Abstract
Objective
To determine whether additional risk adjustment is necessary in economic profiling of physicians when claims data are already grouped into episodes of care, and to measure effects of risk adjustment on cost efficiency rankings of physicians.
Data Sources
Four years of inpatient, outpatient, professional, and pharmacy claims data from a mixed model HMO.
Study Design
Claims data were processed through Symmetry Health Data Systems' episode treatment group (ETG) grouper to define episodes of care and Symmetry's episode risk group (ERG) software to define measures of patients' health risk scores. For each episode type (ETG), ETG-mean expected costs were calculated as the mean costs of all episodes of that type, and risk-adjusted expected costs were calculated using three alternative risk model formulations.
Data Collection
Within specialties, physicians were ranked from most cost efficient to least cost efficient, based on standardized difference between actual and expected costs. ETG-mean based rankings were compared with risk-adjusted rankings. Analyses were performed for cardiologists, family practitioners, general surgeons, and neurologists.
Principal Findings
With all three risk models, risk scores were essentially unrelated to episode costs in approximately three-fourths of episode categories (ETGs). In a sample of ETGs for which risks–costs relationships appeared to exist, split sample validation showed the relationships to be unstable or spurious in all except one ETG. Within specialties, risk-adjusted cost efficiency rankings differ little from ETG-mean adjusted rankings.
Conclusions
Depending upon the purpose for which economic profiling is performed, additional risk adjustment, beyond that already provided by episode grouping, may be unnecessary. Additional research may be needed to identify and validate ETG-level relationships between patient risks and episode costs.
Keywords: Risk adjustment, economic profiling, health care costs
After the medicare prospective payment system was introduced in the early 1980s, some hospitals—especially teaching institutions—were concerned about inadequate reimbursement for the care they delivered. This concern was prompted by findings that: (a) severity-related cost differences existed among hospitalized patients, even after controlling for diagnosis-related group (DRG) (Horn et al. 1985; McMahon and Newbold 1986; Averill et al. 1992); and, (b) within individual DRG categories, teaching hospitals treated a more severe case mix than other hospitals (Berman et al. 1986; McNeil, Kominski, and Williams-Ashman 1988).1 A similar question, based on similar assumptions, has been raised about possible bias of patient health status differences on economic profiles of physicians (Yi et al. 2002).
In economic profiling, health plans compare physicians' actual costs for services performed or ordered on behalf of patients to the expected costs of those services. Physicians whose actual costs are less than expected are considered cost efficient,2 while those whose actual costs exceed the expected values are viewed as cost inefficient. On the basis of measured cost efficiency, physicians may find their compensation rates increased or decreased (Strunk and Reschovsky 2002), their placement in provider network tiers determined (Fronstin 2003), or their continued membership in provider networks terminated.
In recent years, it has become common for health plans to use episode of care as the unit of analysis for economic profiling. Thus, the first step in economic profiling is to process a claims database through software, such as Symmetry Health Data Systems' Episode-Treatment Group (ETG) system (Symmetry Health Data Systems 2005), that aggregates groups of claims into diagnostically and chronologically related episodes. The actual cost of each defined episode is calculated as the sum of costs associated with included claims, and episode expected costs are determined, typically as the mean cost of all episodes of the same type (e.g., ETG) in the database. Once episodes and their costs are defined, responsibility for each episode is assigned to a physician. Physicians' profiles are then constructed using average actual costs and average expected costs of attributed episodes.
In economic profiling of physicians, a concern is that both (a) differences in health status among patients may influence treatment costs within defined episode types and (b) average health status of patients treated may differ significantly among physicians. As a consequence, average cost per episode may be higher for some physicians than for others, not because of poorer cost efficiency, but rather because of the poorer health status of their patients. If episode expected costs were adjusted to account for effects of differences in patient health status, the potential bias against such physicians might be removed.
The purpose of the study described here is to answer the following questions:
Are episode costs related to patient health status, and, if so, can episode expected costs be risk adjusted to account for relationships that exist?
Do cost efficiency rankings that are adjusted for patient health status differ from rankings that are not adjusted?
The first of these questions asks whether or not episode definitions themselves account adequately for relationships between patient health status and episode costs. If they do, then no additional risk adjustment is necessary. If they do not, then additional risk adjustment may be needed. Even if relationships between patient health status and episode costs exist, additional risk adjustment may not be needed if these relationships are too small and/or infrequent to influence profile rankings. This is the focus of the second question.
METHODS
Data for the project were provided by a university-owned, mixed model (group and independent practice association [IPA]) HMO in Southeast Michigan. Data included all professional, outpatient, inpatient, and pharmacy claims for members who were enrolled for the full 12 months of 1999, 2000, 2001, and/or 2002. The HMO was experiencing growth during the study years, expanding its membership, its geographic market area, and its network of physicians.
Claims data were processed through Symmetry's ETG software. The ETG system, which is widely used by health plans and other organizations for analyses of claims databases, is described by Rosen and Mayer-Oakes (1999). The resulting 4-year dataset included 658,646 completed episodes, each of which is associated with a specified member, and is characterized by: a category (ETG) and in some cases a subcategory (ETGSub), a start date, an end date, and a total cost. Episodes were divided among 693 ETG/ETGSub combinations (we will hereafter refer to these combinations simply as ETGs) and were associated with a total of 104,744 different members. Data were also processed through Symmetry's Episode-Risk Group (ERG) software to obtain member level retrospective risk scores, which can be considered measures of member health status for the periods analyzed. Separate member-level retrospective risk scores were developed for each of the 4 data years. Over the 4-year period, scores averaged 2.31 with standard deviation of 3.11, and ranged from 0 (very healthy) to 64.44 (very unhealthy). Mean annual retrospective risk scores did not differ significantly across years.
For each type of service, a standard cost was developed using all claims in the 4-year database. For professional and outpatient claims, standard costs were calculated as arithmetic averages of actual costs of claims associated with each CPT-4 procedure code (for professional claims) or HCPCS or local revenue code (for outpatient claims). Pharmacy claims costs were standardized on the basis of national drug code (NDC) and amount dispensed, and costs of inpatient admissions were standardized on the basis of DRG. (Details of cost standardization procedures are given in Thomas, Ward, and Grazier 2004.) Once costs were standardized, episode costs were calculated by summing costs of individual claims—professional, outpatient, inpatient, and pharmacy—associated with that episode.
To control for the potentially distorting effects of very high cost or very low cost episodes on estimates of physicians' mean costs, costs within ETGs were Winsorized to the second percentile of category-specific costs for low outliers; high outlier episode costs were Winsorized at the 98th percentile (Hedges and Olkin 1985).
Four different methods were used to develop expected cost estimates for episodes:3
ETG Means: Expected cost for an ETG was estimated as the average cost of all episodes in that ETG category. (This is the methodology commonly used by health plans and others when profiling physicians on the basis of episode costs.)
- One Variable Regression Model: Expected cost was estimated by regressing retrisk, (the ERG member-level retrospective risk score for the year in which the episode occurred) on episode costs. With episode as the unit of analysis, the regression equation is:
where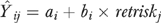
 is expected cost ETG i of member j; ai is the intercept term for ETG i, retriskj is the ERG retrospective risk score for member j, and bi is the slope coefficient of retriskk.
is expected cost ETG i of member j; ai is the intercept term for ETG i, retriskj is the ERG retrospective risk score for member j, and bi is the slope coefficient of retriskk. - Two Variable Regression Model: Expected cost was estimated by regressing retrisk and retrisk2 on episode costs. The regression equation is:
where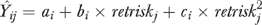
 , ai, bi, and retriskj are the same as above, retriskj2 is the square of retriskj and ci is its slope coefficient.
, ai, bi, and retriskj are the same as above, retriskj2 is the square of retriskj and ci is its slope coefficient. Dichotomized Risk Model: Within each ETG, episodes were dichotomized using mean retrisk score, and expected costs were estimated as the average cost of all episodes within each of the two subgroups.
Three alternative risk-adjustment models were examined because it was not clear, a priori, which functional form would be most appropriate. Because two of the risk-adjustment methods involved regression, analyses (and therefore expected cost estimates) were limited to ETGs for which at least 26 episodes were available in the database. Further, because we wanted to produce full-year profiles, our analyses were limited to episodes that started and ended during the same calendar year.4 With these two sets of restrictions, the final, 4-year analysis dataset included 595,425 episodes, representing 457 ETGs and a total of 104,335 members. Among the 457 ETGs, 106 included 1,000 or more episodes, 62 included 500–999 episodes, 160 included 100–499 episodes, and 129 included 99 or fewer episodes.
The three retrospective risk-based risk-adjustment models were compared on the basis of strength and stability of relationships between patient retrospective risk score and episode costs. Strength of relationship was indicated by R2 value—regression-adjusted R2 for the regression based models and squared correlation between actual and expected costs for the dichotomized risk model.5 Relationship stability was assessed using split sample analysis for selected ETGs, with the first half of the sample used for estimating risk–cost relationships, and the second half used for validation testing of those relationships. ETG selection for these analyses was based on strength of risk–cost relationships (both one-variable and two-variable regression model R2≥0.05) and volume of episodes (the 12 largest volume ETGs satisfying the R2 requirement were selected).
Many episodes involved services and charges, from multiple physicians. But profiling requires that, when possible, responsibility for each episode be assigned to a single physician. Health plans have used a variety of decision rules for determining which physician, among those participating in an episode of care, should be assigned overall responsibility for episode associated costs. In this study, we used the following rule: responsibility for each episode's actual and expected costs was attributed to the physician who accounted for 50 percent of more of episode-related professional and prescribing costs. If no one physician accounted for at least 50 percent of professional and prescribing costs, the episode was not assigned.
After episode responsibility was assigned, physicians were ranked within specialties from most cost efficient to least cost efficient on the basis of standardized cost difference, which is the standardized difference between average actual cost and average expected cost for the sample of episodes managed by the physician. Using Zkj to represent the standardized cost difference for the kth physician according to the jth model,
where yk is average actual costs associated with the kth physician's set of episodes,  is the average expected costs associated with these episodes according to the jth model, σj is the standard deviation of episode expected costs according to the jth model, and Nk is the number of episodes assigned to the kth physician. As we have shown (Thomas, Grazier, and Ward 2004), this measure is less likely than those that do not adjust for sample size to incorrectly identify smaller sized panels as high or low outliers.
is the average expected costs associated with these episodes according to the jth model, σj is the standard deviation of episode expected costs according to the jth model, and Nk is the number of episodes assigned to the kth physician. As we have shown (Thomas, Grazier, and Ward 2004), this measure is less likely than those that do not adjust for sample size to incorrectly identify smaller sized panels as high or low outliers.
As a measure of agreement between alternative model rankings, we used the weighted κ statistic proposed by Landis and Koch (1977), who indicate that appropriate interpretation of weighted κ values, which vary from 0.0 to 1.0, would be: 0–20 percent, slight agreement; 21–40 percent, fair agreement; 41–60 percent, moderate agreement; and 61 percent and greater, substantial agreement. For our weighted κ analyses, we partitioned physician rankings into quintiles, and measured level of agreement between pairs of quintile rankings.
Analyses included all physicians within a specialty who satisfied a specified minimum episode sample size criterion. In this paper, we show findings for economic profile rankings in four clinical specialties: cardiology, family practice, general surgery, and neurology. Based on results provided elsewhere (Thomas 2005), we profiled and ranked cardiologists having 20 or more attributed episodes, family practitioners with at least 125 episodes, general surgeons and neurologists with at least 25 episodes.6
RESULTS
Table 1 presents data on strength of relationships between episode costs and patient retrospective risk scores. R2 values shown in this table are adjusted R2 for each of the two regression models and squared correlations between actual and expected costs for the dichotomized model. (For the first model, R2 would be, by definition, equal to 0.) The data show that none of the three risk models is explain more than a marginal amount of within-ETG cost variation (R2≤0.025) for approximately three-fourths of ETG categories. Summing the last two rows for each model shows that, with one-variable regression models, in only 6 percent of ETGs are R2 values greater than 0.10; with two-variable regression models, R2 values are greater than 0.10 for 8 percent of ETGs, and for dichotomous models, R2 exceeds 0.10 in 4 percent of ETGs. The relatively small proportions of ETGs exhibiting even moderate risks–costs relationships suggest that Symmetry's ETG grouper performs well at defining episode categories in which patient health status exerts relatively little influence on diagnostic and treatment costs. Nevertheless, patient health status appears to be related to episode costs in some ETGs. Table 1 indicates that retrospective risk has at least a slight relationship (R2>0.025) with episode costs in 22 percent of ETGs for one-variable regressions, 26 percent of ETGs for dichotomized model risk adjustment, and for 30 percent of ETGs for two-variable regressions. These ETGs account for 13.7, 6.6, and 16.7 percent, respectively, of all episodes in the study population.
Table 1.
Number of ETGs with Risk Adjustment R2 in Specified Range, by Risk-Adjustment Model
| Number of Episodes per ETG | ||||||
|---|---|---|---|---|---|---|
| Risk-Adjustment Model | R2 | Number of ETDs | Percent of ETGs | Minimum | Average | Maximum |
| One-variable regression | ≤0.01 | 271 | 0.59 | 25 | 1,400.8 | 70,426 |
| ≤0.01≤0.025 | 85 | 0.19 | 28 | 1,567.5 | 18,208 | |
| ≤0.025≤0.05 | 49 | 0.11 | 28 | 1,388.6 | 14,745 | |
| ≤0.05≤0.075 | 19 | 0.04 | 30 | 380.7 | 3,170 | |
| ≤0.075≤0.10 | 4 | 0.01 | 46 | 245.0 | 800 | |
| ≤0.10≤0.15 | 15 | 0.03 | 38 | 340.3 | 1,627 | |
| ≤0.15 | 14 | 0.03 | 26 | 54.6 | 114 | |
| Two-variable regression | ≤0.01 | 228 | 0.50 | 25 | 1,477.1 | 70,426 |
| ≤0.01≤0.025 | 91 | 0.20 | 32 | 1,745.3 | 21,979 | |
| ≤0.025≤0.05 | 67 | 0.15 | 30 | 1,225.3 | 14,745 | |
| ≤0.05≤0.075 | 26 | 0.06 | 28 | 310.6 | 3,170 | |
| ≤0.075≤0.10 | 5 | 0.01 | 53 | 357.0 | 1,331 | |
| ≤0.10≤0.15 | 20 | 0.04 | 28 | 302.7 | 1,627 | |
| ≤0.15 | 20 | 0.04 | 26 | 68.1 | 279 | |
| Dichotomous risk score | ≤0.01 | 224 | 0.49 | 25 | 1,775.8 | 70,426 |
| ≤0.01≤0.025 | 116 | 0.25 | 25 | 1,359.2 | 18,208 | |
| ≤0.025≤0.05 | 58 | 0.13 | 28 | 544.3 | 4,514 | |
| ≤0.05≤0.075 | 30 | 0.07 | 25 | 212.6 | 1,627 | |
| ≤0.075≤0.10 | 11 | 0.02 | 30 | 61.2 | 149 | |
| ≤0.10≤0.15 | 8 | 0.02 | 28 | 66.0 | 104 | |
| ≤0.15 | 10 | 0.02 | 26 | 38.5 | 59 | |
ETG, episode treatment group.
To test stability of the risk-adjustment models, we selected 12 ETGs according to the criteria specified above. The ETGs are shown in Table 2. In each of these ETG categories, half of the episodes were used to estimate relationships between retrospective risk and episode costs. Estimation R2 values suggest that modeled retrospective risk relationships are modestly predictive of episode costs in every ETG category considered. Weighted average difference between estimation and validation R2 values is smallest for the two-variable regression model. However, even with this model, differences within individual ETGs are quite large—greater than 30 percent in 10 of the 12 ETGs listed. We cannot attribute these relatively poor validity results to the small size of the database used for the project, as ETG volume appears to be unrelated to risk model validation results. In the absence of validity evidence, we must consider that many, if not all, of the ETG-level risks–costs relationships are spurious.
Table 2.
Split Sample Stability Analysis of Three Risk-Adjustment Models for Selected ETGs
| One-Variable Regression Models | Two-Variable Regression Models | Dichotomized Models | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| ETG | Total Number of Episodes | Estimation R2 | Validation R2 | Percent Difference (%) | Estimation R2 | Validation R2 | Percent Difference (%) | Estimation R2 | Validation R2 | Percent Difference (%) |
| (a) Comparison of estimation and validation R2values | ||||||||||
| 0005 | 523 | 0.136 | 0.080 | 41 | 0.134 | 0.082 | 39 | 0.061 | 0.019 | 69 |
| 0032 | 377 | 0.161 | 0.022 | 86 | 0.157 | 0.022 | 86 | 0.023 | 0.014 | 38 |
| 0076 | 3,170 | 0.052 | 0.072 | −38 | 0.053 | 0.069 | −30 | 0.036 | 0.016 | 56 |
| 0310 | 284 | 0.046 | 0.181 | −293 | 0.050 | 0.032 | 36 | 0.038 | 0.012 | 69 |
| 0373 | 662 | 0.171 | 0.111 | 35 | 0.169 | 0.111 | 34 | 0.038 | 0.103 | −171 |
| 0374 | 1,627 | 0.147 | 0.059 | 60 | 0.149 | 0.069 | 54 | 0.046 | 0.065 | −39 |
| 0399 | 370 | 0.077 | 0.056 | 27 | 0.080 | 0.058 | 27 | 0.034 | 0.047 | −39 |
| 0450 | 1,331 | 0.065 | 0.073 | −12 | 0.066 | 0.100 | −52 | 0.031 | 0.036 | −14 |
| 0645 | 582 | 0.029 | 0.104 | −259 | 0.099 | 0.000 | 100 | 0.027 | 0.034 | −25 |
| 0737 | 279 | 0.11 | 0.168 | −50 | 0.140 | 0.249 | −78 | 0.010 | 0.047 | −384 |
| 0799 | 423 | 0.188 | 0.084 | 55 | 0.235 | 0.026 | 89 | 0.032 | 0.011 | 64 |
| 0812 | 800 | 0.100 | 0.096 | 4 | 0.098 | 0.096 | 2 | 0.033 | 0.077 | −133 |
| Weighted average percent difference | −17 | 9 | −16 | |||||||
| Episode Cost Range ($) | ||||
| ETG | ETG Name | Minimum | Mean | Maximum |
| (b) Selected high volume ETGs | ||||
| 0005 | Major infectious disease except HIV and septicemia, w/o comorbidity | 13 | 396 | 4,204 |
| 0032 | Benign endocrine disorders of the pancreas | 4 | 299 | 11,193 |
| 0076 | Non-neoplastic blood disease, minor | 5 | 456 | 6,549 |
| 0310 | Other diseases of the veins | 10 | 243 | 2,702 |
| 0373 | Bacterial lung infections, with comorbidity | 40 | 1,624 | 16,974 |
| 0374 | Bacterial lung infections, w/o comorbidity | 40 | 635 | 6,037 |
| 0399 | Other inflammatory lung disease, w/o surgery | 21 | 1,334 | 22,617 |
| 0450 | Other infectious diseases of the intestines and abdomen | 21 | 346 | 3,425 |
| 0645 | Malignant neoplasm of the female genital tract, w/o surgery | 34 | 1,835 | 45,456 |
| 0737 | Closed fracture or dislocation of trunk, w/o surgery | 32 | 795 | 7,871 |
| 0799 | Minor specific procedures not classifed elsewhere | 10 | 295 | 6,952 |
| 0812 | Poisonings and toxic effects of drugs | 21 | 756 | 7,392 |
Even if our analyses had validated all of the estimated relationships, the question of whether or not the frequency and strength of such relationships are sufficient to affect physicians' profile rankings would remain. If rankings are unaffected, then additional risk adjustment, beyond episode grouping, would be unnecessary. If risks–costs relationships exist and do affect judgments about physicians' relative cost efficiency performance, additional risk adjustment in profiling analyses should be performed. While we are unable to validate the existence of most ETG-level risks–costs relationships, we can investigate implications of those relationships, under the assumption that they do in fact exist.
Differences among risk-adjusted cost efficiency rankings are shown in Table 3 for four specialties in each of 4 years7. In all cases, weighted κ values in this table indicate substantial agreement between the rankings based on ERG risk scores and the rankings based on ETG means. Although agreement between pairs of rankings in most cases is not perfect (i.e., weighted κ<1.0), weighted κ values are high in the substantial agreement range for all risk-adjustment models, indicating that for these four specialties risk-score-based and ETG-mean-based rankings are very similar.
Table 3.
Level of Agreement between ETG-Mean Adjusted and Risk-Adjusted Cost Efficiency Rankings for Four Specialties, by Year
| Risk Adjusted with One-Variable Regression Model | Risk Adjusted with Two-Variable Regression Model | Risk Adjusted with Dichotomized Model | ||||||
|---|---|---|---|---|---|---|---|---|
| Specilty* | Year | Number of physicions | Percent Cases in ETGs with R2>.025 (%)† | Weighted Kappa‡ | Percent Cases in ETGs with R2>.025 (%)† | Weighted κ‡ | Percent Cases in ETGs with R2>.025 (%)† | Weighted κ‡ |
| Cardiology(N≥20) | 1999 | 4 | 0.0 | 1.00 | 0.0 | 1.00 | 0.0 | 1.00 |
| 2000 | 11 | 2.3 | 0.68 | 2.3 | 0.76 | 2.3 | 0.76 | |
| 2001 | 14 | 5.3 | 0.80 | 5.3 | 0.80 | 5.3 | 0.90 | |
| 2002 | 11 | 0.7 | 0.87 | 0.7 | 0.87 | 0.7 | 0.87 | |
| Family Practice(N≥125) | 1999 | 18 | 14.6 | 0.88 | 14.6 | 0.88 | 0.0 | 0.88 |
| 2000 | 30 | 15.9 | 0.69 | 15.9 | 0.65 | 3.0 | 0.64 | |
| 2001 | 41 | 14.4 | 0.75 | 14.4 | 0.70 | 2.9 | 0.75 | |
| 2002 | 45 | 13.9 | 0.80 | 13.9 | 0.76 | 0.7 | 0.80 | |
| General Surgery(N≥25) | 1999 | 2 | 25.9 | 1.00 | 25.9 | 1.00 | 25.9 | 1.00 |
| 2000 | 9 | 14.6 | 0.94 | 14.6 | 0.94 | 14.6 | 0.94 | |
| 2001 | 9 | 9.6 | 0.94 | 9.6 | 0.94 | 9.6 | 0.94 | |
| 2002 | 9 | 14.2 | 1.00 | 14.2 | 1.00 | 14.2 | 1.00 | |
| Neurology(N≥25) | 1999 | 4 | 1.1 | 1.00 | 1.1 | 1.00 | 1.1 | 1.00 |
| 2000 | 10 | 6.2 | 0.70 | 7.7 | 0.70 | 6.2 | 0.70 | |
| 2001 | 11 | 3.5 | 0.97 | 5.0 | 0.97 | 3.2 | 0.97 | |
| 2002 | 11 | 2.7 | 0.76 | 3.0 | 0.76 | 1.4 | 0.76 | |
N refers to minimum number of episodes required for physician profiles.
Full sample estimation R2 values.
Measuring level of agreement between risk-adjusted rankings and ETG-mean adjusted rankings.
ETG, episode treatment group.
No episodes used in Table 3 analyses were in ETGs for which full sample estimation R2≥0.05 for any of the risk models. However, a number of episodes used in these profiles were in ETGs for which patient risk was marginally related to episode cost (ETGs with risk model 0.025<R2≤0.05). It might reasonably be assumed that lower weighted κ values would be associated with larger proportions of physicians' episodes in ETGs with higher R2 values. However, Table 3 demonstrates that this assumption is incorrect. For all three types of models, there appears to be no relationship between weighted κ scores and percentages of cases in ETGs with R2 values>0.025.
To better understand the meaning of “substantial agreement” between risk-score adjusted and ETG-mean adjusted cost efficiency rankings, in Table 4 we show data for the 14 cardiologists who had 20 or more attributed episodes during 2001. Several interesting patterns can be observed in these data. First, it is clear that the physicians identified as most cost efficient with ETG-mean adjusted expected costs remain as most cost efficient when expected costs are based on risk score calculations. Rankings of several of the six most cost efficient cardiologists change when expected costs are risk adjusted, but these six continue to be identified as the most cost efficient of the 14 physicians profiled. At the bottom of the cost efficiency rankings, five of the six cardiologist identified as least cost efficient remain at the bottom of the distribution when expected episode costs are adjusted to account for patient risk. The sole exception is physician K who is ranked 11th with ETG-mean adjustment and is replaced by physician G in all risk-adjusted cost efficiency rankings.
Table 4.
Cost Efficiency Rank, by Risk-Adjustment Method: Cardiologists with≥20 Episodes, Year=2001
| Risk Adjusted with ETG Means | Risk Adjusted with One-Variable Regression Model | Risk Adjusted with Two-Variable Regression Model | Risk Adjusted with Dichotomized Model | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Provider | Number of Episodes | Avg Risk | Avg Actual Cost | Avg. Exp. Cost | Std. Cost Dif. | Eff. Rank | Avg. Exp. Cost | Std. Cost Dif. | Eff. Rank | Avg. Exp. Cost | Std. Cost Dif. | Eff. Rank | Avg. Exp. Cost | Std. Cost Dif. | Eff. Rank |
| A | 37 | 4.2 | $1,604 | $3,538 | −4.381 | 1 | $2,379 | −2.553 | 1 | $2,440 | −2.756 | 1 | $2,454 | −2.808 | 1 |
| B | 32 | 3.7 | $1,135 | $2,101 | −2.033 | 2 | $1,285 | −0.458 | 4 | $1,306 | −0.523 | 4 | $1,324 | −0.581 | 3 |
| C | 23 | 2.9 | $854 | $1,945 | −1.947 | 3 | $1,175 | −0.835 | 2 | $1,176 | −0.837 | 2 | $1,157 | −0.789 | 2 |
| D | 70 | 3.1 | $740 | $1,041 | −0.940 | 4 | $872 | −0.600 | 3 | $891 | −0.686 | 3 | $831 | −0.416 | 4 |
| E | 27 | 4.1 | $1,450 | $1,824 | −0.723 | 5 | $1,259 | 0.538 | 6 | $1,261 | 0.532 | 6 | $1,361 | 0.253 | 5 |
| F | 28 | 4.8 | $1,467 | $1,768 | −0.591 | 6 | $1,362 | 0.301 | 5 | $1,407 | 0.172 | 5 | $1,316 | 0.436 | 6 |
| G | 33 | 2.2 | $1,485 | $1,420 | 0.140 | 7 | $961 | 1.631 | 10 | $978 | 1.580 | 10 | $1,048 | 1.365 | 9 |
| H | 71 | 2.1 | $800 | $731 | 0.216 | 8 | $576 | 1.022 | 7 | $583 | 0.988 | 7 | $590 | 0.960 | 7 |
| I | 20 | 2.0 | $1,366 | $1,177 | 0.314 | 9 | $754 | 1.483 | 9 | $744 | 1.506 | 9 | $761 | 1.470 | 10 |
| J | 61 | 1.9 | $1,248 | $1,139 | 0.317 | 10 | $818 | 1.817 | 11 | $796 | 1.910 | 11 | $820 | 1.814 | 11 |
| K | 24 | 2.5 | $1,098 | $799 | 0.545 | 11 | $693 | 1.075 | 8 | $703 | 1.047 | 8 | $697 | 1.067 | 8 |
| L | 51 | 2.6 | $1,838 | $1,345 | 1.310 | 12 | $956 | 3.410 | 12 | $953 | 3.423 | 12 | $938 | 3.489 | 12 |
| M | 60 | 3.2 | $2,017 | $1,440 | 1.664 | 13 | $1,045 | 4.077 | 14 | $1,055 | 4.039 | 14 | $977 | 4.376 | 14 |
| N | 70 | 3.2 | $2,049 | $1,454 | 1.855 | 14 | $1,158 | 4.038 | 13 | $1,184 | 3.922 | 13 | $1,110 | 4.268 | 13 |
Avg, average; Std. Cost. Dif., standardized cost difference; Eff., efficiency; Exp., expected.
Table 4 also shows that physicians' average actual episode costs are not predictive of cost efficiency rankings, regardless of risk adjustment methodology. Average actual costs for physicians C and D, who are ranked second, third, or fourth depending upon risk-adjustment model, are among the lowest for the 14 cardiologists, while average actual cost for physician A, who is ranked first in cost efficiency by all models, is relatively high compared with those of the other physicians. Neither are average risk scores determinant of physicians' cost efficiency rankings. Physicians M and N, ranked last (13th and 14th) by all models, have higher average risk scores than 8 and lower average risk scores than 4 of the other profiled physicians. It is not actual costs or risk scores, but rather relationships between expected and actual episode costs that determine physicians' cost efficiency rankings. Table 4 shows that expected cost estimates based on ETG means are generally similar to those based on the various risk score models. With all risk-adjustment methodologies, physician A has the largest and physician H the smallest average expected costs. For two of the risk-adjustment methodologies—ETG-means and dichotomized model—five of the six largest average expected cost values are associated with physicians A through F, while for each of the two regression-based risk-adjustment methodologies four of the six largest average expected cost values are associated with these physicians.
Although not presented here, ranking statistics for family practitioners, general surgeons, and neurologists show similar patterns to those in Tables 4.8 Adjustment for relationships between retrospective risk and episode costs leads to small alterations in cost efficiency rankings with all models, but no major shifts in relative rankings occur.
DISCUSSION AND CONCLUSION
In this study, we examined four different methodologies for estimating episode expected costs. Although all risk-adjusted rankings were in substantial—and in some cases perfect—agreement with ETG-mean based rankings, differences did exist. Of the risk-adjustment methodologies considered, two-variable regression produced the strongest relationships between retrospective risk and episode costs. However, even with the two-variable regression model, essentially no relationship was found between patient health status and episode costs in approximately three-quarters of symmetry's ETG categories. In less than 10 percent of ETGs do risks–costs relationships produce R2 values that exceed 0.10. Furthermore, with all models, split sample validation indicates instability, and possibly spuriousness, in most modeled relationships.
Other findings of this study can be summarized as follows:
Symmetry Health Data System's ETG grouper classifies health care claims into episode groupings in which patient health status exerts relatively little influence on diagnostic and treatment costs. For all three of the risk models considered in this study, none of the economic profiles in any of the four specialties included ETG categories for which risk–cost model R2 values were 0.05 or higher.
No relationship was found between percentage of episodes in ETG categories with nonzero risks–costs relationships and the likelihood that risk adjustment will cause changes in physicians' cost efficiency rankings.
Physicians' cost efficiency rankings are not biased with respect to average retrospective risk score of patients treated. This is true even when episode expected costs are based on ETG means. Thus, the “my patients are sicker” argument cannot be used credibly to explain substandard cost efficiency performance.
Risk-adjusted cost efficiency rankings agree substantially with ETG-means based rankings, for all years and all four specialties examined. In several cases, there was perfect agreement between pairs of rankings.
When changes in rankings occurred because of risk adjustment, changes were small. Specific changes in rankings differed with different risk models.
When evaluating cost efficiency performance of network physicians, health plans typically compare actual costs of services provided or ordered by each physician to the costs expected for those services, given the types of episodes being managed. Expected costs of episodes are calculated as average actual costs of all episodes of the same type (i.e., ETG) in the claims dataset being analyzed. With nominal cost standards such as these, performance assessments depend not only on the claims for which physicians are themselves responsible, but also on other claims in the dataset, as these other claims help determine episode expected costs. Use of nominal cost standards might also suggest that if additional risk adjustment is to be performed, ETG-level risk–costs relationships should be estimated in the dataset being analyzed. However, we found that most of the risks–costs relationships estimated with a 4-year database from a small HMO are spurious or unstable, in that, if they exist at all, the relationships almost certainly are sensitive to inclusion or exclusion of small numbers of episodes in profiling analyses. To protect against such sensitivity, risk-adjustment, if performed, should utilize validated risk models, and this suggests that models must be estimated and validated with datasets larger than that used in this study. If externally estimated and validated models are used in when profiling physicians, episode expected costs will still be nominal because models will be recalibrated to the dataset being analyzed.
A possible concern related to generalizability of our findings is that our analyses were based on only one patient risk measure, the ERG retrospective risk score. We have shown in an earlier study (Thomas, Grazier, and Ward 2004) that this measure produces similar profiling results to those obtained with other commonly used risk measures (e.g., Adjusted Clinical Groups [ACGs] from Johns Hopkins University and Diagnostic Cost Groups [DCGs] from DxCG Inc.). For the current study, in addition to developing health plan members' ERG retrospective risk scores, we also processed the database thorough DCG software from DxCG Inc. For each of the four data years, we found ERG and DCG retrospective risk measures to be highly correlated (average r=0.75 over the 4-year period), and we are confident that our findings on risk adjustment would have been similar had we utilized the DCG risk measure instead of the ERG risk measure in our analyses.
Another issue regarding the generalizability of out findings—and this is an important caveat—is that our analyses were performed on data from a single, university-owned health plan. We do not know whether or not the strength and stability of within-ETG risks–costs relationships would be similar if estimated in different datasets. Similarly, it is possible that effects of such relationships on cost efficiency rankings could be greater or lesser than shown here. We believe that a priority for future research should be investigation of these relationships in large datasets.
Acknowledgments
This study was supported by Grant 047789 from the Robert Woods Johnson Foundation Health Care Financing and Organization (HCFO) Program.
NOTES
Other research has suggested that, controlling for DRG, teaching institutions do not, in fact, treat more severely ill patients than nonteaching hospitals (Welch 1987; Goldfarb and Coffey 1987).
A consensus conference convened in September 2005 by the Ambulatory Care Quality Alliance and National Committee for Quality Assurance determined that the relative-resource-use measure described in this paper should be termed cost efficiency, and that this should be differentiated from efficiency, a term long used by economist to refer to the cost of resources utilized in achieving a given outcome or benefit to the patient.
To control for skewness in episode cost distributions, in preliminary analyses, we estimated risk models using log transform of episode costs as the dependent variable. Findings from subsequent analyses using transformed actual and expected cost estimates did not differ greatly from those based on untransformed data, and as a result are not presented here. Results of these analyses are available from the author upon request.
The 595,425 single year episodes represented 89.1 percent of the total 668,234 episodes in the database. Among episodes that began in one year and ended in a different year (10.8 percent of the total), the most frequently occurring conditions were benign hypertension (ETG 0281), hyperlipidemia (ETG 0047), and minor depression (ETG 0096). Including these cross-year episodes in our analyses would have required estimating cross-year retrospective risk scores, for example by calculating simple or time-weighted averages of single year risk scores. Because within-ETG relationships between these calculated risk scores and episode costs might be different than risk adjustment relationships for single year single year episodes, we chose to exclude cross-year episodes from our analyses.
For the dichotomized risk model, R2 is calculated as 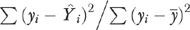 where yi is actual cost of episode i,
where yi is actual cost of episode i,  is expected cost of episode i, and
is expected cost of episode i, and  is mean actual cost of all episodes within the ETG.
is mean actual cost of all episodes within the ETG.
Analyses were also performed with other minimum sample sizes for each specialty. Results were similar to those reported below for the minimum sample sizes specified here.
Number of episodes per physician for profiles represented in Table 3 ranged from 20 to 105, with mean=47.1 for cardiologists; from 125 to 418, with mean=190.5 for family practitioners; from 25 to 89, with mean=44.7 for general surgeons; and from 25 to 163, with mean=54.1 for neurologists.
Tables are available from the authors upon request.
REFERENCES
- Averill RF, McGuire TE, Manning BE, Fowler DA, Horn SD, Dickson PS, Coye MJ, Knowlton DL, Bender JA. “A Study of the Relationship between Severity of Illness and Hospital Cost in New Jersey Hospitals.”. Health Services Research. 1992;27((5)):587–606. [PMC free article] [PubMed] [Google Scholar]
- Berman RA, Green J, Kwo D, Safian KF, Botnick L. “Severity of Illness and the Teaching Hospital.”. Journal of Medical Education. 1986;61((1)):1–9. doi: 10.1097/00001888-198601000-00001. [DOI] [PubMed] [Google Scholar]
- Fronstin P. Tiered Networks for Hospital and Physician Health Care Services. Washington, DC: Employee Benefits Research Institute; Auguest 2003. EBRI Issue Brief Number 260. [PubMed] [Google Scholar]
- Goldfarb MG, Coffey RM. “Case-Mix Differences between Teaching and Nonteaching Hospitals.”. Inquiry. 1987;24((1)):68–84. [PubMed] [Google Scholar]
- Hedges LV, Olkin I. Statistical Methods for Meta-Analysis. Orlando, FL: Academic Press; 1985. [Google Scholar]
- Horn SD, Bulkley G, Sharkey PD, Chambers AF, Horn RA, Schramm CJ. “Inter-Hospital Differences in Severity of Illness. Problems for Prospective Payment Based on Diagnosis-Related Groups (DRGs).”. New England Journal of Medicine. 1985;313((1)):20–4. doi: 10.1056/NEJM198507043130105. [DOI] [PubMed] [Google Scholar]
- Landis JR, Koch GG. “The Measurement of Observer Agreement for Categorical Data.”. Biometrica. 1977;33:159–74. [PubMed] [Google Scholar]
- McMahon LF, Jr, Newbold R. “Variation in Resource Use within Diagnosis-Related Groups. The Effects of Severity of Illness and Physician Practice.”. Medical Care. 1986;24((5)):388–97. doi: 10.1097/00005650-198605000-00002. [DOI] [PubMed] [Google Scholar]
- McNeil BJ, Kominski GF, Williams-Ashman A. “Modified DRGs as Evidence of Variability in Patient Severity.”. Medical Care. 1988;26((1)):53–61. doi: 10.1097/00005650-198801000-00006. [DOI] [PubMed] [Google Scholar]
- Rosen AK, Mayer-Oakes A. “Episodes of Care: Theoretical Frameworks versus Current Operational Realities.”. Journal on Quality Improvement. 1999;25((3)):111–28. doi: 10.1016/s1070-3241(16)30431-x. [DOI] [PubMed] [Google Scholar]
- Strunk BC, Reschovsky JD. Center for the Study of Health System Change (CSHSC); 2002. “Kinder and Gentler: Physicians and Managed Care, 1997–2001.”. Tracking Report: Results from the Community Tracking Study. No. 5. [PubMed] [Google Scholar]
- Symmetry Health Data Systems. “Episode Treatment Groups: An Illness Classification and Episode Building System.”. 2005 Available at http://www.symmetry-health.com/ETGTut_Desc1.htm.
- Thomas JW. Portland, ME: Institute for Health Policy, Muskie School of Public Service, University of Southern Maine; 2005. “Sample Size Considerations in Economic Profiling of Physician Specialists.”. [Google Scholar]
- Thomas JW, Grazie KL, Ward K. “Economic Profiling of Primary Care Physicians: Consistency among Risk Adjusted Measures.”. Health Services Research. 2004;39:985–1004. doi: 10.1111/j.1475-6773.2004.00268.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas JW, Grazier KL, Ward K. “Comparing Accuracy of Risk Adjustment Methodologies Used in Economic Profiling of Physicians.”. Inquiry. 2004;41:218–31. doi: 10.5034/inquiryjrnl_41.2.218. [DOI] [PubMed] [Google Scholar]
- Thomas JW, Ward K, Grazier KL. Portland, ME: Institute for Health Policy, Muskie School for Public Service, University of Southern Maine; 2004. “Using Physician Profiling Software to Evaluate the Practice Efficiency of Physician Specialists.”. Final Report to the Robert Wood Johnson Foundation Health Care Organization and Financing Program Grant #047789. [Google Scholar]
- Welch WP. “Do All Teaching Hospitals Deserve an Add-On Payment under the Prospective Payment System?”. Inquiry. 1987;24((3)):221–32. [PubMed] [Google Scholar]
- Yi R, Haughton J, Cecere F, Rubin M. Boston: AdvanceMed. Inc. and DxCG Inc; 2002. “Integration of Episode Analysis and Risk Assessment for Provider Profiling.”. [Google Scholar]


