrics (AAP) (American Academy of Pediatrics Committee on Psychosocial Aspects of Child and Family Health 1997; Green and Palfrey 2000). Counseling topics include sexually transmitted diseases (STDs), emotions or moods, cigarette smoking, alcohol use, marijuana use, wearing bicycle helmets, car seatbelt use, and violence.
Health status is reported by the most knowledgeable adult for children ages 0–11 and self-reported by adolescents ages 12–19. It is assessed using a standard five-category Likert-type response scale of “excellent, very good, good, fair, or poor.” Health status is used as a dependent variable in most analyses in this study, and the responses are dichotomized as “excellent or very good” versus “good, fair, or poor.” When health status is used for stratification, the response category of “good” is dropped leaving the categories: “excellent or very good” versus “fair or poor.”
Covariates include child age (in years), gender, immigration status (child and parents are both citizens, child is a citizen and parents are noncitizens, and both child and parents are noncitizens), and geographic residence (urban, second city, suburban, small town, and rural).
Analysis
Analyses were performed using survey procedures in STATA 8.0 to account for the complex sampling design of the 2001 CHIS and to weight the estimates to be representative of children/adolescents (ages 0–19) in California. Since odds ratios may overestimate relationships when an outcome is common in a population, prevalence ratios (PR) (i.e., a form of relative risks for cross-sectional analyses) with 95 percent confidence intervals (CI) are used for all regressions (Zhang and Yu 1998).
First, frequencies of risk factors and the vulnerability risk profiles are presented by age group (children ages 0–11, adolescents 12–19) and for the total sample (Table 1). Second, the distribution (percentages and standard errors) of risk profiles is examined by two other family characteristics (i.e., immigration status and geographic residence) that have been the focus of recent discussions of access to care and have particular relevance in California (Table 2). Chi-square tests of association were used to assess the statistical significance of the correlation between the family characteristics and the risk profiles.
Table 1.
Frequency of Vulnerability Risk Factors and Risk Profiles
| % (SE) | |||
|---|---|---|---|
| Risk Factors | Children 0–11, (N=12,592) | Adolescents 12–19, (N=6,893) | Total 0–19, (N=19,485) |
| Child race/ethnicity | |||
| African American Ω | 6.7 (0.003) | 6.6 (0.005) | 6.6 (0.003) |
| Asian/Pacific Islander (Ω) | 9.6 (0.004) | 10.2 (0.006) | 9.8 (0.003) |
| Latino (Ω) | 37.7 (0.006) | 35.6 (0.009) | 36.9 (0.005) |
| Other (Ω) | 3.0 (0.002) | 4.9 (0.004) | 3.7 (0.002) |
| White | 43.1 (0.006) | 42.7 (0.008) | 43.0 (0.005) |
| Poverty status | |||
| Less than 100% FPL (Ω) | 23.0 (0.006) | 23.9 (0.008) | 23.4 (0.005) |
| 100–199% of FPL (Ω) | 22.9 (0.006) | 22.1 (0.008) | 22.6 (0.004) |
| 200–299% of FPL | 15.1 (0.004) | 14.4 (0.006) | 14.8 (0.004) |
| 300% FPL or higher | 38.9 (0.006) | 39.7 (0.008) | 39.2 (0.005) |
| Child health insurance | |||
| Private insurance | 57.9 (0.007) | 56.1 (0.009) | 57.2 (0.005) |
| Medicaid | 24.6 (0.006) | 19.5 (0.008) | 22.6 (0.004) |
| Healthy families | 4.9 (0.003) | 3.7 (0.003) | 4.5 (0.002) |
| Other insurance | 4.0 (0.002) | 5.5 (0.004) | 4.6 (0.002) |
| Uninsured (Ω) | 8.6 (0.003) | 15.1 (0.007) | 11.1 (0.003) |
| Educational level* | |||
| < High school (Ω) | 23.2 (0.006) | 25.3 (0.008) | 23.9 (0.005) |
| High school graduate | 25.4 (0.006) | 31.1 (0.008) | 27.6 (0.005) |
| Some college | 24.2 (0.005) | 23.8 (0.007) | 24.0 (0.004) |
| College graduate | 27.2 (0.005) | 19.7 (0.006) | 24.3 (0.004) |
| Non-English language Ω | 13.0 (0.004) | 7.9 (0.005) | 11.0 (0.003) |
| Risk profile (risk factors) | |||
| 0 | 30.8 (0.006) | 29.6 (0.008) | 30.4 (0.005) |
| 1 | 26.0 (0.006) | 27.3 (0.008) | 26.6 (0.005) |
| 2 | 18.5 (0.005) | 27.8 (0.007) | 22.1 (0.005) |
| 3 | 14.9 (0.004) | 11.5 (0.006) | 13.6 (0.004) |
| 4 | 8.1 (0.003) | 3.2 (0.005) | 6.2 (0.004) |
| 5 | 1.5 (0.003) | 0.5 (0.003) | 1.1 (0.003) |
Note: Categories of the independent measures that are considered risk factors are marked by (Ω).
Educational level is of the adult respondent for children/adolescents 0–17 years of age, and of the adolescent for those 18–19 years.
FPL, federal poverty level; SE, standard error.
Table 2.
The Distribution of Vulnerability Risk Profiles by Family Immigration Status and Geographic Residence for Children/Adolescents Ages 0–19 (n=19,485)
| Risk Profiles (RF) % SE | ||||||
|---|---|---|---|---|---|---|
| Family Characteristics | 0 | 1 | 2 | 3 | 4 | 5 |
| Immigration status* | ||||||
| Child and parent citizens | 40.0 (0.03) | 31.0 (0.03) | 18.8 (0.02) | 8.0 (0.01) | 2.0 (0.01) | 0.6 (0.01) |
| Child citizen, parent noncitizen | 3.6 (0.01) | 11.1 (0.02) | 21.0 (0.02) | 38.9 (0.03) | 21.8 (0.02) | 3.5 (0.01) |
| Child and parent noncitizens | 3.3 (0.01) | 10.0 (0.01) | 18.4 (0.02) | 31.4 (0.03) | 27.8 (0.03) | 9.1 (0.01) |
| Geographic residence* | ||||||
| Urban | 17.0 (0.02) | 23.1 (0.02) | 25.5 (0.02) | 21.3 (0.02) | 11.4 (0.02) | 1.7 (0.01) |
| Second city | 37.5 (0.03) | 25.0 (0.02) | 15.7 (0.01) | 14.3 (0.01) | 5.9 (0.01) | 1.6 (0.01) |
| Suburban | 42.5 (0.04) | 30.8 (0.03) | 12.7 (0.01) | 9.8 (0.01) | 3.7 (0.01) | 0.5 (0.01) |
| Small town | 44.6 (0.04) | 26.3 (0.02) | 17.0 (0.02) | 7.6 (0.01) | 3.6 (0.01) | 1.1 (0.01) |
| Rural | 22.1 (0.02) | 22.3 (0.02) | 20.3 (0.02) | 20.2 (0.02) | 12.2 (0.01) | 2.9 (0.01) |
p<.001 for overall χ2 of the family characteristic with the risk profiles.
RF, risk factor(s); SE, standard error.
Third, the independent association of the individual risk factors with health status and primary care access and continuity (Table 3) are presented with multivariate logistic regression for the total sample. Dummy variables for “risk” categories of the independent variables were entered in logistic multivariate models, additionally controlling for age and gender. For analyses of primary care access and continuity, the logistic models controlled for health status.
Table 3.
The Independent Relationship of Risk Factors with Health Status, and Primary Care Access and Continuity for Children/Adolescents Ages 0–19 (n=19,485)
| PR (CI) | |||||
|---|---|---|---|---|---|
| Risk Factors | Ex/Vg Health | Physician Visit† | Dental Visit† | Surety in Access‡ | Regular Source |
| Child race/ethnicity (ref=white) | |||||
| African American | 0.87¶ (0.78–0.95) | 1.07¶ (1.04–1.10) | 1.00 (0.94–1.06) | 0.95 (0.86–1.01) | 0.99 (0.95–1.02) |
| Asian/Pacific Islander | 0.84¶ (0.77–0.90) | 0.95Φ (0.91–0.99) | 0.91¶ (0.86–0.97) | 0.95 (0.86–1.01) | 0.98 (0.95–1.01) |
| Latino | 0.71¶ (0.66–0.75) | 0.99 (0.96–1.02) | 0.93¶ (0.89–0.97) | 0.93Φ (0.87–0.98) | 0.97Φ (0.94–0.99) |
| Other | 0.87Φ (0.77–0.97) | 1.02 (0.98–1.07) | 0.86¶ (0.76–0.94) | 0.97 (0.88–1.03) | 0.95 (0.90–1.00) |
| Income <200% FPL (ref=200%+FPL) | 0.82¶ (0.77–0.86) | 0.99 (0.97–1.02) | 0.88¶ (0.84–0.92) | 0.93Φ (0.87–0.98) | 0.96¶ (0.93–0.98) |
| Child health insurance (ref=private insurance) | |||||
| Medicaid | 0.87¶ (0.82–0.93) | 0.98 (0.95–1.01) | 0.97 (0.92–1.01) | 1.00 (0.95–1.05) | 0.95¶ (0.91–0.98) |
| Healthy Families | 0.90Φ (0.82–0.98) | 0.92¶ (0.86–0.97) | 0.99 (0.92–1.05) | 0.97 (0.86–1.04) | 0.97 (0.92–1.01) |
| Other insurance | 0.95 (0.86–1.03) | 0.92Φ (0.87–0.98) | 0.88¶ (0.81–0.95) | 0.94 (0.83–1.02) | 0.89¶ (0.82–0.94) |
| Uninsured | 0.83¶ (0.77–0.90) | 0.85¶ (0.80–0.89) | 0.69¶ (0.63–0.76) | 0.93* (0.84–0.99) | 0.68¶ (0.63–0.73) |
| Education <high school§ (ref=high school graduate+) | 0.84¶ (0.78–0.90) | 0.93¶ (0.89–0.97) | 1.02 (0.97–1.06) | 0.99 (0.97–1.03) | 1.02 (0.99–1.03) |
| Non-English language (ref=English language) | 0.80¶ (0.74–0.86) | 0.93¶ (0.89–0.97) | 0.95¶ (0.90–0.99) | 0.96 (0.87–1.02) | 0.97Φ (0.94–0.99) |
Note: Models adjusted for child age, gender, and (for primary care measures) health status.
p<.05;
p<.01;
p<.001 for the prevalence ratio of the category vs. the reference group.
In the past year.
Assessed for adolescents ages 12–17.
Educational level is of the adult respondent for children/adolescents 0–17 years of age, and of the adolescent for those 18–19 years.
Ex/Vg, excellent/very good; PR, prevalence ratio; CI, 95% confidence interval.
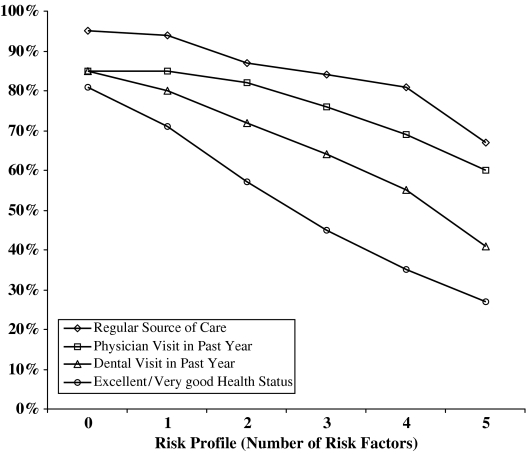
Fourth, the association of vulnerability risk profiles (using 0 risk factors as the reference) with health status and primary care access and continuity is presented using multivariate logistic regression for children and adolescents separately (Table 4). The smaller sample of adolescents required the combination of four and five risk factors into a single profile of four or more risk factors. In addition to comparing the risk profiles to a reference group of 0 risk factors, each risk profile was tested for statistical significance against its preceding profile (by changing the prior profile to the reference group) to examine whether a dose-response relationship is present. Figure 1 shows the prevalence of excellent/very good health status and the measures of access and continuity by risk profiles for the total sample of children.
Table 4.
The Relationship of Risk Profiles with Health Status, and Access to and Continuity of Primary Care
| PR (CI) | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Children Ages 0–11, (N=12,592) | Adolescents Ages 12–19, (N=6,893) | ||||||||
| Risk Profile (Risk Factor) | Ex/Vg Health | Physician Visit∥ | Dental Visit∥ | Regular Source | Ex/Vg Health | Physician Visit∥ | Dental Visit∥ | Surety of Access** | Regular Source |
| 1 | 0.78¶,§ (0.72–0.84) | 0.99 (0.96–1.02) | 0.94Φ,§ (0.89–0.98) | 1.00 (0.97–1.01) | 0.76¶,§ (0.68–0.83) | 1.00 (0.96–1.04) | 0.84¶,§ (0.76–0.91) | 0.94Φ,‡ (0.88–0.99) | 0.92Φ,§ (0.86–0.98) |
| 2 | 0.54¶,§ (0.48–0.60) | 0.95Φ,† (0.90–0.99) | 0.87¶,† (0.80–0.94) | 0.93¶,§ (0.86–0.97) | 0.57¶,§ (0.49–0.65) | 0.98 (0.93–1.02) | 0.64¶,§ (0.56–0.72) | 0.87¶,† (0.79–0.93) | 0.77¶,§ (0.69–0.84) |
| 3 | 0.29¶,§ (0.25–0.36) | 0.84¶,§ (0.78–0.90) | 0.76¶,‡ (0.68–0.83) | 0.88¶,† (0.79–0.94) | 0.43¶,§ (0.34–0.53) | 0.94 (0.86–1.00) | 0.53¶,‡ (0.42–0.63) | 0.71¶,§ (0.60–0.82) | 0.55¶,§ (0.46–0.65) |
| 4†† | 0.19¶,§ (0.16–0.25) | 0.78¶ (0.70–0.85) | 0.63¶,‡ (0.53–0.73) | 0.77¶,§ (0.64–0.87) | 0.28¶,† (0.13–0.41) | 0.76Φ,‡ (0.62–0.89) | 0.37¶,† (0.27–0.51) | 0.67¶ (0.40–0.89) | 0.31¶,§ (0.22–0.44) |
| 5 | 0.13¶ (0.07–0.19) | 0.71¶ (0.55–0.86) | 0.43¶ (0.27–0.64) | 0.54¶,§ (0.36–0.73) | – | – | – | – | – |
| – | – | – | – | – | |||||
Note: Models adjusted for child age, gender, and (for primary care measures) health status.
p<.01;
p<.001 for the difference between the risk profile and a risk profile of zero;
p<.05;
p<.01;
p<.001 for the difference between the risk profile and its preceding risk profile (e.g. three risk factors versus two risk factors).
Reported visit in the past year.
Assessed for adolescents ages 12–17.
For adolescents, four and five risk factors were combined into a single risk profile because of the smaller sample size.
Ex/Vg, excellent/very good; PR, prevalence ratio; CI, 95% confidence interval.
Figure 1.
The Relationship of Risk Profiles with Health Status, and Primary Care Access and Continuity among Children/Adolescents Ages 0–19
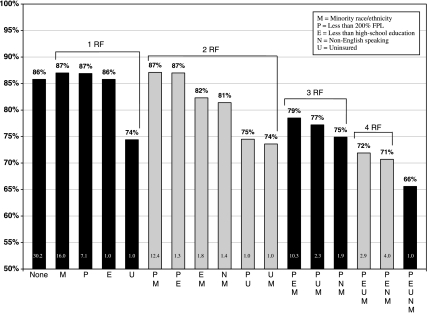
Fifth, differences are explored among various combinations of risk factors in relation to access to care (Figure 2). The figure presents only the most common vulnerability risk profile combinations and their relationship with the receipt of a physician visit in the past year. While all combinations were assessed, only those representing at least 100,000 children—or about 1 percent of all children—in California are presented.
Figure 2.
Common Risk Factor Combinations and the Receipt of a Physician Visit in the Past Year among Children Ages 0–19
Note: Prevalence of the risk factor combination is presented as a percentage at the bottom of the bar.
Sixth, the association of risk profiles (using zero risk factors as the reference) with the reported receipt of counseling on eight health promotion topics was assessed using multivariate logistic regression for adolescents reporting a routine physical exam or check-up in the past year (Table 5). The smaller sample of adolescents who had a physical exam or check-up in the past year required that three, four, and five risk factors be combined into a single profile for adequate statistical reliability, although analyses of higher profiles showed similar patterns (data not shown). Risk profiles were tested for statistical significance against the reference group, and also against the preceding risk profile to examine whether a dose–response relationship exists.
Table 5.
The Relationship of Risk Profiles with Reported Receipt of Health Promotion Counseling Topics among Adolescents (Ages 12–17) Who Saw a Physician for a Routine Physical Exam or Check-Up in the Past Year (n=4,163)
| PR (CI) | ||||||||
|---|---|---|---|---|---|---|---|---|
| Risk Profile (Ref=0) (Risk Factor) | STDs | Emotions | Smoking | Alcohol | Marijuana | Helmets | Seatbelts | Violence |
| 1 | 1.15 (0.99–1.32) | 1.10 (0.94–1.28) | 1.23Φ (1.05–1.43) | 1.30Φ (1.11–1.51) | 1.29¶ (1.07–1.54) | 1.36Φ (1.10–1.67) | 1.33Φ (1.06–1.64) | 1.56¶ (1.23–1.95) |
| 2 | 1.24Φ (1.06–1.44) | 1.18 (1.00–1.38) | 1.27Φ (1.05–1.51) | 1.45¶ (1.20–1.71) | 1.45Φ (1.17–1.76) | 1.32* (1.02–1.67) | 1.59¶ (1.26–1.97) | 1.85¶ (1.44–2.32) |
| 3+ | 1.39Φ (1.12–1.68) | 1.49Φ (1.20–1.79) | 1.18 (0.88–1.53) | 1.33* (1.01–1.71) | 1.59¶ (1.19–2.06) | 1.62Φ (1.18–2.16) | 2.10¶ (1.57–2.71) | 2.32¶ (1.69–3.02) |
Note: Models are adjusted for adolescent age, gender, and health status.
Profiles of three, four, and five risk factors were combined into a single profile of 3+ risks to account for the smaller sample size of adolescents who had a routine physical exam or check-up in the past year and, thus, were asked about receipt of health promotion counseling.
p<.05;
p<.01;
p<.001 for the difference between the risk profile and a risk profile of zero.
STD, sexually transmitted disease; PR, prevalence ratio; CI, confidence interval.
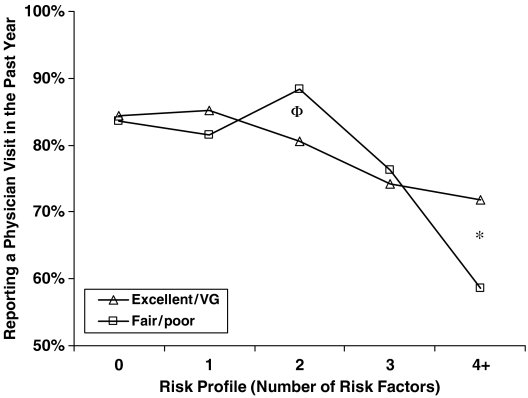
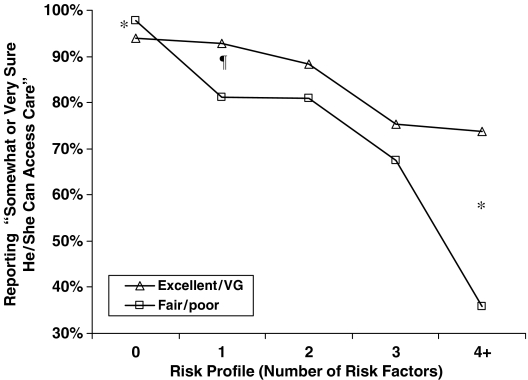
Finally, the relationship between risk profiles and primary care access was examined according to health status to determine if the relationships were different for children/adolescents in “fair or poor” health than for those in “excellent or very good” health. Figures 3 and 4 present analyses of two measures of access: physician visit and access surety. For each risk profile, the difference in the prevalence of the access measure for those in “fair/poor” health was compared with those in “excellent/very good” health and was tested for significance with a Pearson χ2, adjusting for child age and gender.
Figure 3.
The Relationship of Risk Profiles with a Physician Visit in the Past Year by Health Status among Children/Adolescents Ages 0–19
*p<.05, Φp<.01 the difference in having a physician visit in the past year between those in excellent/very good health and those in fair/poor health for a given risk profile.
Figure 4.
The Relationship of Risk Profiles with Self-Reported Surety in Accessing Primary Care by Health Status among Adolescents Ages 12–17
*p<.05; ¶p<.001 the difference in surety in accessing care between those in excellent/very good health and those in fair/poor health for a given risk profile.
RESULTS
Table 1 shows that risk factors for poor primary care are common among both children and adolescents in California. About 57 percent of those ages 0–19 are nonwhite, almost half (46 percent) live below 200 percent of the FPL, and 11.1 percent are uninsured (with 15.1 percent of adolescents uninsured). One-quarter (or 23.9 percent) of children/adolescents have parents or guardians that did not complete high school, and 11.0 percent live in families that do not speak any English at home. Many of those ages 0–19 have multiple risk factors; 43 percent report at least two risk factors (with 22.1 percent reporting two risk factors, 13.6 percent reporting three, 6.2 percent reporting four, and 1.1 percent reporting all five).
Table 2 presents the distribution of risk profiles across two important subgroups that are the focus of recent discussions of access to care in California: family immigration status and geographic region. The analysis shows that families where both the child and parent are citizens are less likely to have multiple RFs (10.2 percent have three or more) compared with families where the child is a citizen and the parent is not a citizen (64.2 percent), and families where both the child and parent are noncitizens (68.3 percent). Families living in urban and rural areas are more likely than those living in second city, suburban, and small town areas to have multiple RFs (34.4 and 35.3 percent have three or more, compared with 21.8, 14.0, and 12.3 percent, respectively).
Table 3 shows that each risk factor is independently related to most, but not every, health status or primary care measure. Controlling for the other risk factors, and child age and gender, an uninsured child/adolescent was 17 percent less likely than a privately insured child/adolescent to be in excellent or very good health, 15 percent less likely to have a physician visit, 31 percent less likely to have a dental visit in the past year, 7 percent less likely to report being somewhat or very sure he/she could access care, and 32 percent less likely to have a regular source of care. After adjustment for other risk factors, however, African Americans, were only found to have significantly poorer health status, and were actually 7 percent more likely to report visiting a physician.
Table 4 demonstrates an apparent dose–response relationship between higher risk profiles and poorer health status, primary care access, and continuity. For example, compared with children aged 0–11 with no risks, children with one were 22 percent less likely to be in “excellent/very good” health. The prevalence was 46 percent lower for those with two risks, 71 percent lower for three, 81 percent lower for four, and 87 percent lower for all five (each p<.001 compared with zero risks and compared with the preceding risk profile). The estimate for five risk factors, however, was not statistically different from the preceding risk profile for this outcome. A similar pattern of decreasing prevalence was apparent for each of the dependent measures. For physician visits among adolescents, however, only the estimate for four or more risk factors was found to be significantly higher compared with zero risks and versus the preceding risk profile (both p<.01). Figure 1 demonstrates the same dose–response relationship for the total child/adolescent sample.
Figure 2 shows the relationship between the most common risk factor combinations and having a physician visit in the past year (for example). The figure reveals that there is a pattern of increasing risk factors associated with a decreasing likelihood of having a physician visit, but that there is substantial variability within each risk profile category (i.e., combinations of two risk factors, three risk factors, etc.) depending on which combination of risk factors is present. There is some variation within each risk profile category suggesting that certain combinations of risks have larger effects than others on having a physician visit. For example, risk profiles including “uninsured” are frequently among those most strongly associated with no physician visit. While not shown, a similar pattern was found between the combination of risks and the other access measures.
Table 5 demonstrates that when examined as combined risk profiles, higher profiles of risk were associated with a higher likelihood of receiving counseling on each of the eight health promotion topics. For example, adjusting for age, gender, and health status, the prevalence of receiving counseling on violence was higher for adolescents with one risk factor (PR=1.56, CI: 1.23–1.95), two risk factors (PR=1.85, CI: 1.44–2.32), and for those with three or more (PR=2.32, CI: 1.69–3.02), although the difference between each risk profile and its preceding risk profile was not significant. Dose-response relationships were apparent for some of the health promotion topics, but were not confirmed through testing.
To provide some detail regarding the association of the individual risk factors with the receipt of health promotion counseling (data not shown), multivariate regressions using individual risk factors rather than risk profiles showed that African Americans were more likely to be counseled on STDs (PR=1.30, CI: 1.00–1.62), Latinos were more likely to be counseled on violence (PR=1.40, CI: 1.04–1.83), uninsured children had higher likelihood of counseling on emotions (PR=1.33, CI=1.02–1.65), and having a parents with less than a high school education was associated with greater receipt of counseling on smoking (PR=1.39, CI: 1.12–1.69) and alcohol use (PR=1.35, CI: 1.06–1.66). While a general pattern of higher counseling was found among many of the individual risk factors and counseling topics, the results were not significant likely due to the smaller analytic sample size of adolescents.
Figures 3 and 4 show that as risk profiles increase, children in fair/poor health status report increasing difficulty with access care than children in excellent/very good health status. The differences in access to care in both figures are nonexistent or reversed at the lowest risk profile, suggesting children who need health services can obtain it when no barriers are present. With a few exceptions, however, the differences are greater as risk profiles increase. For example, at the highest risk profile (4+), the difference in reporting a physician visit in the past year between those in “fair/poor” health and those in “excellent/very good” health increased to about 14 percent. Similarly, at the highest risk profile, the difference in reported surety in accessing care according to health status increased to 45 percent.
DISCUSSION
This study demonstrates that child/adolescent vulnerability can be operationalized as a profile of multiple risk factors. Risk factors for poor health status and poor primary care are very prevalent in California, with about 43 percent of all children and adolescents 19 years of age and under (4.4 million children in the state) having two or more risk factors. In addition to demonstrating that each risk factor is independently associated with most or nearly all of the primary care measures, this study reveals a clear dose-response relationship of increasing risk profiles with poorer child health status, access to and continuity of primary care.
Furthermore, higher risk profiles are associated with greater barriers to accessing primary care for children in “fair or poor” health than for those in “excellent or very good” health, which suggests that children with the greatest health care needs may also have the greatest difficulty obtaining needed care. For children without any risks, however, there was no disparity or a significantly higher rate of reported access for those in “fair/poor” health compared to those in “excellent/very good” health. This suggests that those in need of primary care appear to be obtaining it when risk is absent, but the opposite appears to be true at the highest risk profile. Alternately, a lack of access to care may contribute to the poorer health of the most vulnerable children, but such an interpretation requires a longitudinal analysis.
The finding of higher prevalence of multiple risk factors among immigrant families and families residing in urban or rural areas (compared with those residing in more suburban areas) is of particular interest because both factors have featured prominently in recent California policy discussion regarding expanding access to care for children. New legislation recently introduced aims to expand health insurance coverage to all children in the state regardless of immigration status, and builds upon existing county-based health insurance programs (known most often as Healthy Kids) to specifically target children residing in rural areas through expansions of local programs or linking programs with neighboring counties (The California Endowment 2004). The higher risk profiles identified in this study among immigrant and rural children suggests that this legislative initiative would be one important first step to addressing the higher levels of vulnerability for poor access to care found among noncitizen families and families residing in rural areas.
Among adolescents who reported having a routine physical exam or check-up in the past year, a greater number of risk factors was associated with higher rates of physician counseling on a range of health promotion topics. While may be a potentially effective strategy of targeting the counseling services to adolescents who need it most (i.e., the higher rate corresponds with certain health-related behaviors that are more prevalent in higher risk profile groups), this is not always the case. Among all U.S. high school students in 2002, for example, whites reported higher rates of current cigarette smoking, use of alcohol, and marijuana smoking than African Americans and Hispanics (National Center for Health Statistics 2003). Adolescents with lower risk profiles in this study (including whites), however, were less likely than those with higher-risk profiles to receive counseling on smoking, alcohol use, and marijuana. It is likely that such generalized targeting of health promotion counseling is based on stereotypes of risk behaviors associated with SES and race/ethnicity (van Ryn and Burke 2000; van Ryn 2002).
While this higher rate of counseling is potentially beneficial to higher risk adolescents in this study, adolescents with lower risk profiles (but higher rates of certain risk behaviors) appear to be undertargeted. Even for certain topics where adolescents appear to be targeted for receipt of counseling appropriately, there is still concern that avoidance of counseling low-risk adolescents is not sufficiently “anticipatory,” or rather does not take into account the potential of adolescents to later become high-risk because of changes in family economic status, health insurance, etc. Since eye-balling an adolescent is not a sufficient risk assessment tool, physician should provide health promotion counseling to all adolescents or use more refined and standardized office-based tools for assessing adolescent health risk behaviors.
The analysis of multiple risk factor combinations provides some guidance regarding the risk profiles that may serve as starting points for intervention. Across the sets of risk factors, lacking health insurance coverage was generally found among the profiles associated with the lowest prevalence of having a physician visit in the past year. Because this is a factor that can be modified through policy, it may serve as a focal point for policy efforts to improve primary care for the most vulnerable populations. For example, the legislation proposed to cover all children in the state by building upon existing county-based children's health insurance programs would be an important step forward, particularly if combined with other initiatives to alleviate the risk factors commonly found in combination with lack of insurance (e.g., minimizing cost-sharing to reduce barriers created by poverty status, encouraging the linkage of families with a provider that speaks their language, reducing care-seeking restrictions that create barriers to the development of the patient–provider relationship, etc.) (Stevens and Shi 2002).
There are several limitations to this study. First, the data are cross-sectional and do not demonstrate causality. Simultaneous causation may be a concern for some risk factors (e.g., children who visit the doctor may be more likely to obtain health coverage, as well as vice versa). Second, the risk factors included are not exhaustive. Exploring other risk factors, such as the availability of primary care providers, area of geographic residence, as well as the varying impact of risk factors within certain subgroups such as immigrants may produce different results. Moreover, better understanding of the relative role of various combinations of risk factors is an important next step since, as demonstrated in the one example, not every combinations has the same influence on primary care. Third, the primary care measures in CHIS are limited; other, more detailed measures of primary care experience are now available (Flocke 1997; Safran et al. 1998; Cassady et al. 2000; Seid et al. 2001; Shi, Starfield, and Xu 2001), but have not yet been incorporated in larger state-wide or national surveys. The measure of continuity in this study, for example, did not account for the type of regular source of care which may have some impact on the quality of care. While counseling topics are one important aspect of comprehensiveness, the concept is much broader (i.e., addressing most of the common health needs in a population, including immunizations, mental health, etc.) and thus our results may not be generalizable to the concept of comprehensiveness overall. Finally, while the measure of health status used in CHIS is widely repeated in most national health surveys, its predictive validity is not yet demonstrated for children. For adults, it is a powerful predictor of future morbidity and mortality (Idler and Benyamini 1997; McGee et al. 1999; Burstrom and Fredlund 2001).
Overall, our study confirms that the determinants of poor health, and poor primary care access and continuity for children and adolescents are multifactorial. Analyses of risk profiles based on the major correlates of inadequate primary care revealed a dose–response relationship with poorer health status, and poorer access to and continuity of care. Children and adolescents in “fair or poor” health appear to experience particular difficulties in accessing care when more risk factors are present, suggesting that children with the greatest health needs also have greater difficulty accessing primary care. For adolescents who are able to enter the health care system, however, those with higher risk profiles report higher rates of receiving preventive counseling, indicating some success in targeting certain counseling to adolescents with greater need.
Reducing disparities for vulnerable children and adolescents will likely require multiple, coordinated, health care and social policy strategies. These results imply that a multifactorial approach to vulnerability can be used to target resources, outreach, and access programs to the most vulnerable children. Even so, health systems will need to simultaneously address health insurance gaps and financial barriers to pediatric care; assist with nonfinancial barriers such as health literacy (reflected, in part, by education level), language and other cultural barriers (e.g., linguistic and cultural competence), and assure that families feel empowered to obtain needed care. Strategies to reduce disparities in primary care should be tailored to address these and other co-occurring risks, instead of continuing the fragmented approaches of targeting single risk factors. Barring such a comprehensive approach, it is unlikely that substantial gains will be made in improving primary care and health for the most vulnerable children/adolescents.
Acknowledgments
This research was supported by funds from the California Program on Access to Care (CPAC), California Policy Research Center, University of California, Grant Number CNN03K. The views and opinions expressed do not necessarily represent those of The Regents of the University of California, CPAC, its advisory board, or any state or county executive agency represented thereon. The authors have no disclaimers or disclosures.
REFERENCES
- Aday L. At Risk in America: The Health and Health Care Needs of Vulnerable Populations in the United States. 2d edition. San Francisco: Jossey-Bass; 2001. [Google Scholar]
- American Academy of Pediatrics Committee on Psychosocial Aspects of Child and Family Health. Guidelines for Health Supervision III (updated 2002) Elk Grove Village, IL: American Academy of Pediatrics; 1997. [Google Scholar]
- Bindman AB, Grumbach K, Osmond D, Komaromy M, Vranizan K, Lurie N, Billings J, Stewart A. “Preventable Hospitalizations and Access to Health Care.”. Journal of the American Medical Association. 1995;274((4)):305–11. [PubMed] [Google Scholar]
- Blumenthal D, Mort E, Edwards J. “The Efficacy of Primary Care for Vulnerable Population Groups.”. Health Services Research. 1995;30((1, Part 2)):253–73. [PMC free article] [PubMed] [Google Scholar]
- Bradley RH, Corwyn RF. “Socioeconomic Status and Child Development.”. Annual Review of Psychology. 2002;53:371–99. doi: 10.1146/annurev.psych.53.100901.135233. [DOI] [PubMed] [Google Scholar]
- Brooks-Gunn J, Duncan GJ. “The Effects of Poverty on Children.”. Future of Children. 1997;7((2)):55–71. [PubMed] [Google Scholar]
- Burstrom B, Fredlund P. “Self Rated Health: Is It as Good a Predictor of Subsequent Mortality among Adults in Lower as Well as in Higher Social Classes?”. Journal of Epidemiology and Community Health. 2001;55:836–40. doi: 10.1136/jech.55.11.836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cassady C, Starfield B, Hurtado M, Berk R, Nanda J, Friedenberg L. “Measuring Consumer Experiences with Primary Care.”. Pediatrics. 2000;105((4, Part 2)):998–1003. [PubMed] [Google Scholar]
- Chande V, Kinnane J. “Role of the Primary Care Provider in Expediting Care of Children with Acute Appendicitis.”. Archives of Pediatrics and Adolescent Medicine. 1996;150((7)):703–6. doi: 10.1001/archpedi.1996.02170320049008. [DOI] [PubMed] [Google Scholar]
- Christakis D, Mell L, Koepsell T, Zimmerman F, Connell F. “Association of Lower Continuity of Care with Greater Risk of Emergency Department Use and Hospitalization in Children.”. Pediatrics. 2001;107((3)):524–9. doi: 10.1542/peds.107.3.524. [DOI] [PubMed] [Google Scholar]
- DiLiberti JH. “The Relationship between Social Stratification and All-Cause Mortality among Children in the United States: 1968–1992.”. Pediatrics. 2000;105((1)):e2. doi: 10.1542/peds.105.1.e2. [DOI] [PubMed] [Google Scholar]
- Donaldson M, Yordy K, Lohr K, Vanselow N. Primary Care: America's Health in a New Era. Washington, DC: National Academy Press; 1996. [PubMed] [Google Scholar]
- Elster A, Jarosik J, VanGeest J, Fleming M. “Racial and Ethnic Disparities in Health Care for Adolescents: A Systematic Review of the Literature.”. Archives of Pediatrics & Adolescevt Medicine. 2003;157((9)):867–74. doi: 10.1001/archpedi.157.9.867. [DOI] [PubMed] [Google Scholar]
- Flocke S. “Measuring Attributes of Primary Care: Development of a New Instrument.”. Journal of Family Practice. 1997;45((1)):64–74. [PubMed] [Google Scholar]
- Flores G, Bauchner H, Feinstein AR, Nguyen U. “The Impact of Ethnicity, Family Income, and Parental Education on Children's Health and Use of Health Services.”. American Journal of Public Health. 1999;89((7)):1066–71. doi: 10.2105/ajph.89.7.1066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forrest CB, Starfield B. “The Effect of First-Contact Care with Primary Care Clinicians on Ambulatory Health Care Expenditures.”. Journal of Family Practice. 1996;43((1)):40–8. [PubMed] [Google Scholar]
- Fox MH, Moore J, Davis R, Heintzelman R. “Changes in Reported Health Status and Unmet Need for Children Enrolling in the Kansas Children's Health Insurance Program.”. American Journal of Public Health. 2003;93((4)):579–82. doi: 10.2105/ajph.93.4.579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franks P, Fiscella K. “Primary Care Physicians and Specialists as Personal Physicians. Health Care Expenditures and Mortality Experience.”. Journal of Family Practice. 1988;47((2)):105–9. [PubMed] [Google Scholar]
- Furstenberg FJ, Cook T, Eccles J, Edler G, Sameroff AJ. Urban Families and Adolescent Success. Chicago: University of Chicago Press; 1999. [Google Scholar]
- Gill J, Mainous A, Nsereko M. “The Effect of Continuity of Care on Emergency Department Use.”. Archives of Family Medicine. 2000;9((4)):333–8. doi: 10.1001/archfami.9.4.333. [DOI] [PubMed] [Google Scholar]
- Goodman E. “The Role of Socioeconomic Status Gradients in Explaining Differences in U.S. Adolescents' Health.”. American Journal of Public Health. 1999;89((10)):1522–8. doi: 10.2105/ajph.89.10.1522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green M, Palfrey J, editors. Bright Future: Guidelines for Health Supervision of Infants, Children, and Adolescents. 2d edition. Arlington, VA: National Center for Education in Maternal and Child Health; 2000. [Google Scholar]
- Holl JL, Szilagyi PG, Rodewald LE, et al. “Evaluation of New York State's Child Health Plus: Access, Utilization, Quality of Health Care, and Health Status.”. Pediatrics. 2000;105((3, suppl E)):711–8. [PubMed] [Google Scholar]
- Idler EL, Benyamini Y. “Self-Rated Health and Mortality: A Review of Twenty-Seven Community Studies.”. Journal of Health and Social Behavior. 1997;38:21–37. [PubMed] [Google Scholar]
- Inkelas M, Halfon N, Uyeda K, Stevens G, Wright J, Holtby S, Brown ER. The Health of Young Children in California: Findings from the 2001 California Health Interview Survey. Los Angeles and Sacramento: UCLA Center for Health Policy and Research and First 5 California; 2003. [Google Scholar]
- LaVeist T. “Beyond Dummy Variables and Sample Selection: What Health Services Researchers Ought to Know about Race as a Variable.”. Health Services Research. 1994;29((1)):1–16. [PMC free article] [PubMed] [Google Scholar]
- Lave JR, Keane CR, Lin CJ, Ricci EM, Amersbach G, LaVallee CP. “Impact of a Children's Health Insurance Program on Newly Enrolled Children.”. Journal of the American Medical Association. 1998;279((22)):1820–5. doi: 10.1001/jama.279.22.1820. [DOI] [PubMed] [Google Scholar]
- Lurie N, Ward N, Shapiro M, Brook R. “Termination from Medical–Does It Affect Health?”. New England Journal of Medicine. 1984;311((7)):480–4. doi: 10.1056/nejm198408163110735. [DOI] [PubMed] [Google Scholar]
- Lurie N, Zhan C, Sangl J, Bierman AS, Sekscenski ES. “Variation in Racial and Ethnic Differences in Consumer Assessments of Health Care.”. American Journal of Managed Care. 2003;9((7)):502–9. [PubMed] [Google Scholar]
- McGee DL, Liao Y, Cao G, Cooper RS. “Self-Reported Health Status and Mortality in a Multiethnic U.S. Cohort.”. American Journal of Epidemiology. 1999;149((1)):41–6. doi: 10.1093/oxfordjournals.aje.a009725. [DOI] [PubMed] [Google Scholar]
- Montgomery LE, Kiely JL, Pappas G. “The Effects of Poverty, Race, and Family Structure on U.S. Children's Health: Data from the NHIS, 1978 through 1980 and 1989 through 1991.”. American Journal of Public Health. 1996;86((10)):1401–5. doi: 10.2105/ajph.86.10.1401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Center for Health Statistics. Health, United States 2003. Hyattsville, MD: Centers for Disease Control; 2003. [Google Scholar]
- Newacheck PW, Hughes DC, Stoddard J. “Children's Access to Primary Care: Differences by Race, Income and Insurance Status.”. Pediatrics. 1996;97((1)):26–32. [PubMed] [Google Scholar]
- Newacheck PW, Hung Y, Hochstein M, Halfon N. “Access to Health Care for Disadvantaged Young Children.”. Journal of Early Intervention. 2002;25((1)):1–11. [Google Scholar]
- Newacheck PW, Stein RE, Bauman L, Hung YY. “Disparities in the Prevalence of Disability between Black and White Children.”. Archives of Pediatrics & Adolescent Medicine. 2003;157((3)):244–8. doi: 10.1001/archpedi.157.3.244. [DOI] [PubMed] [Google Scholar]
- Newacheck PW, Stoddard JJ, Hughes DC, Pearl M. “Health Insurance and Access to Primary Care for Children.”. New England Journal of Medicine. 1998;338((8)):513–9. doi: 10.1056/NEJM199802193380806. [DOI] [PubMed] [Google Scholar]
- Ortega AN, Stewart DC, Dowshen SA, Katz SH. “Perceived Access to Pediatric Primary Care by Insurance Status and Race.”. Journal of Community Health. 2000;25((6)):481–93. doi: 10.1023/a:1005196714900. [DOI] [PubMed] [Google Scholar]
- Parker S, Greer S, Zuckerman B. “Double Jeopardy: The Impact of Poverty on Early Childhood Development.”. Pediatric Clinics of North America. 1988;35((6)):1227–40. doi: 10.1016/s0031-3955(16)36580-4. [DOI] [PubMed] [Google Scholar]
- van Ryn M. “Research on the Provider Contribution to Race/Ethnicity Disparities in Medical Care.”. Medical Care. 2002;40((1 suppl)):140–51. doi: 10.1097/00005650-200201001-00015. [DOI] [PubMed] [Google Scholar]
- Safran D, Kosinski M, Tarlov A, Rogers WH, Taira DH, Lieberman N, Ware JE. “The Primary Care Assessment Survey: Tests of Data Quality and Measurement Performance.”. Medical Care. 1998;36((5)):728–39. doi: 10.1097/00005650-199805000-00012. [DOI] [PubMed] [Google Scholar]
- Safran DG, Taira D, Rogers WH, Kosinski M, Ware JE, Tarlov AR. “Linking Primary Care Performance to Outcomes of Care.”. Journal of Family Practice. 1998;47((3)):213–9. [PubMed] [Google Scholar]
- Sameroff AJ, Seifer R, Barocas R, Zax M, Greenspan S. “Intelligence Quotient Scores of 4-year-old Children: Social–Environmental Risk Factors.”. Pediatrics. 1987;79((3)):343–50. [PubMed] [Google Scholar]
- Seid M, Stevens G, Varni J. “Parents' Perceptions of Pediatric Primary Care Quality: Effects of Race/Ethnicity, Language, and Access.”. Health Services Research. 2003;38((4)):1009–31. doi: 10.1111/1475-6773.00160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seid M, Varni J, Bermudez L, et al. “Parents' Perceptions of Primary Care: Measuring Parents' Experiences of Pediatric Primary Care Quality.”. Pediatrics. 2001;108((2)):264–70. doi: 10.1542/peds.108.2.264. [DOI] [PubMed] [Google Scholar]
- Shi L. “Primary Care, Specialty Care, and Life Chances.”. International Journal of Health Services. 1994;24((3)):431–58. doi: 10.2190/BDUU-J0JD-BVEX-N90B. [DOI] [PubMed] [Google Scholar]
- Shi L, Green LH, Kazakova S. “Primary Care Experience and Racial Disparities in Self-Reported Health Status.”. Journal of American Board on Family Practice. 2004;17((6)):443–52. doi: 10.3122/jabfm.17.6.443. [DOI] [PubMed] [Google Scholar]
- Shi L, Starfield B, Xu J. “Validating the Adult Primary Care Assessment Tool.”. Journal of Family Practice. 2001;50((2)):E1. [Google Scholar]
- Shi L, Stevens GD. Vulnerable Populations in the United States. San Francisco: Jossey-Bass; 2005. [Google Scholar]
- Smedley B, Stith A, Nelson A, editors. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academy Press; 2002. [PubMed] [Google Scholar]
- Starfield B. “Family Income, Ill Health, and Medical Care of U.S. Children.”. Journal of Public Health Policy. 1982;3((3)):244–59. [PubMed] [Google Scholar]
- Starfield B. “Primary Care: Is It Essential?”. Lancet. 1994;344((8930)):1129–33. doi: 10.1016/s0140-6736(94)90634-3. [DOI] [PubMed] [Google Scholar]
- Starfield B. Primary Care: Balancing Health Needs, Services, and Technology. New York: Oxford University Press; 1998. [Google Scholar]
- Starfield B, Riley AW, Witt WP, Robertson J. “Social Class Gradients in Health during Adolescence.”. Journal of Epidemiology and Community Health. 2002;56((5)):354–61. doi: 10.1136/jech.56.5.354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Starfield B, Robertson J, Riley AW. “Social Class Gradients and Health in Childhood.”. Ambulatory Pediatrics. 2002;2((4)):238–46. doi: 10.1367/1539-4409(2002)002<0238:scgahi>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- Stevens GD, Shi L. “Racial and Ethnic Disparities in the Quality of Primary Care for Children.”. Journal of Family Practice. 2002;51((6)):573. [PubMed] [Google Scholar]
- Stevens GD. “Effect of Managed Care on Children's Relationships with Their Primary Care Physicians: Differences by Race.”. Archives of Pediatrics & Adolescent Medicine. 2002;156((4)):369–77. doi: 10.1001/archpedi.156.4.369. [DOI] [PubMed] [Google Scholar]
- Stevens GD. “Racial and Ethnic Disparities in the Primary Care Experiences of Children: A Review of the Literature.”. Medical Care Research and Review. 2003;60((1)):3–30. doi: 10.1177/1077558702250229. [DOI] [PubMed] [Google Scholar]
- The California Endowment. Health Insurance Coverage for All Children: A Goal within Reach. 2. Vol. 3. Woodland Hills, CA: The California Endowment; 2004. [Google Scholar]
- >U.S. Department of Health and Human Services. Healthy People 2010: Understanding and Improving Health. 2d edition. Washington, DC: U.S. Government Printing Office; 2000. [Google Scholar]
- van Ryn M, Burke J. “The Effect of Patient Race and Socio-Economic Status on Physicians' Perceptions of Patients.”. Social Science and Medicine. 2000;50:813–28. doi: 10.1016/s0277-9536(99)00338-x. [DOI] [PubMed] [Google Scholar]
- Weech-Maldonado R, Morales L, Spritzer K, Elliot M, Hays R. “Racial and Ethnic Differences in Parents' Assessments of Pediatric Care in Medicaid Managed Care.”. Health Services Research. 2001;36((3)):575–94. [PMC free article] [PubMed] [Google Scholar]
- Wood PR, Smith LA, Romero D, Bradshaw P, Wise PH, Chavkin W. “Relationships between Welfare Status, Health Insurance Status, and Health and Medical Care among Children with Asthma.”. American Journal of Public Health. 2002;92((9)):1446–52. doi: 10.2105/ajph.92.9.1446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang J, Yu KF. “What's the Relative Risk? A Method of Correcting the Odds Ratio in Cohort Studies of Common Outcomes.”. Journal of the American Medical Association. 1998;280((19)):1690–1. doi: 10.1001/jama.280.19.1690. [DOI] [PubMed] [Google Scholar]