Introduction
The management of congenital cataract is very different to the treatment of a routine age-related cataract. In adults, surgery may be delayed for years without affecting the visual outcome. In infants, if the cataract is not removed during the first year of life, the vision will never be fully regained after surgery. In adults, if the aphakia is not corrected immediately, it can be corrected later. In young children, if the aphakia is not corrected, the vision will never develop normally.
Pre-operative Evaluation
Because the whole process of managing a congenital cataract is much more complex, it is very important to make the right decisions during the pre-operative evaluation. In adults, we know that most of the poor outcomes following cataract surgery are due to poor case selection. Poor decision making at this stage can result in children being blind for the rest of their lives.
Congenital cataract affects not only the child but also their immediate family. Money spent on treatment means less is available to send other children to school. It is very important to ensure that the family understands the prognosis and duration of treatment because they are going to be responsible for implementing most of it. The families have to become our partners and colleagues in treating their own children.
Investigations
Age-related cataract usually occurs in isolation, and we rarely investigate patients to look for some underlying cause for their lens opacity. However, in children, cataract is much less common, and is more likely to be associated with some systemic condition. There are numerous different conditions that may be associated with cataract in childhood (Box 1). Most of these are rare, and in many children we do not know what causes the cataract. Even in rich countries, with almost unlimited resources, no cause is found for the majority of cataracts occurring in children.
Box 1: Causes of Congenital Cataract
Prenatal (intra-uterine) infection e.g. rubella, cytomegalovirus, syphilis.
Prenatal (intra-uterine) drug exposure e.g. corticosteroids, vitamin A.
Prenatal (intra-uterine) ionizing radiation e.g. x-rays.
Prenatal / peri-natal metabolic disorder e.g. maternal diabetes.
Hereditary (isolated - without associated eye or systemic disorder) e.g. autosomal dominant inheritance.
- Hereditary with associated systemic disorder or multi-system syndrome.
- Chromosomal e.g. Down's syndrome (trisomy 21), Turner's syndrome.
- With skeletal disease or muscle disorder e.g. Stickler syndrome, Myotonic dystrophy.
- With central nervous system disorder e.g. Norrie's disease.
- With renal disease e.g. Lowe's syndrome, Alport's syndrome.
- With mandibulo-facial disorder e.g. Nance-Horan cataract-dental syndrome.
- With dermatological disorder e.g. Congenital icthyosis, Incontinentia pigmenti.
There is no benefit in doing a large number of tests and investigations on all children with cataract. It is better to take a careful history, including a family history, from the parents. Ask about any illnesses or drugs used during the pregnancy, and find out if the child is developing normally. Remember that all blind children will experience some developmental delay, and this is usually reversed if vision is restored. However, speech and hearing development should be normal.
If possible, the child should be examined by a paediatrician, who can look for other congenital anomalies, and can determine if the child is fit for general anaesthesia. If the history and examination do not give any clues to the cause of the cataract, there is little point in doing any further investigations.
When to operate
The rules for operating on cataract are quite simple. Cataracts should only be removed when:
They are interfering with a person's quality of life
There is a reasonable prospect that surgery will lead to a significant improvement in vision.
This is true for congenital cataract as well. Unfortunately, it can be very difficult to answer these two questions in children. As a general rule, if a child is behaving and developing normally, do not operate, but keep under review. As the child grows, the visual demands will also increase. For example, a mild cataract may not interfere with playing outside the house when a child is four years old, but does cause problems at school when he or she is learning to read at the age of six or seven. Do not be misled by the red reflex, as children may see remarkably well despite a zonular cataract through which no red reflex is visible. Remember that removing a cataract in a child removes their ability to accommodate. They may be better off with 6/18 and a full range of accommodation than they would be with 6/9 and no depth of field.
Although cataract surgery in children should be done as early as possible, if there is real doubt about whether children will benefit, they are unlikely to come to serious harm by waiting a little longer. As they grow older, it becomes easier to test their vision, and to determine if they need an operation.
Surgery
Cataract surgery in children is very different to cataract surgery in adults. The operation will require a general anaesthetic. There may be associated cardiac or other congenital anomalies. The infant eye behaves very differently to an adult eye. Congenital cataract surgery should only be performed in centres that are suitably equipped to carry out these demanding procedures (Box 2).
Box 2: Minimum Facilities for Congenital Cataract Surgery
An anaesthetist with suitable equipment and skills to treat infants and small children.
A vitrectomy instrument (and/or anterior vitrectomy) to deal with the posterior capsule.
An ophthalmologist with experience in treating children.
Access to paediatric care for children with associated problems.
Access to low vision services to ensure that the child's vision develops as well as possible.
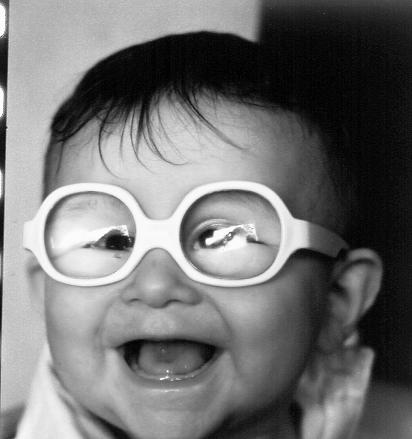
Cataract surgery in children, although complex and time-consuming, can have excellent results
Photo: David Yorston
Children do not have a hard lens nucleus, so it is possible to remove the entire cataract by aspiration alone. There are two operations that are widely used for congenital cataract.
Lensectomy
In a lensectomy, most of the lens (including the posterior capsule) and anterior vitreous is removed. This leaves a permanently clear visual axis. However, it requires a vitrectomy machine, and any interference with the vitreous may increase the risk of late retinal detachment.
My preferred technique is to use an anterior chamber maintainer inserted through the cornea. I then remove the anterior lens capsule with the vitrector, leaving an intact rim of capsule. The lens matter is aspirated, and then the posterior capsule and anterior vitreous are removed using the cutting action of the vitrector.
Provided an intact rim of capsule is retained, it is possible to insert an IOL at the time of surgery or later as a secondary procedure.
Extra-capsular Cataract Extraction (ECCE)
The anterior capsule of a child is much more elastic than an adult lens. This makes continuous curvilinear capsulorhexis (CCC) more difficult. The rhexis should be kept small (4–5mm) as the lens matter can easily be aspirated with a Simcoe cannulae, and there is no large nucleus to remove. Alternatively, a standard can-opener capsulotomy can be performed.
If the capsule is left intact, it will opacify. In adults, most patients do not develop visually significant posterior capsule opacity. However, in children, every eye will eventually need a capsulotomy. Some surgeons perform a primary capsulotomy at the end of the ECCE. However, this frequently closes and requires revision, particularly in younger children.
My own preference is to do a lensectomy on most children under five years old, and an ECCE on most older children. The rationale for this is that older children are at much less risk of amblyopia, so vision lost from capsule opacity can be regained. In younger children, capsule opacity can lead to irreversible amblyopia and must be prevented.
Intra Ocular Lenses (IOLs)
In infants it is essential to correct aphakia as soon as possible after surgery. One option is to implant an IOL when the cataract is removed. Unfortunately, it is not that simple. At birth the human lens is more spherical than in adults. It has a power of about 30D, which compensates for the shorter axial length of a baby's eye. This decreases to about 20–22D by the age of five. This means that an IOL which gives normal vision to an infant will lead to significant myopia when he or she is older. It is further complicated by changes in the power of the cornea and axial lengthening of the globe. These changes are most rapid during the first few years of life and this makes it almost impossible to predict the correct power of lens for any infant.
IOL implantation has become quite routine for older children, but it is still very controversial in younger children, particularly those under two years old (see Community Eye Health Vol. 14 No. 40, 2001).
Post-operative Care
In adults, little post-operative care is required, apart from the provision of eye drops and spectacles – if required. In children, the surgery is only the beginning of a prolonged course of treatment and this needs to be emphasised from the beginning.
Refraction
The first priority is to correct the aphakia and this should be done as early as possible. In rich countries contact lenses are widely used. They can be changed easily and the power can be modified. However, they require meticulous hygiene and this makes them inappropriate in situations with inadequate water and sanitation. Alternatives are to use spectacles or an IOL. Even if an IOL is used there will be some residual refractive error and spectacles will be necessary to get the best possible vision. The spectacles should be fitted as soon as the child is able to wear them. The refraction must be checked regularly, at least every four months until two years old, reducing to an annual check after the age of five.
Amblyopia
Most children with congenital cataract will be amblyopic. Because the retinal image has been blurred by the cataract, vision does not develop properly, and the brain cannot make sense of the information it receives from the eye. Removing the cataract, and correcting the aphakia, will restore image clarity but the brain still needs to learn to see, and this takes time. If the eyes have never had clear vision, they will not fixate accurately and this can lead to nystagmus. If the vision is restored, the nystagmus will often resolve, so nystagmus in a child is not a contra-indication to surgery.
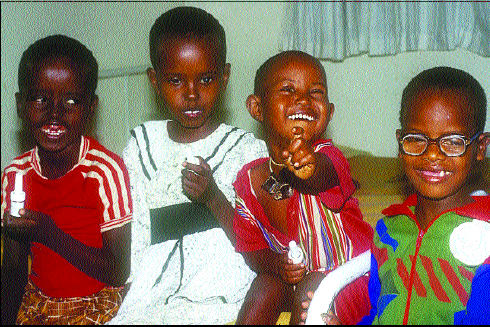
The spectacles should be fitted as soon as the child is able to wear them
Photo: Clare Gilbert
Frequently one eye will do better than the other and this will become the preferred eye, which makes the other eye amblyopic. The only way to detect this is to measure the best corrected vision regularly in each eye. If one eye is two or more lines worse than the other, with no other apparent explanation, it is probably amblyopic and the child needs occlusion treatment of the preferred eye. The risk of amblyopia is greatest during the first year of life and declines rapidly after the age of five.
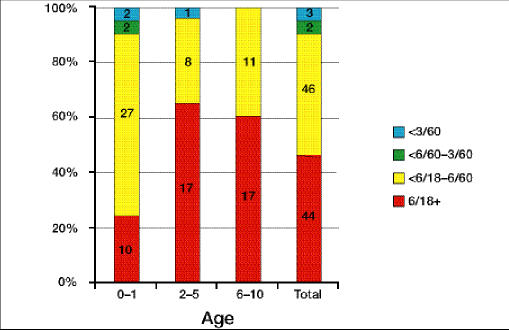
Providing optimum care is provided, the visual prognosis is good. In Kenya, 47% of eyes achieved 6/18 or better and only 5% were less than 6/60.1 Almost all these children will be able to attend a normal school (Fig. 1).
Fig. 1.
Results of Cataract Surgery in Young Children in East Africa
Complications
Every child who does not have a posterior capsulotomy will develop posterior capsule opacification. This can be treated by making an opening in the capsule with a Nd:YAG laser or a needle. Alternatively, the posterior capsule and anterior vitreous can be removed with a vitrector. If the capsule is opened without removing the vitreous, the opacification may recur on the anterior hyaloid face. Loss of vision in one eye from increasing capsule opacity will be asymptomatic and the only way to detect this is by regular examinations.
Glaucoma may occur after lensectomy, particularly if it is carried out in the first week of life. This glaucoma is very difficult to treat and frequently leads to blindness. Delaying surgery until after the child is 3–4 months old makes it unlikely that the eyes will recover 6/6 vision but it reduces the risk of glaucoma.
Retinal detachment is more common in eyes that have had surgery for congenital cataract. It often occurs very late, on average 35 years after the operation. If any patient complains of sudden loss of vision, even if it is years after their operation for congenital cataract, it should be assumed to be due to retinal detachment until proven otherwise.
Conclusion
The management of congenital cataract is complex, and should only be carried out in specialist centres. However, every eye worker can play a role by assisting with case finding and follow-up.
Reference
- Yorston D, Wood M, Foster A. Results of cataract surgery in young children in East Africa. Br J Ophthalmol. 2001;85(3):267–271. doi: 10.1136/bjo.85.3.267. [DOI] [PMC free article] [PubMed] [Google Scholar]