Abstract
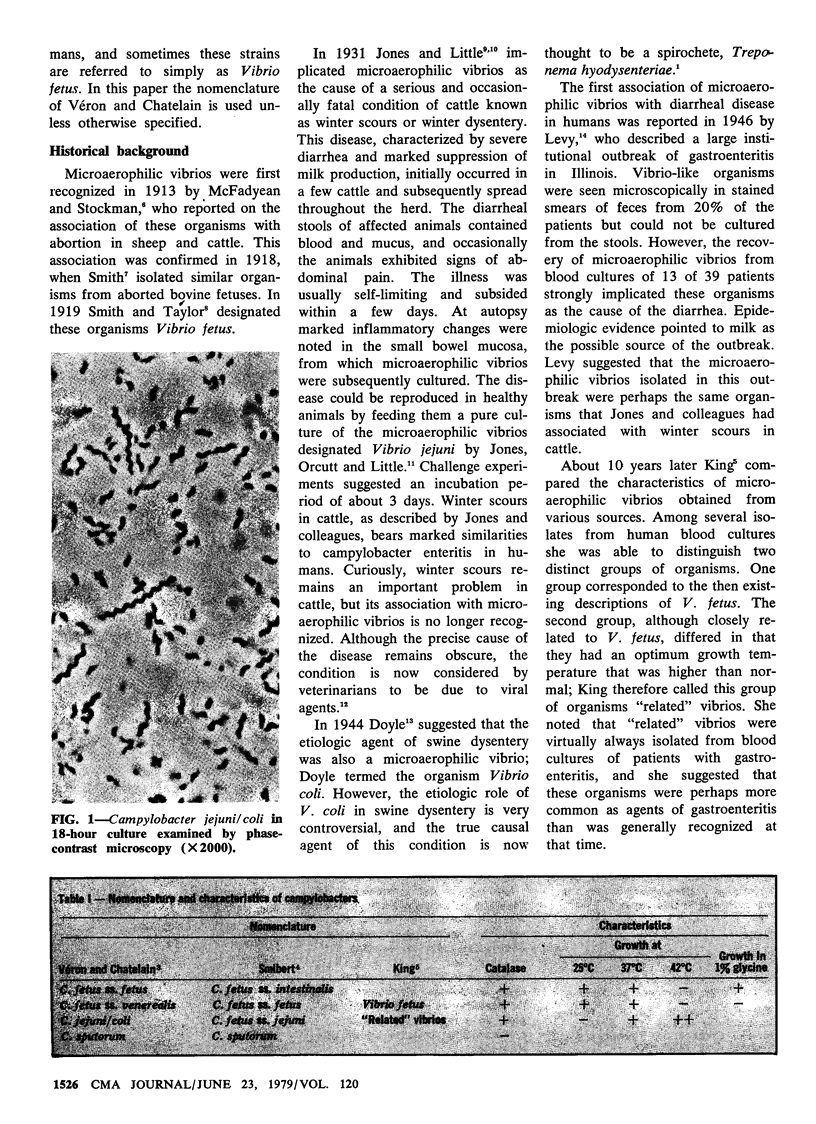
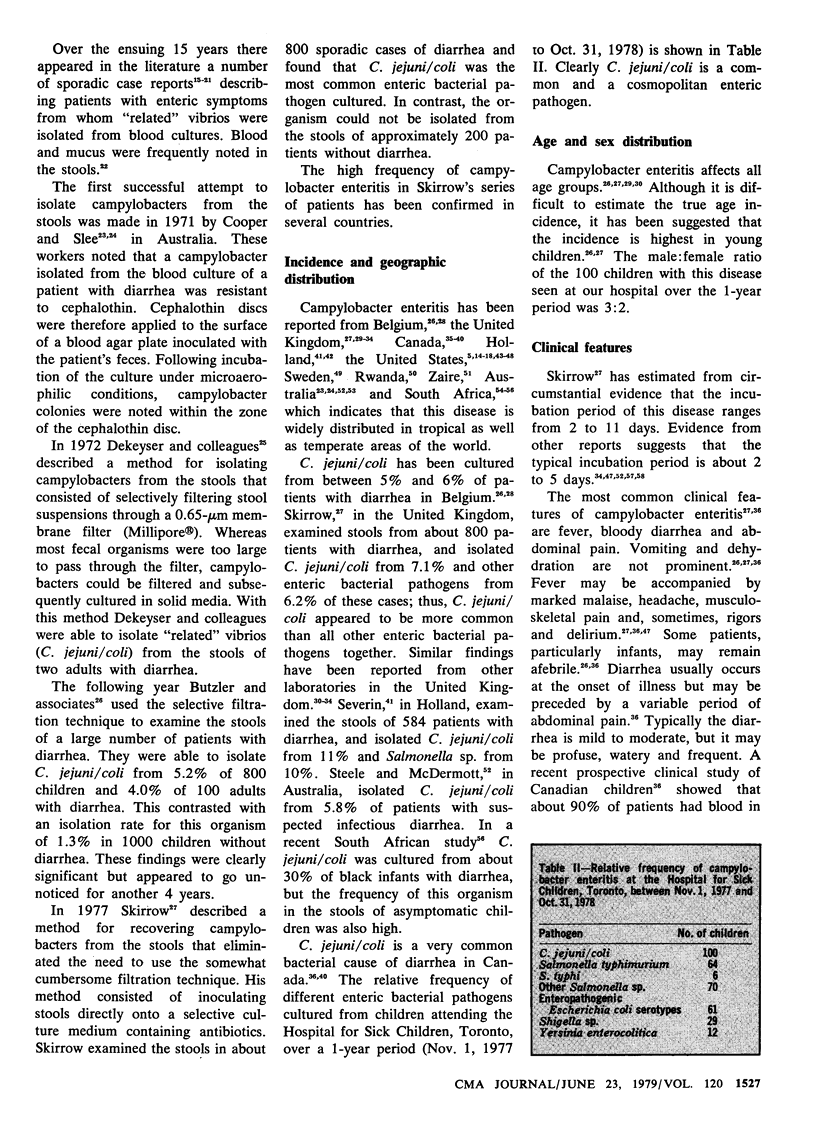
Campylobacter jejuni/coli has recently become recognized as a common bacterial cause of diarrhea. Infection can occur at any age. The usual incubation period of campylobacter enteritis is 2 to 5 days. Fever, diarrhea and abdominal pain are the most common clinical features. The stools frequently contain mucus and, a few days after the onset of symptoms, frank blood. Significant vomiting and dehydration are uncommon. A rapid presumptive laboratory diagnosis may be made during the acute phase of the illness by direct phase-contrast microscopy of stools. Isolation of the organism from stools requires culture in a selective medium containing antibiotics and incubation under reduced oxygen tension at 42 degrees C. The organism persists in the stools of untreated patients for up to 7 weeks following the onset of symptoms. Erythromycin may produce a rapid clinical and bacteriologic cure, and should be used to treat moderately to severely ill patients as well as patients with compromised host defences. The emergence of erythromycin-resistant strains requires close monitoring. The epidemiologic aspects of campylobacter enteritis will be fully understood only when methods become available for differentiating strains of C. jejuni/coli. The historical background and current knowledge of campylobacter enteritis are reviewed in this paper.
Full text
PDF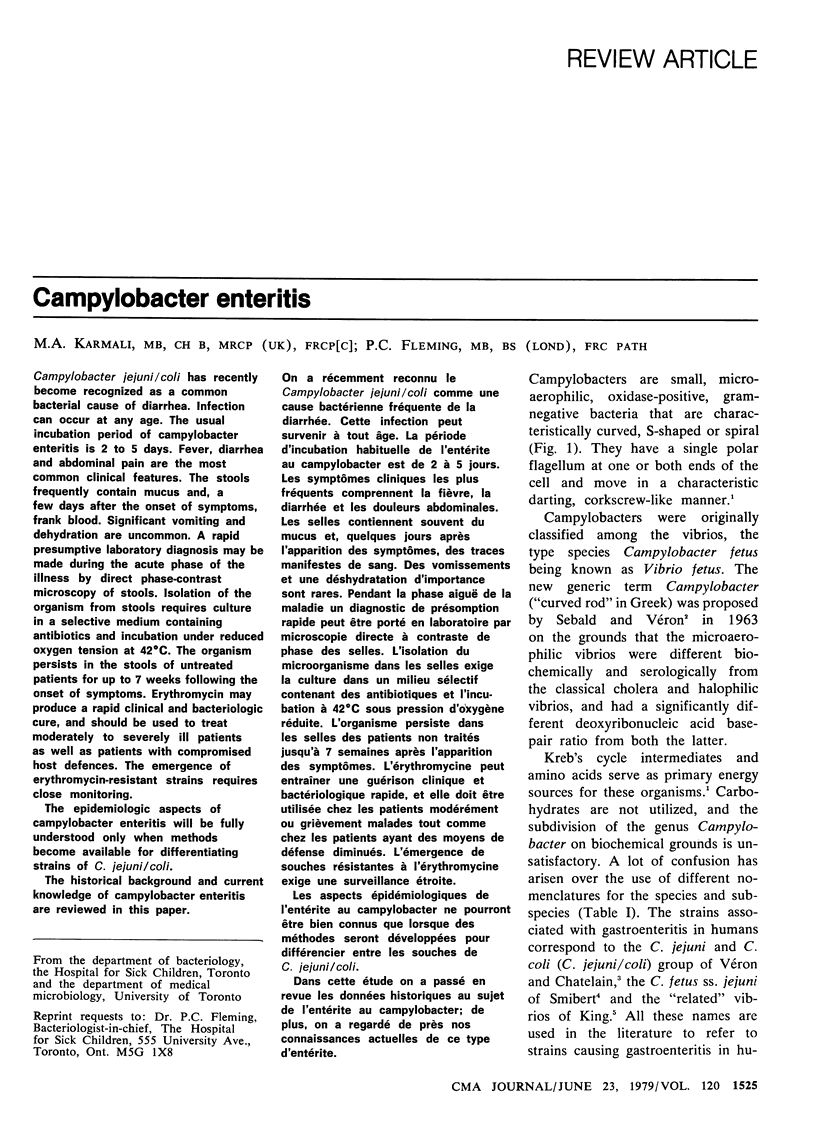


Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Berden J. H., Muytjens H. L., van de Putte L. B. Reactive arthritis associated with Campylobacter jejuni enteritis. Br Med J. 1979 Feb 10;1(6160):380–381. doi: 10.1136/bmj.1.6160.380-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blaser M., Cravens J., Powers B. W., Wang W. L. Campylobacter enteritis associated with canine infection. Lancet. 1978 Nov 4;2(8097):979–981. doi: 10.1016/s0140-6736(78)92541-2. [DOI] [PubMed] [Google Scholar]
- Bokkenheuser V. D., Richardson N. J., Bryner J. H., Roux D. J., Schutte A. B., Koornhof H. J., Freiman I., Hartman E. Detection of enteric campylobacteriosis in children. J Clin Microbiol. 1979 Feb;9(2):227–232. doi: 10.1128/jcm.9.2.227-232.1979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bokkenheuser V. Vibrio fetus infection in man. I. Ten new cases and some epidemiologic observations. Am J Epidemiol. 1970 Apr;91(4):400–409. doi: 10.1093/oxfordjournals.aje.a121150. [DOI] [PubMed] [Google Scholar]
- Bryner J. H., Ritchie A. E., Booth G. D., Foley J. W. Lytic activity of vibrio phages on strains of Vibrio fetus isolated from man and animals. Appl Microbiol. 1973 Sep;26(3):404–409. doi: 10.1128/am.26.3.404-409.1973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butzler J. P., Dekeyser P., Detrain M., Dehaen F. Related vibrio in stools. J Pediatr. 1973 Mar;82(3):493–495. doi: 10.1016/s0022-3476(73)80131-3. [DOI] [PubMed] [Google Scholar]
- Butzler J. P. Letter: Related vibrios in Africa. Lancet. 1973 Oct 13;2(7833):858–858. doi: 10.1016/s0140-6736(73)90915-x. [DOI] [PubMed] [Google Scholar]
- Cadranel S., Rodesch P., Butzler J. P., Dekeyser P. Enteritis due to "related vibrio" in children. Am J Dis Child. 1973 Aug;126(2):152–155. doi: 10.1001/archpedi.1973.02110190134004. [DOI] [PubMed] [Google Scholar]
- Campbell S. G., Cookingham C. A. The enigma of winter dysentery. Cornell Vet. 1978 Oct;68(4):423–441. [PubMed] [Google Scholar]
- Cooper I. A., Slee K. J. Human infection by Vibrio fetus. Med J Aust. 1971 Jun 12;1(24):1263–1267. doi: 10.5694/j.1326-5377.1971.tb92386.x. [DOI] [PubMed] [Google Scholar]
- Dale B. Campylobacter enteritis. Br Med J. 1977 Jul 30;2(6082):318–318. doi: 10.1136/bmj.2.6082.318-c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Darrell J. H., Farrell B. C., Mulligan R. A. Case of human vibriosis. Br Med J. 1967 Apr 29;2(5547):287–289. doi: 10.1136/bmj.2.5547.287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Mol P., Bosmans E. Campylobacter enteritis in Central Africa. Lancet. 1978 Mar 18;1(8064):604–604. doi: 10.1016/s0140-6736(78)91044-9. [DOI] [PubMed] [Google Scholar]
- Dekeyser P., Gossuin-Detrain M., Butzler J. P., Sternon J. Acute enteritis due to related vibrio: first positive stool cultures. J Infect Dis. 1972 Apr;125(4):390–392. doi: 10.1093/infdis/125.4.390. [DOI] [PubMed] [Google Scholar]
- DuPont H. L., Hornick R. B. Clinical approach to infectious diarrheas. Medicine (Baltimore) 1973 Jul;52(4):265–270. [PubMed] [Google Scholar]
- Duffell S. J., Skirrow M. B. Shepherd's scours and ovine Camphylobacter abortion--A "new" zoonosis? Vet Rec. 1978 Aug 12;103(7):144–144. doi: 10.1136/vr.103.7.144. [DOI] [PubMed] [Google Scholar]
- Fernie D. S., Park R. W. The isolation and nature of campylobacters (microaerophilic vibrios) from laboratory and wild rodents. J Med Microbiol. 1977 Aug;10(3):325–329. doi: 10.1099/00222615-10-3-325. [DOI] [PubMed] [Google Scholar]
- Guerrant R. L., Lahita R. G., Winn W. C., Jr, Roberts R. B. Campylobacteriosis in man: pathogenic mechanisms and review of 91 bloodstream infections. Am J Med. 1978 Oct;65(4):584–592. doi: 10.1016/0002-9343(78)90845-8. [DOI] [PubMed] [Google Scholar]
- Hallett A. F., Botha P. L., Logan A. Isolation of Campylobacter fetus from recent cases of human vibriosis. J Hyg (Lond) 1977 Dec;79(3):381–389. doi: 10.1017/s0022172400053225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- KING E. O. Human infections with Vibrio fetus and a closely related vibrio. J Infect Dis. 1957 Sep-Oct;101(2):119–128. doi: 10.1093/infdis/101.2.119. [DOI] [PubMed] [Google Scholar]
- Karmali M. A., Fleming P. C. Campylobacter enteritis in children. J Pediatr. 1979 Apr;94(4):527–533. doi: 10.1016/s0022-3476(79)80004-9. [DOI] [PubMed] [Google Scholar]
- Knill M., Suckling W. G., Pearson A. D. Environmental isolation of heat-tolerant Campylobacter in the Southampton area. Lancet. 1978 Nov 4;2(8097):1002–1003. doi: 10.1016/s0140-6736(78)92577-1. [DOI] [PubMed] [Google Scholar]
- Lambert M. E., Schofield P. F., Ironside A. G., Mandal B. K. Campylobacter colitis. Br Med J. 1979 Mar 31;1(6167):857–859. doi: 10.1136/bmj.1.6167.857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lauwers S., De Boeck M., Butzler J. P. Campylobacter enteritis in Brussels. Lancet. 1978 Mar 18;1(8064):604–605. doi: 10.1016/s0140-6736(78)91045-0. [DOI] [PubMed] [Google Scholar]
- MIDDELKAMP J. N., WOLF H. A. Infection due to a "related" Vibrio. J Pediatr. 1961 Sep;59:318–321. doi: 10.1016/s0022-3476(61)80283-7. [DOI] [PubMed] [Google Scholar]
- Pai C. H., Sorger S., Lackman L., Sinai R. E., Marks M. I. Campylobacter gastroenteritis in children. J Pediatr. 1979 Apr;94(4):589–591. doi: 10.1016/s0022-3476(79)80016-5. [DOI] [PubMed] [Google Scholar]
- Park C. H., McDonald F. K., Twohig A. M., Cook C. B. Septicemia and gastroenteritis due to Vibrio fetus. South Med J. 1973 May;66(5):531–533. doi: 10.1097/00007611-197305000-00004. [DOI] [PubMed] [Google Scholar]
- Peel R. N., McIntosh A. W. The dog it was that died. Lancet. 1978 Dec 2;2(8101):1212–1212. doi: 10.1016/s0140-6736(78)92209-2. [DOI] [PubMed] [Google Scholar]
- Prescott J. F., Karmali M. A. Attempts to transmit campylobacter enteritis to dogs and cats. Can Med Assoc J. 1978 Nov 4;119(9):1001–1002. [PMC free article] [PubMed] [Google Scholar]
- REICH C. V., MORSE E. V., WILSON J. B. Gaseous requirements for growth of Vibrio fetus. Am J Vet Res. 1956 Jan;17(62):140–143. [PubMed] [Google Scholar]
- Robinson D. A., Edgar W. J., Gibson G. L., Matchett A. A., Robertson L. Campylobacter enteritis associated with consumption of unpasteurised milk. Br Med J. 1979 May 5;1(6172):1171–1173. doi: 10.1136/bmj.1.6172.1171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SEBALD M., VERON M. TENEUR EN BASES DE L'ADN ET CLASSIFICATION DES VIBRIONS. Ann Inst Pasteur (Paris) 1963 Nov;105:897–910. [PubMed] [Google Scholar]
- Schewitz I. A., Roux E. Campylobacter infections. First reports from Red Cross War Memorial Children's Hospital, Cape Town. S Afr Med J. 1978 Sep 2;54(10):385–388. [PubMed] [Google Scholar]
- Severin W. P. Campylobacter en enteritis. Ned Tijdschr Geneeskd. 1978 Apr 15;122(15):499–504. [PubMed] [Google Scholar]
- Skirrow M. B. Campylobacter enteritis: a "new" disease. Br Med J. 1977 Jul 2;2(6078):9–11. doi: 10.1136/bmj.2.6078.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smibert R. M. The genus Campylobacter. Annu Rev Microbiol. 1978;32:673–709. doi: 10.1146/annurev.mi.32.100178.003325. [DOI] [PubMed] [Google Scholar]
- Smith J. P., Marymont J. H., Jr, Schweers J. Septicemia due to Campylobacter fetus in a newborn infant with gastroenteritis. Am J Med Technol. 1977 Jan;43(1):38–40. [PubMed] [Google Scholar]
- Smith M. V., 2nd, Muldoon P. J. Campylobacter fetus subspecies jejuni (Vibrio fetus) from commercially processed poultry. Appl Microbiol. 1974 May;27(5):995–996. doi: 10.1128/am.27.5.995-996.1974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steele T. W., McDermott S. Campylobacter enteritis in South Australia. Med J Aust. 1978 Oct 21;2(9):404–406. doi: 10.5694/j.1326-5377.1978.tb76814.x. [DOI] [PubMed] [Google Scholar]
- Vanhoof R., Vanderlinden M. P., Dierickx R., Lauwers S., Yourassowsky E., Butzler J. P. Susceptibility of Campylobacter fetus subsp. jejuni to twenty-nine antimicrobial agents. Antimicrob Agents Chemother. 1978 Oct;14(4):553–556. doi: 10.1128/aac.14.4.553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHEELER W. E., BORCHERS J. Vibrionic enteritis in infants. Am J Dis Child. 1961 Jan;101:60–66. doi: 10.1001/archpedi.1961.04020020062010. [DOI] [PubMed] [Google Scholar]
- Walder M., Forsgren A. Erythromycin-resistant Campylobacters. Lancet. 1978 Dec 2;2(8101):1201–1201. doi: 10.1016/s0140-6736(78)92182-7. [DOI] [PubMed] [Google Scholar]