Abstract
Objective
To provide detailed demographic profiles of prescription drug utilization and expenditures in order to isolate the impact of demographic change from other factors that affect drug expenditure trends.
Data Sources/Study Setting
Demographic information and drug utilization data were extracted for virtually the entire British Columbia (BC) population of 1996 and 2002. All residents had public medical and hospital insurance; however their drug coverage resembled the mix of private and public insurance in the United States.
Study Design
A series of research variables were constructed to illustrate profiles of drug expenditures and drug utilization across 96 age/sex strata.
Data Collection/Extraction Methods
Drug use and expenditure information was extracted from the BC PharmaNet, a computer network connecting all pharmacies in the province.
Principal Findings
Per capita drug expenditures increased at an average annual rate of 10.8 percent between 1996 and 2002. Population aging explained 1.0 points of this annual rate of expenditure growth; the balance was attributable to rising age/sex-specific drug expenditures.
Conclusions
Relatively little of the observed increase in drug expenditures in BC could be attributed to demographic change. Most of the expenditure increase stemmed from the age/sex-specific quantity and type of drugs purchased. The sustainability of drug spending therefore depends not on outside forces but on decisions made by policy makers, prescribers, and patients.
Keywords: Prescription drugs, expenditures, demographics, British Columbia
Population demographics play important roles in health system trends and feature prominently in popular rhetoric about health care policy. For example, there is little doubt that the effects of the post-war “baby boom” are being felt in health care systems. Certain and inevitable cost pressures result from the fact that the generation of baby boomers is now of the age where their health care needs can be expected to increase significantly every year. Add to this demographic phenomenon that of a steady increase in average longevity and the image of a demographic crisis in health care is not hard to evoke. There is, however, a danger of misrepresenting the pressures caused by demographic forces. Overestimating the role of demographic forces in health expenditure trends can call into question the fiscal prudence of public health care programs or draw attention away from cost-drivers that might otherwise be managed (Evans 1985; Evans et al. 2001). In contrast, underestimating the impact of demographic change on specific health care needs could lull policy makers into missing opportunities to plan for future requirements.
To foster prudent policy and planning, health services researchers must accurately depict the health services use of a population by age and sex, and then carefully measure the impact that population demographics have on health care systems and specific components thereof. For example, researchers have shown that, despite steep age-gradients in service utilization, population aging has explained approximately 1–2 percentage points of medical and hospital expenditure growth (Fuchs 1984; Barer, Evans, and Hertzman 1995; Reinhardt 2003). Owing in part to a lack of necessary data, and to the fact that pharmaceuticals have historically been a minor component of health system expenditures (Berndt 2001), there is less information about the demographics of prescription drugs. Researchers have illustrated static age gradients in pharmaceutical use in North America (Mueller, Schur, and O'Connell 1997; Metge et al. 1999). And, using data from U.S. surveys and private drug plans, or from public programs in Europe, researchers have estimated that population aging may increase drug expenditures by 1 to 3 percent per year (Van Tielen, Peys, and Genaert 1998; Merlis 2000; Gerdtham and Lundin 2004).
With the recent addition of a Medicare drug benefit in the U.S. (U.S.A. 2003), ongoing changes to seniors drug benefits in Canada (Morgan, Barer, and Agnew 2003), and continued rapid growth in pharmaceutical expenditures (IMS 2004), the extent to which demographics affect pharmaceutical expenditures will have growing significance in North American policy debates over the coming years. This study uses a population-based, patient-specific pharmaceutical database from the Canadian province of British Columbia (BC) to depict the population's age/sex profiles of drug utilization and expenditures from 1996 to 2002. It also provides estimates of expenditure trends that isolate the impact of demographic forces from the impact of utilization and expenditure dynamics that may be managed through policy. The unique dataset used permit demographic patterns to be calculated with an accuracy and detail not possible with existing surveys or nonrepresentative drug plan datasets. The main findings should be reasonably generalizable in North America. For, while all BC residents have public medical and hospital insurance, their drug coverage over the period of analysis resembled somewhat the mix of private and public insurance that will be in effect in the United States when the Medicare drug benefit is fully implemented. Potential sources of differences in drug use are outlined in the discussion.
METHODS
Data
Demographic information and drug utilization data were extracted for virtually the entire BC population in 1996 and 2002. Demographic information was assembled from the population registry files of the BC Linked Health Database at the UBC Centre for Health Services and Policy Research. Owing to special circumstances concerning stewardship for drug utilization data for registered First Nations, veterans, and the Royal Canadian Mounted Police, the study excluded those cohorts. The study cohort therefore comprised approximately 96 percent of the provincial population: 3.9 million in 1996 and 4.1 million in 2002. All members of this cohort were publicly insured for medical and hospital care. Their drug coverage was mixed. The government offered prescription drug coverage to all social assistance recipients and seniors, and subsidized drug expenses exceeding $1,000 for nonseniors (British Columbia 2001). Approximately 50 percent of the working population had voluntary, employment-related private drug coverage, and the balance of the working population was effectively uninsured for routine drug expenditures (Applied Management, Fraser Group, and Tristat Resources 2000).
Drug use and expenditure information for each member of the study cohort was extracted from the BC PharmaNet, a computer network connecting all pharmacies in the province, including dispensaries of long-term care facilities. A record of all filled prescriptions, regardless of payer type, must be entered into this database by law. Prescriptions for over-the-counter medicines, vitamins, and medical supplies (e.g., test strips) were excluded. Each of the 49.7 million records extracted included the following variables: dispensation date, patient identification number (encrypted), drug identification number, drug quantity, and cost. Cost information included all sources of public and private payment for ingredient costs, markups, and pharmacists' professional fees.
Each drug identified in the database was assigned to one of 14 broad therapeutic categories using the World Health Organization's Anatomic Therapeutic Chemical Classification System (WHO 2004). These broad and mutually exclusive groupings include such categories as “alimentary tract and metabolism,”“blood and blood forming organs,”“cardiovascular system,” and “dermatologicals.” They were assigned so that analyses could be stratified by the nature of drugs being used and so that the number of different types of treatment used by each patient could be quantified (Morgan 2002). A patient could receive between 1 and 14 different types of prescription drug treatment provided that she or he filled one or more prescriptions for drugs from respective therapeutic categories.
Variables and Expenditure Equations
Expenditures per capita are a function of the population profile and the age-specific expenditure profile. To depict these profiles, the BC population was stratified by sex and by 2-year age intervals. Newborns were included in the cohort aged 2 and under, and residents aged 91 and older were combined in a single 91+ cohort, yielding a total of 92 age/sex cells in the population frame. For each age/sex cell (e.g., 41–42 year-old females), cohort size, and age-specific average per capita expenditures were computed for 1996 and 2002.
The change in population-wide expenditures per capita was calculated as the product of changes in the population share falling into each age/sex category and changes in age-specific average expenditures per capita:
Here, EXP/POP depicts population-wide expenditure per capita; agesexPOP depicts the matrix of population shares falling into the 92 age/sex cells; and agesexEXP/POP depicts the matrix of age/sex-specific expenditures per capita. With this formula, a measure of the impact of population aging on drug expenditures was computed by forecasting how population-wide per capita expenditures would change if the population age profile had changed while age-specific average per capita expenditures remained constant. This was done separately using the 1996 and 2002 age/sex expenditure profiles as the constant expenditures, and the geometric mean was taken of the two measures (which differed by less than 0.2 percent over 6 years). The geographic mean, known as Fisher's Ideal index formula, has the desirable property that no unexplained residual remains after the impact of all variables in the expenditure equation are calculated (Diewert 1993).
The measurement of the impact of aging can be illustrated with a simplified example. Suppose that the population in 1996 was 10 percent elderly and 90 percent nonelderly, and that drug expenditures were $100.00 per elderly and $10.00 per nonelderly, yielding an average expenditure per capita of $19.00. Suppose also that the population in 2002 was 15 percent elderly and 85 percent nonelderly, with age-specific expenditures per capita of $150.00 and $20.00, yielding an average expenditure per capita of $39.50. The impact of aging in this scenario can be computed by comparing actual expenditure per capita in 1996 ($19.00) with a hypothetical level for 2002. The hypothetical level for 2002 is that which would have occurred if age-specific expenditures were held constant at the 1996 level ($100 and $10) but the age of the population changed to the 2002 level (15 percent elderly): this yields a hypothetical $23.50 per capita for 2002, which compared with actual costs in 1996 reflects an age-related increase of 24 percent. The rest of the change in expenditure ($16.00 per capita, or 76 percent) would have been because of changes in age-specific drug expenditure: the 50 percent rise in expenditure per elderly and 100 percent rise in expenditure per nonelderly.
To provide information about changes in age/sex-specific expenditures, matrices of the following measures were computed: agesexUSE, the percentage of the age/sex-specific cohort that “used” one or more prescription of any kind; agesexTx, the age/sex-specific average number of the 14 therapeutic classes from which prescription users received one or more prescriptions; agesexRx/Tx, the age/sex-specific average number of prescriptions filled per patient per therapeutic category; and agesexCOST/Rx, the age/sex-specific average cost per prescription filled. These factors combine in the following equation describing changes in age/sex-specific expenditures:
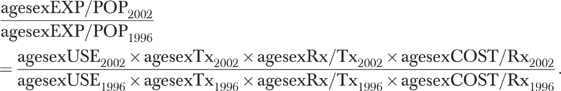 |
Cost per prescription can be further broken down into two components: agesexMIX/Rx, the age/sex-specific mix of drug products selected per prescription within therapeutic categories, including changes in dosages selected; and PRICE/PILL, a price index for all products in each therapeutic category. Because of the underlying data requirements, the price index for each therapeutic class was computed for five broad age categories (residents aged 0–19, 20–44, 45–64, 56–84, and 85 and older). With these price estimates, the age/sex-specific cost per prescription can be described with the following equation:
The impact of each factor in the equations describing age/sex-specific expenditures per capita and age/sex-specific costs per prescription was calculated using the methods described for the measurement of the impact of population aging. Each factor's impact on population-wide expenditures per capita is calculated holding constant all other factors, including the effect of population aging.
RESULTS
Population Profiles of Drug Expenditure and Drug Use
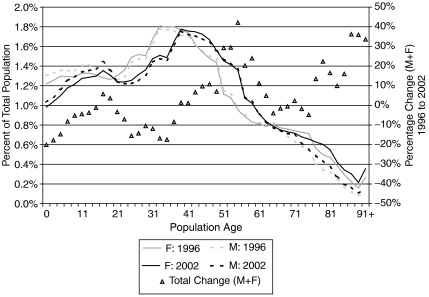
Figure 1 illustrates the age/sex profile of the BC population in 1996 and 2002 and, on the right-hand scale, the total percentage change in the share of the population (male plus female) that fell in the age-specific cohort between 1996 and 2002. It illustrates the wave of baby-boomers, roughly aged 40–60 in 2002, followed by a decline in the population profile (the “baby bust” generation, or generation X), and then a second relatively large generation comprised of the boomers children (the echo generation) (Foot and Stoffman 1998). Owing to aging of the boomers, the share of the population aged 45–60 grew significantly: rising from 18.8 percent in 1996 to 22.5 percent in 2002. In contrast, the share of the population younger than 10 declined from 13 percent in 1996 to 11.3 percent in 2002, and the population share aged 21–40 fell from 31.6 to 28.3 percent. Owing to increased longevity in BC, the share of the population aged 85 and older increased from 1.4 percent of the population in 1996 to 1.8 percent of the population in 2002.
Figure 1.
Age/Sex Profiles of Population, 1996 and 2002
The effect of population aging on overall drug expenditures will depend on the gradient of age-specific drug expenditure—Figure 2. Over the male and female age-specific drug expenditure profiles in both 2002 and 1996, average expenditures for an individual increased by roughly 3.5 percent per year of age from 35 to 65 years of age. Age-specific expenditures per capita fall beyond age 80, which may reflect a healthy-survivor selection bias. In addition to the slope in the age gradient, the other principle finding from Figure 2 is that, between 1996 and 2002, age-specific drug expenditures increased by between 60 and 90 percent for adults over age 30 and increased by 20–60 percent for younger populations.
Figure 2.
Age/Sex Profiles of Expenditures per Capita, 1996 and 2002
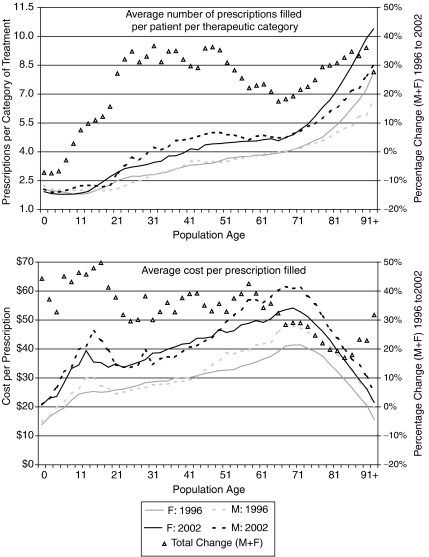
Factors contributing to the age/sex profiles of drug expenditures are illustrated in Figure 3. Each graph in Figure 3 illustrates the age-specific levels of a variable for males and females as well as the percentage change in these variables for all persons of given ages (male and female combined). The scale of the percentage change measures is found on the right side of each graph; moreover, it is identically scaled across all graphs in Figure 3, allowing ready comparison of the differences in growth across ages and across variables.
Figure 3a Figure 3b.
Sex Profiles of Contributors to Expenditures, 1996 and 2002
Age/Sex of Contributors to Expenditures, 1996 and 2002
The profile of “use” of any drug treatment shows that the share of an age/sex cohort that receives one or more prescription drugs increases slightly with age and is notably higher for females, particularly those of childbearing age. While not shown in the figure, secondary analysis illustrated that use in drugs from ATC categories G (“genito urinary system and sex hormones”) and N (“nervous system”) explain virtually all of the gender difference between ages 13 and 73. In both 1996 and 2002, greater than 75 percent of females over age 17 filled one or more prescriptions; only males over age 55 filled prescriptions at a rate of 75 percent or more. The rate of drug use among adults over age 50 increased by 2–5 percent between 1996 and 2002, while use fell for younger cohorts, particularly children under 13 years of age.
Conditional on use of at least one drug of any kind, the average number of distinct therapeutic categories from which patients received prescriptions increased with age and was consistently higher for females beyond childhood. The average child that was exposed to any drug therapy filled prescriptions from approximately 1.5 different therapeutic categories. Rising steadily with age, the average number of categories of drug received by prescription users was above three for residents aged 50 and older and above four for residents aged 80 and older. Between 1996 and 2002, this age/sex-specific profile rose only slightly, with the rate of change slightly greater for older adults.
The age/sex profile of prescriptions filled per patient per therapeutic category had a moderate, positive slope between ages 15 and 65. Beyond age 65, this positive age-gradient increases substantially, particularly for females. The number of prescriptions per patient per therapeutic category increased between 1996 and 2002 at rates ranging from 20 to 31 percent across adult cohorts. The change was more rapid for males than females. Whereas males and females age 23–64 filled comparable numbers of prescriptions per course of therapy in 1996, male prescription users age 23–64 filled a larger number of prescriptions per therapeutic category than their female contemporaries did in 2002.
The average cost per prescription filled increased with age up to age 70 for both the 1996 and 2002 age/sex profiles. Costs per prescription fell sharply with age beyond age 70. Given the profile of prescriptions per patient per category, it appears that older users of prescription drugs fill a greater quantity of less costly prescriptions per course of treatment. This may reflect the dispensation of “shorter” prescriptions for older populations. Age/sex-specific costs per prescription, which rose at rates of 17–50 percent, increased more rapidly than other factors contributing to age-specific expenditures per capita. Growth in costs per prescription was highest among children, and lowest among residents aged 67–84. Total price inflation between 1996 and 2002 for the drug products selected per prescription was approximately 0.9 percent for adults (of all ages) and 1.2 percent for children (average annual rates of 0.13 and 0.17 percent, respectively). This indicates that almost all of the change in costs per prescription stemmed from changes in the mix of products selected.
Causes of Change in Population-Wide Expenditures per Capita
The preceding profiles of drug expenditure and utilization measures combine to determine population-wide expenditures per capita. Prescription drug expenditures per BC resident increased by 86 percent from $186 in 1996 to $344 in 2002. Expenditures per female increased by 82 percent, from $213 to $389, and expenditures per male increased by 90 percent, from $158 to $300. Table 1 lists the determinants of these changes in expenditure per capita for all prescription drugs, and for the fastest growing therapeutic categories.
Table 1.
Determinants of Change in Per Capita Prescription Drug Expenditures, 1996–2002
| Overall drug use | Cardiovascular | Nervous system | Alimentary tract and metabolism | Genitourinary system and sex hormones | Anti-Infectives for systemic use | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| F | M | Total | F | M | Total | F | M | Total | F | M | Total | F | M | Total | F | M | Total | |
| 1996 per capital expenditure | $213 | $158 | $186 | $47.80 | $44.90 | $46.40 | $49.20 | $33.50 | $41.40 | $25.70 | $19.00 | $22.40 | $23.90 | $3.90 | $14.00 | $18.30 | $15.20 | $16.80 |
| 2002 per capital expenditure | $389 | $300 | $344 | $88.50 | $92.20 | $90.30 | $100.40 | $72.70 | $86.70 | $49.80 | $39.00 | $44.50 | $32.20 | $11.30 | $21.90 | $24.20 | $21.40 | $22.80 |
| Total change | 82% | 90% | 86% | 85% | 105% | 95% | 104% | 118% | 110% | 94% | 104% | 98% | 35% | 187% | 63% | 33% | 43% | 38% |
| Population aging | 6% | 7% | 6% | 8% | 11% | 10% | 5% | 4% | 5% | 7% | 8% | 8% | 1% | 10% | 3% | 1% | 2% | 1% |
| Age-specific expenditures | 73% | 77% | 75% | 71% | 85% | 78% | 94% | 109% | 100% | 81% | 89% | 84% | 33% | 161% | 59% | 32% | 41% | 36% |
| Age-specific expenditures | ||||||||||||||||||
| Rate of use | 0% | 0% | 0% | 19% | 31% | 24% | 4% | 2% | 3% | 10% | 12% | 11% | 10% | 206% | 37% | −11% | −13% | −12% |
| Number of categories | 5% | 5% | 5% | |||||||||||||||
| Rx per category | 23% | 29% | 26% | 31% | 27% | 29% | 43% | 64% | 51% | 14% | 15% | 14% | 8% | 8% | 8% | 0% | −1% | −1% |
| Drug mix | 32% | 29% | 31% | 10% | 12% | 11% | 33% | 26% | 30% | 46% | 47% | 46% | 11% | −20% | 7% | 48% | 65% | 56% |
| Prince inflation | 1% | 1% | 1% | 0% | 0% | 0% | −1% | −1% | −1% | −1% | −1% | −1% | 0% | −1% | 0% | 0% | 0% | 0% |
Population aging per se was sufficient to increase per capita drug expenditures by 6 percent (6 percent for females and 7 percent for males). Aging had a slightly larger impact on expenditures per male because the age gradient of expenditure per male was steeper over the range of ages for which population growth was most rapid. After accounting for aging, increases in age-specific drug expenditure along the demographic profile caused population-wide prescription drug expenditures per capita to increase by 75 percent between 1996 and 2002. Age-specific expenditures increased more rapidly for males (77 percent) than for females (73 percent).
The most significant determinant of drug spending at the population level—slightly more so for females than males—was changes in the age-specific mix of drugs prescribed per prescription. These changes were sufficient to increase the average expenditures per capita by 31 percent (29 percent for males and 32 percent for females). The second largest impact on per capita drug expenditures was the age-adjusted number of prescriptions filled per patient per therapeutic category, which increased population-wide per capita expenditures by 26 percent (29 percent for males and 23 percent for females). Changes in the age-specific rates at which residents used one or more prescription drugs had no measurable impact on population-wide drug expenditures, whereas the rise in age/sex-specific average numbers of categories used per “exposed” patient caused expenditures per capita to increase by 5 percent. Finally, drug price inflation (for existing products) increased expenditures per capita by 1 percent.
Causes of Change by Drug Category
In 1996 and 2002, over 75 percent of total drug expenditures were concentrated in the five fastest-growing broad therapeutic categories of drug treatment—Table 1. In descending order of expenditure, these categories were cardiovascular; nervous system; alimentary tract and metabolism; genitourinary system and sex hormones; and antiinfectives for systemic use.
Cardiovascular medicines were the largest drug category in terms of spending for males and second largest for females. Population aging caused per capita cardiovascular drug expenditures to rise by 10 percent between 1996 and 2002. This was slightly higher than the impact of aging on overall drug expenditures per capita because of the fact that there is a relatively steep age gradient in cardiovascular drug expenditures. Increases in the rate at which patients received cardiovascular drugs and increases in the quantity of prescriptions filled per recipient explained most of the expenditure change in this category. Given the breadth of the cardiovascular category, some of the increase in prescriptions filled per patient may reflect increased treatment of concomitant cardiovascular conditions (e.g., high cholesterol and hypertension).
Expenditure on nervous system treatments grew more quickly than overall drug expenditures, and accounted for 25 percent of total expenditures in 2002. Population aging had a relatively modest, 5 percent impact on nervous system drug expenditures because the age gradient was relatively flat for this therapeutic category. Most of the increase in nervous system drug expenditures resulted from age-adjusted increases in the number of prescriptions per recipient of therapy and changing mix of products selected.
Demographics played varying roles in the remaining top-selling therapeutic categories. While population aging had a pronounced impact on cardiovascular drug expenditure, it played a minor role in the antiinfective category. Aging had a small impact on genitourinary drug expenditure per female, but had a significant impact on expenditure per male in the same class. After adjusting for aging, the rate of use was the most significant determinant of increased spending on genitourinary drugs. Changes in the mix of drugs selected per prescription had the most significant impact on expenditures per capita for the remaining large therapeutic categories: alimentary tract and metabolism drugs; and antiinfectives for systemic use.
DISCUSSION
Between 1996 and 2002 in BC, per capita drug expenditures grew at a rate of 10.8 percent per annum. Despite steep age gradients in drug expenditure, population aging explained 1.0 points of the observed annual rate of expenditure growth. Most of the observed increase in per capita expenditures resulted from the fact that age/sex-specific drug expenditures rose significantly at all points in the population's demographic profile. The increase in age/sex-specific drug expenditures was largely the result of increases in the age/sex-specific numbers of prescriptions filled per patient per therapeutic category of drugs, and from changes in the age/sex-specific mix of products selected per prescription.
Unique factors that may have affected the findings in BC include the drug pricing system in Canada, the lack of the Medicare-style “doughnut hole” (Anderson et al. 2004) for the seniors benefit plan in BC, and changes in sociocultural demographics. Difference in pricing systems between Canada and the U.S. may imply that U.S. spending trends would exhibit a much greater impact from changes in the price of drugs on the market than is shown here. In Canada, such changes are now rare, owing to “frozen” prices for large public drug formularies (Morgan, Barer, and Agnew 2003). Terms of coverage for seniors are another source of potential difference in expenditure growth between BC and the U.S. The Medicare Drug Benefit contains a substantial gap in coverage (a “doughnut hole”) wherein patients must pay their own drug costs between approximately $2,000 and $5,000. No such gap in coverage existed in BC during the study period. Thus, owing to seniors' more favorable access to public subsidy in BC, the age gradient computed in this study may have been “steeper” than that which would occur in the U.S. If this were the case, age-related cost growth would be even lower in the U.S. than it has been in BC. Finally, there are other demographic changes that have not been accounted for in this study that will differ between BC, the U.S., and the rest of Canada. Notably, BC has experienced a significant immigration of population from China and South Asia over the period of study. An analysis of regional variation in BC has shown that areas that have recently experienced significant immigration from China and South Asia have lower rates of prescription drug use than other areas of the province (Morgan et al. 2005). To the extent that these regional variations owe to sociocultural background, and to the extent that BC has experienced greater than average immigration of these populations, growth in drug expenditure in BC will be lower than other regions of North America. Notwithstanding these potential sources of difference in drug utilization and expenditure, the general findings of this study are likely to be true of the U.S. and Canada.
The detailed findings of this study illustrate the value of universal drug claims data systems to help separate fact from perception for those tasked with policy and planning. Moreover, datasets such as the one used here could be used to assess drug use, safety, and outcomes in the real world with much greater detail than has been provided in this study. While further research is needed to investigate the details lying beneath the age/sex profiles computed in this study, hypotheses about the major trends emerge from the results. First, it is likely that some portion of the increased numbers of prescriptions per patient per broad therapeutic category reflects poly-therapy in the management of given conditions (e.g., using several drugs to manage asthma) as well as the treatment of multiple diagnoses that fall under the same broad therapeutic category (e.g., managing high cholesterol and high blood pressure simultaneously). Policy makers may not wish to alter such dynamics except in cases where contraindications may occur or when the benefit of treating the Nth condition of a given patient no longer justifies the cost of that treatment (Marshall 2003). Some of the increase in drug utilization per therapeutic category may also reflect better compliance with the management of chronic conditions. Trends in compliance with treatment should be studied in relation to evidence-based clinical guidelines and adherence to treatment of appropriate duration and type should be encouraged through policy.
Second, given that both the number of prescriptions filled per patient and the mix of products selected per prescription caused significant expenditure increases in the market overall and in five of the six largest therapeutic categories, the changing mix of products selected likely reflects substitutions from lower to higher cost medicines rather than a trend toward filling longer prescriptions of unchanging products. This trend deserves careful scrutiny and is a potential target for policy intervention. Substitutions from low-cost to high-cost alternatives that generate improvements in health outcomes commensurate with the relative costs should not be a policy concern. However, where expenditures escalate more rapidly than quality, policy interventions such as generic substitutions, tiered formularies, or reference pricing may be warranted.
The primary objective of this study was to isolate the impact of immutable demographic forces from the impact of utilization and expenditure dynamics that may be managed through policy. The related finding is that very little of the increase in drug expenditures in BC could be considered the inevitable result of demographics. Even as the baby boomer cohort threatens to swell the ranks of seniors entitled to public drug subsidy, the major drivers of expenditures and therefore public liability are endogenous to the pharmaceutical market. For, prevailing trends in choices concerning the quantity and type of drugs provided to people of all ages are sufficient to double age-specific drug expenditures in 10 years. Demographic change will not double the beneficiaries of seniors' drug programs for nearly 30 years (George and Statistics Canada, Demography Division 2001; U.S. Census Bureau 2004); by which time, age-specific drug expenditures per capita could be up to eight times current levels if left unchecked. The sustainability of pharmaceutical spending therefore depends not on outside forces but on decisions made by policy makers, prescribers, and patients.
Acknowledgments
This research was supported by an operating grant from the Canadian Institutes of Health Research (CIHR) and a Research Unit Award of the Michael Smith Foundation for Health Research (MSFHR). Steve Morgan is supported by a CIHR New Investigator Award and a MSFHR Scholar Award. Data were extracted with permission and assistance of the BC Ministry of Health Services and the BC College of Pharmacists. The BC College of Pharmacists and Canadian Institute for Health Information assisted with the ATC classification of over 14,000 drug products in the dataset. The views presented here are solely those of the author; the author has no disclosures.
REFERENCES
- Anderson GF, Shea DG, Hussey PS, Keyhani S, Zephyrin L. “MarketWatch: Doughnut Holes and Price Controls.”. Health Affairs (Millwood) 2004;23((Suppl. 2)):396–404. doi: 10.1377/hlthaff.w4.396. [DOI] [PubMed] [Google Scholar]
- Applied Management, Fraser Group, and Tristat Resources. Canadians' Access to Insurance for Prescription Medicines. Vol. 2. Ottawa: Health Canada, Health Transition Fund; 2000. [Google Scholar]
- Barer ML, Evans RG, Hertzman C. “Avalanche or Glacier? Health Care and the Demographic Rhetoric.”. Canadian Journal on Aging. 1995;14((2)):193–224. [Google Scholar]
- Berndt ER. “The U.S. Pharmaceutical Industry: Why Major Growth in Times of Cost Containment?”. Health Affairs. 2001;20((2)):100–14. doi: 10.1377/hlthaff.20.2.100. [DOI] [PubMed] [Google Scholar]
- British Columbia. Pharmacare Trends 2000. Victoria: Pharmacare, Ministry of Health Services; 2001. [July 23, 2003]. p. 56. [Available at http://www.hlth.gov.bc.ca/pharme/outgoing/PcareTrends2000.pdf. [Google Scholar]
- Diewert WE. “The Economic Theory of Index Numbers: A Survey.”. In: Diewert WE, Nakamura AO, editors. Essays in Index Number Theory. Vol. 1. Amsterdam: Elsevier Science; 1993. [Google Scholar]
- Evans RG. “Illusions of Necessity: Evading Responsibility for Choice in Health Care.”. Journal of Health Politics, Policy and Law. 1985;10((3)):439–67. doi: 10.1215/03616878-10-3-439. [DOI] [PubMed] [Google Scholar]
- Evans RG, McGrail KM, Morgan SG, Barer ML, Hertzman C. “APOCALYPSE NO: Population Aging and the Future of Health Care Systems.”. Canadian Journal on Aging. 2001;20((suppl 1)):160–91. [Google Scholar]
- Foot DK, Stoffman D. Boom, Bust & Echo 2000: Profiting from the Demographic Shift in the New Millennium. Toronto: Macfarlane Walter & Ross; 1998. [Google Scholar]
- Fuchs VR. “‘Though Much Is Taken’: Reflections on Aging, Health, and Medical Care.”. Milbank Memorial Fund Quarterly Health Society. 1984;62((2)):143–66. [PubMed] [Google Scholar]
- George MV Statistics Canada, Demography Division. Population Projections for Canada, Provinces and Territories, 2000–2026 (Projections démographiques pour le Canada, les provinces et les territoires, 2000–2026); Ottawa: Statistics Canada=Statistique Canada; 2001. [Google Scholar]
- Gerdtham UG, Lundin D. “Changes in Drug Spending for Different Age Groups during the 1990s? Evidence from Sweden.”. Expert Review of Pharmacoeconomics and Outcomes Research. 2004;4((3)):343–51. doi: 10.1586/14737167.4.3.343. [DOI] [PubMed] [Google Scholar]
- IMS. “Global Pharmaceutical Sales by Region, 2000–2003”. [on May 4, 2004];2004 Available at http://www.imshealth.com/ims/portal/front/indexC/0,2773,6599_5264_0,00.html.
- Marshall T. “Coronary Heart Disease Prevention: Insights from Modelling Incremental Cost Effectiveness.”. British Medical Journal. 2003;327((7426)):1264–70. doi: 10.1136/bmj.327.7426.1264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merlis M. “Explaining the Growth in Prescription Drug Spending: A Review of Recent Studies.”. Conference on Pharmaceutical Pricing Practices, Utilization and Costs; August; 2000. Report prepared for the U.S. Department of Health and Human Services. [Google Scholar]
- Metge C, Black C, Peterson S, Kozyrskyj AL. “The Population's Use of Pharmaceuticals.”. Medical Care. 1999;37((6 suppl)):JS42–59. doi: 10.1097/00005650-199906001-00008. [DOI] [PubMed] [Google Scholar]
- Morgan SG. “Quantifying Components of Drug Expenditure Inflation: The British Columbia Seniors' Drug Benefit Plan.”. Health Services Research. 2002;37((5)):1243–66. doi: 10.1111/1475-6773.01058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan SG, Barer ML, Agnew JD. “Whither Seniors' Pharmacare: Lessons from (and for) Canada.”. Health Affairs (Millwood) 2003;22((3)):49–59. doi: 10.1377/hlthaff.22.3.49. [DOI] [PubMed] [Google Scholar]
- Morgan S, Schaub P, Mooney D, Caetano P, Rahim-Jamal S, McMahon M, Yan L. “Mapping Drug Utilization Patterns: A Canadian Case Study”. 2005 Annual Research Meeting of Academy Health; Boston. 2005. [Google Scholar]
- Mueller C, Schur C, O'Connell J. “Prescription Drug Spending: The Impact of Age and Chronic Disease Status.”. American Journal of Public Health. 1997;87((10)):1626–29. doi: 10.2105/ajph.87.10.1626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reinhardt UE. “Does the Aging of the Population Really Drive the Demand for Health Care?”. Health Affairs. 2003;22((6)):27–39. doi: 10.1377/hlthaff.22.6.27. [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau. “U.S. Interim Projections by Age, Sex, Race, and Hispanic Origin”. [on Jan. 19, 2004];2004 Available at http://www.census.gov/ipc/www/usinterimproj.
- U.S.A. “Medicare Prescription Drug, Improvement, and Modernization Act.”. One Hundred Eighth Congress of the United States of America.2003. [Google Scholar]
- Van Tielen R, Peys F, Genaert J. “The Demographic Impact on Ambulatory Pharmaceutical Expenditure in Belgium.”. Health Policy. 1998;45((1)):1–14. doi: 10.1016/s0168-8510(98)00026-8. [DOI] [PubMed] [Google Scholar]
- WHO. Guidelines for ATC Classification and DDD Assignment 2004. Oslo, Norway: WHO Collaborating Centre for Drug Statistics Methodology; 2004. [Google Scholar]