Abstract
The incretin hormones glucagon-like peptide–1 (GLP-1) and glucose-dependent insulinotropic polypeptide (GIP) control glucose homeostasis through well-defined actions on the islet β cell via stimulation of insulin secretion and preservation and expansion of β cell mass. We examined the importance of endogenous incretin receptors for control of glucose homeostasis through analysis of Glp1r–/–, Gipr–/–, and double incretin receptor knockout (DIRKO) mice fed a high-fat (HF) diet. DIRKO mice failed to upregulate levels of plasma insulin, pancreatic insulin mRNA transcripts, and insulin content following several months of HF feeding. Both single incretin receptor knockout and DIRKO mice exhibited resistance to diet-induced obesity, preservation of insulin sensitivity, and increased energy expenditure associated with increased locomotor activity. Moreover, plasma levels of plasminogen activator inhibitor–1 and resistin failed to increase significantly in DIRKO mice after HF feeding, and the GIP receptor agonist [D-Ala2]GIP, but not the GLP-1 receptor agonist exendin-4, increased the levels of plasma resistin in studies of both acute and chronic administration. These findings extend our understanding of how endogenous incretin circuits regulate glucose homeostasis independent of the β cell via control of adipokine secretion and energy expenditure.
Introduction
Gut hormones secreted in response to nutrient ingestion play essential roles at multiple levels in the regulation of energy homeostasis (1). Enteroendocrine-derived peptides modulate gastrointestinal motility and communicate signals regulating satiety to central nervous system centers, initiating and terminating food ingestion. Moreover, gut peptides, exemplified by glucagon-like peptide–2, regulate nutrient absorption and mucosal epithelial integrity, thereby optimizing nutrient absorption. At least 2 gastrointestinal peptides, glucagon-like peptide–1 (GLP-1) and glucose-dependent insulinotropic polypeptide (GIP), function as incretin hormones, potentiating insulin secretion in response to enteral nutrient signals (2, 3).
GLP-1 and GIP exhibit overlapping actions on the islet β cell via interaction with structurally related yet distinct G protein–coupled receptors (4). Activation of either the GLP-1 receptor (GLP-1R) or the GIP receptor (GIPR) engages β cell signaling pathways coupled to stimulation of insulin secretion in a glucose-dependent manner. Both incretins also stimulate pathways regulating β cell proliferation and inhibition of β cell apoptosis (5, 6). Although GLP-1 actions on insulin secretion remain intact in the setting of experimental or clinical diabetes, the insulinotropic action of GIP is impaired in the context of diabetes, but the defect(s) leading to loss of GIP action on the diabetic β cell remain poorly understood (7).
GLP-1 and GIP also have effects independent of insulin secretion. GLP-1 inhibits glucagon secretion and gastric emptying, leading to reduction of blood glucose even in subjects with type 1 diabetes (8, 9). Furthermore, GLP-1R agonists act as satiety factors (10), reducing food intake and inducing weight loss following chronic administration in both preclinical and clinical studies (11, 12). In contrast, GIP acts as an anabolic factor for bone (13) and stimulates insulin-dependent glucose uptake and lipoprotein lipase activity in adipose tissue (14, 15).
The majority of incretin actions have been delineated in pharmacologic studies employing exogenous administration of GLP-1 and GIP, often resulting in supraphysiologic levels of circulating incretin hormones. Conversely, the importance of endogenous incretin action for glucose homeostasis has been studied using peptide antagonists, immunoneutralizing antibodies, and targeted disruption of incretin receptor gene expression (16–18). Surprisingly, despite the potent glucose-lowering actions of exogenous incretin receptor agonists, disruption of incretin action produces only modest perturbations in glucose homeostasis (16–20).
One potential explanation for the mild glucose intolerance observed in single incretin receptor knockout mice (17, 18) invokes upregulation of compensatory factors, particularly enhanced activity of the remaining incretin. Support for this hypothesis is derived from observations that Glp1r–/– mice exhibit increased circulating levels of GIP and selectively enhanced sensitivity to the insulinotropic actions of GIP both in vitro and in vivo (21). Moreover, results of complementary studies in Gipr–/– mice reveal normal circulating levels of GLP-1 but enhanced sensitivity to GLP-1 action (22).
To delineate the physiologic importance of incretin action, we generated double incretin receptor knockout (DIRKO) mice. Surprisingly, DIRKO mice exhibit only modest perturbations in glucose homeostasis and retain normal insulin sensitivity despite complete disruption of both incretin receptors (23, 24). We hypothesized that the physiologic importance of combined GLP-1 and GIPR action for glucose homeostasis would be unmasked in the presence of a metabolic stress such as chronic high-fat feeding (HFF). We found that DIRKO mice exhibited multiple defects in the adaptive β cell response to HFF together with abnormal regulation of plasma adipokines. Unexpectedly, disruption of incretin receptor action in single incretin receptor knockout mice and in DIRKO mice was also associated with enhanced locomotor activity, increased energy expenditure, and resistance to diet-induced obesity. These results delineate what we believe to be new aspects of endogenous incretin receptor action that are critically important for control of glucose homeostasis and body weight.
Results
DIRKO mice are resistant to high-fat diet–induced obesity.
To examine the physiologic role(s) of incretin action for the control of glucose homeostasis, male WT, Glp1r–/–, Gipr–/–, and DIRKO mice were placed on regular chow (RC) or a high-fat (HF) diet for 20 weeks beginning at 9 weeks of age. Although WT mice fed HF diet displayed accelerated weight gain compared with RC-fed WT mice (Figure 1A), DIRKO mice failed to exhibit significant weight gain on HF diet. In contrast, Glp1r–/– and Gipr–/– mice gained small but significant amounts of weight on HF diet (Supplemental Figure 1, B and C; supplemental material available online with this article; doi:10.1172/JCI25483DS1). Furthermore, DIRKO mice on RC weighed significantly less than did their WT counterparts (Figure 1A).
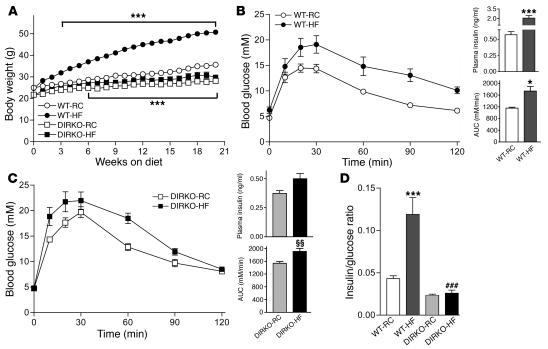
Figure 1. DIRKO mice exhibit reduced weight gain and impaired glucose tolerance on HF diet.
(A) Body weight gain in WT and DIRKO mice on RC or HF diet (n = 8–13 per group). (B and C) Oral glucose tolerance in WT (B) and DIRKO mice (C) fed RC or HF diet for 12 weeks (n = 6–8 per group). At right, plasma insulin concentrations obtained 10 minutes after glucose administration (top; n = 6–8 per group) and quantification of AUC for the total glycemic excursions (bottom; n = 6–8 per group). (D) Plasma insulin/glucose ratios (ng/ml to mmol/l) at the 10–20 minute time point following glucose administration (n = 6–8 per group). *P < 0.05, ***P < 0.001 versus WT-RC; ###P < 0.001 versus WT-HF; ΧΧP < 0.01 versus DIRKO-RC.
Defective β cell function in HF diet–fed DIRKO mice.
To determine whether HFF impairs β cell function in DIRKO mice despite the absence of obesity, we assessed oral glucose tolerance after 12 weeks of HFF. Although WT mice gained significantly more weight relative to DIRKO mice on the HF diet, the deterioration in glucose tolerance was comparable between WT and DIRKO mice after 12 weeks of HFF (Figure 1, B and C). Plasma levels of glucose-stimulated insulin increased more than 3-fold in WT mice after HFF (RC, 0.58 ± 0.05 ng/ml; HF diet, 2.07 ± 0.38 ng/ml; n = 7–8 per group; P < 0.001; Figure 1B). In contrast, despite a greater increase in area under the curve (AUC) glucose following glucose loading in DIRKO mice, plasma insulin levels were lower in RC-fed DIRKO mice compared with those of RC-fed WT mice (Figure 1, B and C) and failed to increase significantly after oral glucose challenge (RC, 0.37 ± 0.02 ng/ml; HF diet, 0.49 ± 0.04 ng/ml; n = 8) despite a significant increase in AUC glucose after HFF (Figure 1C). Consistent with these findings, the insulin/glucose ratio increased significantly in WT mice but not in DIRKO mice after 12 weeks of HFF (Figure 1D). Hence, DIRKO mice exhibit deterioration of glucose tolerance and an inability to upregulate plasma levels of insulin following HFF. Although both Glp1r–/– and Gipr–/– mice exhibited deterioration in glucose tolerance following HFF, the impairment in glucose tolerance was more pronounced in Glp1r–/– mice, which showed a higher AUC glucose despite greater augmentation of glucose-stimulated insulin secretion compared with Gipr–/– mice (Supplemental Figure 1, E and F).
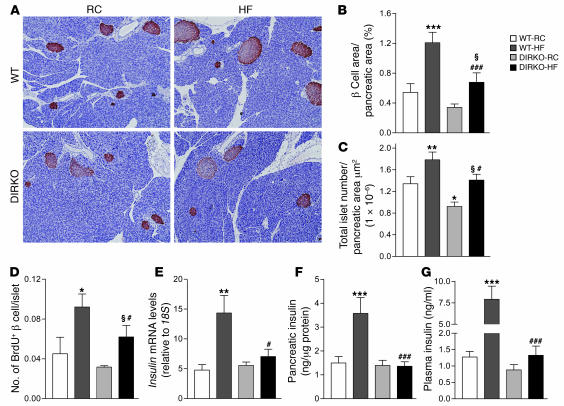
As GLP-1 and GIP regulate β cell growth and survival, we examined whether the β cell response to HFF was compromised in DIRKO mice. WT mice exhibited larger and more numerous islets following 20 weeks of HFF (Figure 2, A and B), with significant increases in β cell area and islet number observed relative to RC-fed WT mice (approximately 2.2- and 1.3-fold, respectively; Figure 2, B and C). Although β cell area and islet number increased significantly in WT and DIRKO mice after HFF (Figure 2, B and C), HF diet–fed DIRKO mice exhibited significantly lower β cell area and fewer islets compared with their HF diet–fed WT counterparts (Figure 2C). Moreover, β cell proliferation as assessed by the number of BrdU+ β cells was significantly lower in DIRKO relative to WT mice after 20 weeks of HFF (Figure 2D).
Figure 2. Analyses of the endocrine pancreas in WT and DIRKO mice.
Following 20 weeks on RC or HF diet, nonfasted WT and DIRKO mice were euthanized, and pancreata were harvested for assessment of insulin mRNA and insulin content as well as for histological and morphometric analyses. Blood was also obtained by cardiac puncture for measurement of ambient levels of circulating insulin. (A) Pancreatic histology and immunohistochemical staining for insulin in sections from WT and DIRKO mice. Original magnification, ×100. (B) Percent total β cell area per total pancreatic area (n = 5–9 per group). (C) Total islet number per total pancreatic area in μm2 (n = 6–9 per group). (D) Number of BrdU+ β cells per islet (n = 4–7 per group). (E) Insulin mRNA levels in pancreata from mice (n = 7–8 per group). (F) Pancreatic insulin content in WT and DIRKO mice (n = 7–10 per group). (G) Ambient levels of plasma insulin (n = 8–12 per group). *P < 0.05, **P < 0.01, ***P < 0.001 versus WT-RC; #P < 0.05, ###P < 0.001 versus WT-HF; ΧP < 0.05 versus DIRKO-RC.
Exogenous administration of GLP-1 and GIP has been shown to increase insulin biosynthesis via induction of insulin gene expression (25, 26); however, basal pancreatic insulin content is normal in DIRKO mice on RC (23, 24). Following 20 weeks of HFF, levels of pancreatic insulin mRNA (Figure 2E) and insulin content (Figure 2F) were markedly increased in WT mice compared with those of RC-fed WT mice. In contrast, both single incretin receptor knockout mice (Supplemental Figure 2B) and DIRKO mice (Figure 2F) failed to exhibit significant increases in pancreatic insulin levels after HFF. Furthermore, although circulating levels of plasma insulin increased greater than 5-fold in HF diet–fed WT mice, plasma insulin levels were not significantly increased in DIRKO mice (Figure 2G) or in single incretin receptor knockout mice (Supplemental Figure 2C) following 20 weeks of HFF. Taken together, these findings demonstrate multiple defects in the β cell response to metabolic stress induced by HFF in both single incretin receptor knockout and DIRKO mice.
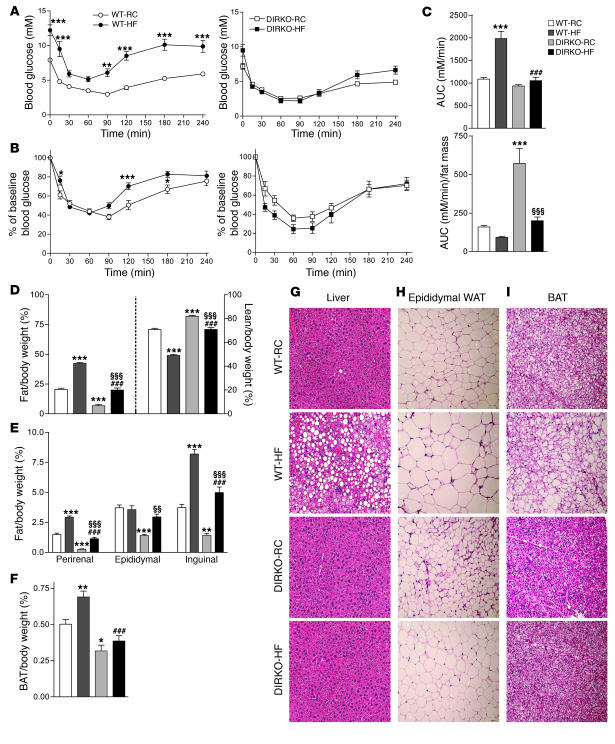
The comparatively modest deterioration in glucose tolerance in DIRKO mice despite the failure to augment insulin biosynthesis or increase plasma levels of insulin after prolonged exposure to increased dietary fat prompted us to examine insulin sensitivity via insulin tolerance testing. Gipr–/– mice exhibit resistance to obesity and preserved insulin sensitivity following prolonged HFF (15), whereas DIRKO mice were previously shown to exhibit normal insulin sensitivity on a regular diet (23, 24). We hypothesized that HF diet–fed DIRKO mice evolved a compensatory preservation of insulin sensitivity. As expected, WT mice exhibited a significantly blunted hypoglycemic response to insulin following 19 weeks of HFF (Figure 3, A and B). In contrast, the hypoglycemic response to insulin was not significantly different in single incretin receptor knockout mice (Supplemental Figure 3B) or DIRKO mice after 19 weeks of HFF compared with their respective RC-fed controls (Figure 3, A and B), which suggests relative preservation of insulin sensitivity following HFF. Furthermore, the AUC glucose following insulin administration was similar in HF diet–fed WT and DIRKO mice after correction for fat mass (Figure 3C).
Figure 3. DIRKO mice are protected from HF diet–induced insulin resistance.
(A) Glucose levels during an insulin tolerance test in RC- and HF diet–fed WT and DIRKO mice (n = 8–9 per group). After 19 weeks of HFF, WT and DIRKO mice were fasted for 5 hours and subsequently injected with 1.2 U/kg insulin. Blood glucose levels were monitored for 4 hours following insulin administration. (B) Glucose levels during an insulin tolerance test expressed as percentage of baseline blood glucose values in WT and DIRKO mice. (C) Quantification of AUC for the total glycemic excursions in A and AUC normalized to fat mass. (D) Weights of total body fat and lean mass normalized to body weight (n = 8–9 per group) in WT and DIRKO mice fed RC or HF diet for 19 weeks as assessed by MRI. (E) Weights of perirenal, epididymal, and inguinal fat pads normalized to body weight (n = 8–12 per group). (F) Weight of brown adipose tissue (BAT) normalized to body weight (n = 8–12 per group). (G–I) Histological analyses of (G) liver, (H) epididymal white adipose tissue (WAT), and (I) brown adipose tissue from WT and DIRKO mice fed RC or HF diet. Sections were stained with H&E. Original magnification, ×200. *P < 0.05, **P < 0.01, ***P < 0.001 versus WT-RC; ###P < 0.001 versus WT-HF; ΧΧP < 0.01, ΧΧΧP < 0.001 versus DIRKO-RC.
One potential explanation for preservation of insulin sensitivity may be resistance to weight gain and decreased fat mass in DIRKO mice despite prolonged HFF. WT mice exhibited increased total fat mass following HFF when normalized for body weight, whereas DIRKO mice had significantly less body fat and a greater proportion of lean mass despite HFF (Figure 3D). Furthermore, DIRKO mice exhibited decreased fat pad weight after RC feeding (Figure 3E). Nevertheless, fat pad weight increased significantly in each depot after HFF in Glp1r–/– and Gipr–/– mice (Supplemental Figure 3C) as well as DIRKO mice (Figure 3E). In contrast, brown adipose tissue weight increased significantly in WT but not in DIRKO mice after HFF (Figure 3F). Hepatocytes from WT mice exhibited markedly increased lipid accumulation following HFF; however, single incretin receptor knockout mice (Supplemental Figure 3E) and DIRKO mice (Figure 3G) exhibited no clear increase in hepatic lipid accumulation after 20 weeks of HFF. Although DIRKO adipocytes appeared smaller relative to WT adipocytes on RC, DIRKO, Glp1r–/–, and Gipr–/– epididymal adipocytes increased in size after 20 weeks of HFF (Figure 3H and Supplemental Figure 3F). In contrast, brown adipocytes from DIRKO mice failed to accumulate significant amounts of lipid following HFF (Figure 3I).
DIRKO mice exhibit increased energy expenditure.
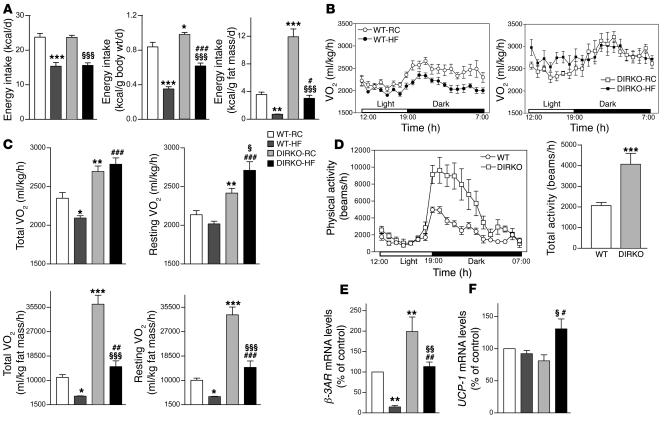
Analysis of basal energy intake in WT and DIRKO mice 1 week prior to the start of HFF did not reveal any significant differences in energy intake, neither in absolute terms nor when normalized to body weight (Supplemental Figure 4A). However, DIRKO mice exhibited significantly higher rates of oxygen consumption compared with WT controls throughout the light and dark cycles, indicative of increased energy expenditure (Supplemental Figure 4B). Although no significant differences were observed in the absolute amount of total kcal consumed over 24 hours between WT and DIRKO mice fed HF diet, both RC- and HF diet–fed DIRKO mice were significantly more hyperphagic when food consumption was corrected for body weight or fat mass (Figure 4A), despite gaining less weight on both diets (Figure 1A). Consistent with the possibility that GLP-1 functions as an endogenous satiety factor (10), Glp1r–/– mice exhibited increased energy intake on both RC and HF diet compared with WT and Gipr–/– mice (Supplemental Figure 5A). Both single incretin receptor knockout mice (Supplemental Figure 5, B and C) and DIRKO mice (Figure 4, B and C) demonstrated oxygen consumption rates significantly higher than those of their WT counterparts throughout the light and dark cycles on both RC and HF diet. Furthermore, whereas HF diet–fed WT mice exhibited significantly lowered oxygen consumption compared with their RC-fed counterparts, single incretin receptor knockout mice and DIRKO mice failed to exhibit reduced oxygen consumption on HF diet (Figure 4, B and C, and Supplemental Figure 5, B and C), and energy expenditure remained significantly increased in HF diet–fed DIRKO mice compared with their RC- or HF diet–fed WT counterparts when normalized for body fat content (Figure 4C). As icv GLP-1 may induce malaise associated with reduced locomotor activity, we assessed locomotor activity in RC-fed WT mice, single incretin receptor knockout mice, and DIRKO mice. Remarkably, DIRKO mice exhibited significantly increased locomotor activity relative to WT mice (Figure 4D). Furthermore, significant increases in locomotor activity were also observed in both Glp1r–/– and Gipr–/– mice (Supplemental Figure 5D).
Figure 4. Increased energy expenditure in DIRKO mice.
(A) Following an overnight fast (16–18 hours), WT and DIRKO mice were placed in individual cages, and food intake was monitored over 24 hours (n = 7–8 per group). Data are expressed as kcal consumed per day, kcal consumed per gram of body weight per day, and kcal consumed per gram of fat mass per day. (B) Oxygen consumption (VO2) was measured during the light and dark cycles in WT and DIRKO mice (n = 8 per group). (C) Total oxygen consumption over the light and dark phases, resting oxygen consumption (oxygen consumption over the light phase), and total and resting oxygen consumption normalized to fat mass. (D) Assessment of physical activity (as described in Methods) during the light and dark cycles in WT and DIRKO mice (n = 4–6 per group). At right, data are expressed as total physical activity over the light and dark cycles. (E) Expression of β3AR mRNA levels in epididymal white adipose tissue (n = 5–7 per group) relative to 18S. (F) Expression of UCP-1 in brown adipose tissue (n = 5–6 per group) relative to 18S. *P < 0.05, **P < 0.01, ***P < 0.001 versus WT-RC; #P < 0.05, ##P < 0.01, ###P < 0.001 versus WT-HF; ΧP < 0.05, ΧΧP < 0.01, ΧΧΧP < 0.001 versus DIRKO-RC.
As the β3 adrenergic receptor (β3AR) plays an important role in the regulation of energy balance (27), we examined β3AR expression in white adipose tissue. HF diet–fed WT mice demonstrated markedly reduced β3AR mRNA transcripts (Figure 4E). In contrast, the levels of β3AR mRNA transcripts were significantly increased in RC-fed Glp1r–/–, Gipr–/–, and DIRKO mice compared with RC-fed WT mice and were only partially suppressed following HFF (Figure 4E and Supplemental Figure 5E). Furthermore, mRNA levels of uncoupling protein–1 (UCP-1) in brown adipose tissue from HF diet–fed Gipr–/– and DIRKO mice were significantly increased compared with HF diet–fed WT mice (Figure 4F and Supplemental Figure 5F). Taken together, these findings suggest that multiple mechanisms contribute to increased energy expenditure and the prevention of HF diet–induced obesity in DIRKO mice.
Circulating adipokines in DIRKO mice.
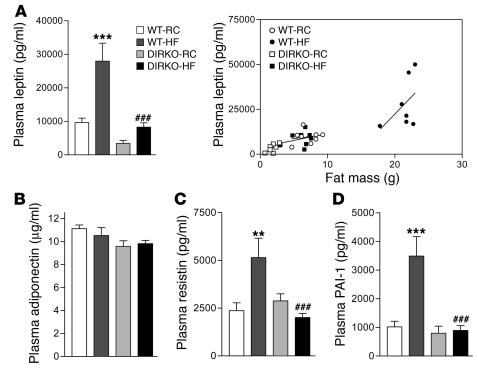
GIP, but not GLP-1, has been postulated to exert direct metabolic actions in fat tissue (14); however, whether enhancement or loss of incretin receptor signaling modifies adipokine secretion has not to our knowledge been examined previously. Plasma levels of TNF-α were undetectable in all mice (data not shown). Although levels of plasma leptin increased in both WT and DIRKO mice after HFF, leptin levels in HF diet–fed DIRKO mice remained approximately 3-fold lower than those in HF diet–fed WT mice (Figure 5A). Similarly, leptin levels increased in single incretin receptor knockout mice following HFF but remained significantly lower than those of HF diet–fed WT mice (Supplemental Figure 6A). Surprisingly, while no significant changes in circulating adiponectin were detected in WT, Glp1r–/–, or DIRKO mice after HFF (Figure 5B and Supplemental Figure 6B), adiponectin levels were significantly increased in Gipr–/– mice (Supplemental Figure 6B). Furthermore, DIRKO mice failed to exhibit increased circulating levels of either resistin or plasminogen activator inhibitor–1 (PAI-1) following HFF (Figure 5, C and D), whereas the levels of resistin and PAI-1 increased significantly following HFF in Gipr–/– and Glp1r–/– mice, respectively (Supplemental Figure 6, C and D).
Figure 5. Ambient circulating levels of plasma adipokines in mice fed RC or HF diet for 20 weeks.
Following 20 weeks on RC or HF diet, WT and DIRKO mice were euthanized and cardiac blood was obtained. (A) Ambient levels of circulating leptin in WT and DIRKO mice (n = 7–11 per group). At right, data are expressed as a scatter plot with leptin levels on the y axis and fat mass on the x axis, demonstrating that the leptin levels were at the level expected for the degree of adiposity. (B–D) Ambient levels of circulating (B) adiponectin (n = 8–12 per group), (C) resistin (n = 8–12 per group), and (D) PAI-1 (n = 7–12 per group) in WT and DIRKO mice following 20 weeks of RC or HF diet. **P < 0.01, ***P < 0.001 versus WT-RC; ###P < 0.001 versus WT-HF.
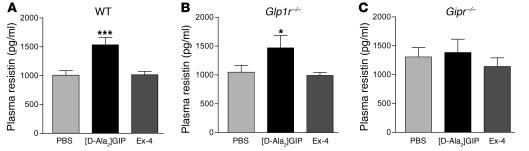
Activation of GIPR, but not GLP-1R, increases plasma resistin in WT and Glp1r–/– mice.
The findings of reduced levels of plasma leptin as well as defective upregulation of PAI-1 and resistin in HF diet–fed DIRKO mice relative to WT mice prompted us to ascertain whether these differences arose as a result of abnormalities inherent in DIRKO adipocytes or whether they reflected a previously unrecognized role for GLP-1R and/or GIPR in the regulation of plasma adipokines. The GLP-1R agonist exendin-4 (Ex-4) had no significant effect on circulating levels of leptin or PAI-1 (data not shown) or resistin in WT mice (Figure 6A), Glp1r–/– mice (Figure 6B), or Gipr–/– mice (Figure 6C). In contrast, although acute [D-Ala2]GIP administration had no significant effect on levels of leptin or PAI-1 (data not shown), circulating levels of resistin were significantly increased after [D-Ala2]GIP administration in WT and Glp1r–/– mice, but not in Gipr–/– mice (Figure 6, A–C).
Figure 6. Resistin secretion stimulated by [D-Ala2]GIP in WT and Gipr–/– mice.
(A–C) Effect of 24 nmol/kg [D-Ala2]GIP or Ex-4 on resistin secretion in 10-week-old (A) WT, (B) Glp1r–/–, and (C) Gipr–/– mice following an oral glucose load (n = 5–15 per group). Mice were fasted overnight, after which PBS or peptide was administered immediately prior to oral glucose loading. Mice were euthanized at 45 minutes following peptide/glucose administration, and cardiac blood was obtained. *P < 0.05, ***P < 0.001 versus PBS and Ex-4.
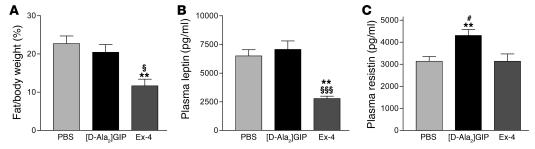
Chronic administration of [D-Ala2]GIP increases plasma resistin in HF diet–fed WT mice.
To determine whether chronic exposure to incretin receptor agonists modulates adipokine levels in WT mice, we administered 24 nmol/kg of [D-Ala2]GIP or Ex-4 twice daily for 2 weeks to HF diet–fed mice. Treatment with Ex-4 resulted in a significant decrease in adiposity and a concomitant reduction in plasma leptin but no change in resistin levels (Figure 7, A–C). In contrast, treatment with [D-Ala2]GIP significantly increased levels of plasma resistin (Figure 7C) independent of changes in fat mass or plasma leptin (Figure 7, A–C).
Figure 7. Chronic exposure of WT mice to incretin receptor agonists.
WT mice were maintained on HF diet starting from 6 weeks of age. After 4 weeks of HFF, mice were administered either PBS or 24 nmol/kg [D-Ala2]GIP or Ex-4 twice daily for 2 weeks, after which body fat composition was assessed by MRI. Mice were euthanized 1 hour after the last injection of PBS or peptide, and cardiac blood was collected. (A) Total body fat mass normalized to body weight (n = 8–19 per group). (B and C) Ambient levels of (B) plasma leptin and (C) plasma resistin in HF diet–fed WT mice treated twice daily with either [D-Ala2]GIP or Ex-4 (n = 8–19 per group). **P < 0.01 versus PBS; ΧP < 0.05, ΧΧΧP < 0.001 versus [D-Ala2]GIP; #P < 0.05 versus Ex-4.
Discussion
The enteroinsular axis, a term defined by Unger and Eisentraut (28), describes the phenomena of greater insulin release when nutrients are taken orally versus intravenously, even under conditions of an isoglycemic load. GIP and GLP-1 are believed to represent the predominant incretins, and disruption of each incretin receptor gene in mice produces glucose intolerance together with defects in glucose-stimulated insulin secretion (17, 18). Furthermore, exogenous administration of GIP or GLP-1 potentiates glucose-dependent insulin secretion (29). Hence the results of both gain- and loss-of-function studies support the physiologic and pharmacologic importance of incretin action for control of meal-stimulated insulin secretion.
More recent studies have identified actions for GLP-1 and GIP independent of insulin secretion, including regulation of β cell proliferation (5, 30) and activation of insulin gene transcription with subsequent induction of insulin biosynthesis. Surprisingly, despite complete disruption of the genes encoding GIPR and GLP-1R, insulin mRNA transcripts, pancreatic insulin content, and β cell area were normal in DIRKO mice on a regular diet (23, 24). We hypothesized that the importance of incretin action for β cell function might be determined following exposure of mice to prolonged HFF and its resulting sustained glucolipotoxic stress. Our data illustrate that DIRKO mice were unable to increase levels of insulin mRNA or pancreatic insulin content despite the presence of chronic hyperglycemia. These findings demonstrate that incretin receptors are essential for β cell adaptation to metabolic stress caused by chronic HFF.
Gipr–/– mice exhibit normal growth and body weight on RC, but chronic HFF is associated with increased energy expenditure during the light phase of the feeding cycle (15, 18). Our present data demonstrate that Glp1r–/– and DIRKO mice also exhibited increased energy expenditure on RC as well as HF diet during both light and dark phases of the feeding cycle. Furthermore, DIRKO mice exhibited resistance to diet-induced obesity to a greater extent than that previously described for single incretin receptor knockout mice (15, 18, 31). Remarkably, although DIRKO mice also exhibited increased food intake, the dominant effect of increased energy expenditure resulted in failure to gain weight with increasing age on both RC and HF diet. Furthermore, the increased energy expenditure in both single incretin receptor knockout and DIRKO mice is likely attributable in part to enhanced locomotor activity. These observations suggest that the importance of GLP-1 action as a negative regulator of energy intake is balanced by what we believe to be a previously unrecognized role for endogenous GLP-1 in the control of motor activity, resulting in resistance to diet-induced obesity despite increased energy intake in Glp1r–/– and DIRKO mice.
Introduction of the null Gipr allele into the ob/ob genetic background produces substantial attenuation of the obese phenotype, with Gipr–/–:ob/ob mice exhibiting reduced weight gain and decreased fat mass relative to the phenotype exhibited by the parental ob/ob mice. These findings were attributable to the loss of anabolic GIP action on the adipocyte, which results in increased fat oxidation, reduced lipid accumulation, and enhanced energy expenditure (15). Similarly, DIRKO mice exhibited reduced fat mass, increased adipose tissue expression of mRNA transcripts for β3AR, and uniformly decreased size of white adipose tissue depots and adipocytes, together with reduced fat accumulation in peripheral tissues such as the liver, despite HFF. Hence loss of GIPR signaling likely protects DIRKO mice from many of the metabolic derangements caused by chronic exposure to nutrient excess.
Our present data demonstrate that GIP also regulated levels of plasma adipokines, likely through control of adipokine secretion. Although plasma levels of leptin, resistin, and PAI-1 increased markedly following HFF in control mice, DIRKO mice failed to upregulate levels of resistin or PAI-1 despite several months of HFF. Furthermore, acute and chronic administration of the GIPR agonist [D-Ala2]GIP, but not the GLP-1R agonist Ex-4, increased plasma levels of resistin in WT mice. These observations define what we believe to be a new role for GIPR signaling as an essential component of the adipocyte response to chronic nutritional excess.
Both single incretin receptor knockout mice and DIRKO mice exhibited reduced adiposity on RC and following HFF. As adipose tissue mass is a key determinant of insulin sensitivity, reduced adiposity likely contributes to preservation of insulin sensitivity in single incretin receptor knockout and DIRKO mice. Our present observations linking GIP action to modulation of plasma adipokines and control of energy expenditure clarify divergent roles of GIP action on the β cell, adipocyte, and brain. Whereas loss of GIP action on the β cell impaired the adaptive islet response to metabolic stress, the potential deleterious effect arising from loss of incretin action and impaired insulin secretion was offset by preservation of insulin sensitivity, likely arising through a combination of reduced plasma adipokines, decreased adipose tissue mass, and increased energy expenditure. Similarly, although loss of endogenous anorectic GLP-1 action might lead to increased energy intake and obesity, an increase in locomotor activity and energy expenditure preserved a lean phenotype in Glp1r–/– mice. Taken together, these observations further expand our concepts of incretin receptor actions beyond the β cell and illustrate essential roles for incretin receptors in the modulation of glucose homeostasis via effects on the adipocyte and central nervous system.
Methods
Animal studies.
The generation of Gipr–/–, Glp1r–/–, and DIRKO mice has been described previously (24). Male WT mice (C57BL/6; Charles River Laboratories), single incretin receptor knockout mice, littermate controls, and DIRKO mice were housed 4 per cage under a light/dark cycle of 12 hours in the Toronto General Hospital animal facility, with free access to food and water except where noted. All WT mice used for these studies were acclimatized to the animal facility for several weeks prior to analysis. Nine-week-old mice were fed ad libitum RC or HF diet (Research Diets Inc.), with 10% or 45% kcal from fat, respectively. Individual body weights were monitored over a 20-week period. For assessment of fat and lean mass, a mouse whole-body magnetic resonance analyzer was used (Echo Medical Systems). All procedures were conducted according to protocols and guidelines approved by the Toronto General Hospital Animal Care Committee. For confirmation of genotypes, genomic DNA prepared from tail snips was analyzed by Southern blotting (18, 32).
Glucose tolerance tests and measurement of plasma insulin levels.
After 12 weeks on RC or HF diet, mice were fasted overnight (16–18 hours). Following the overnight fast, glucose (1.5 mg/g body weight) was administered orally through a gavage tube. A blood sample was drawn from a tail vein at 0, 10, 20, 30, 60, 90, and 120 minutes following glucose administration, and blood glucose levels were measured using a Glucometer Elite blood glucose meter (Ascensia; Bayer HealthCare). For plasma insulin determinations, a blood sample (100 μl) was removed from the tail vein during the 10–20 minute time period following glucose administration. For ambient plasma insulin measurements, mice were euthanized following 20 weeks of HFF, and cardiac blood was obtained. Blood samples were immediately mixed with a 10% volume of a chilled solution containing 5,000 KIU/ml trasylol, 1.2 mg/ml EDTA, and 0.1 nM diprotin A. Plasma was separated by centrifugation at 4°C and stored at –80°C until assayed. Plasma was assayed for insulin using a mouse insulin ELISA kit (Linco). For calculation of plasma insulin/glucose ratios, plasma insulin (ng/ml) was divided by the average plasma glucose (mM) at the 10–20 minute time point after glucose administration.
Analysis of β cell area and β cell proliferation.
After 20 weeks of HFF, mice were injected with 100 mg/kg 5-bromo-2′-deoxyuridine (BrdU; Sigma-Aldrich) i.p. and sacrificed 5 hours later. The pancreas was dissected from surrounding tissue, fixed overnight in 5% glacial acetic acid/25% formaldehyde (vol/vol), and embedded in paraffin. Histologic sections were immunostained for insulin using rabbit anti-insulin (1:30 dilution; Dako) as primary antibody and biotinylated goat anti-rabbit (1:200 dilution; Vector Laboratories) as secondary antibody. The sections were then incubated with HRP-conjugated Ultra Streptavidin (ID Labs Inc.) for 30 minutes, and color was developed with freshly prepared 3,3′-diaminobenzidine tetrahydrochloride (DAB; Dako) solution. For assessment of β cell replication, pancreatic sections were double-stained for insulin, as described above, and for BrdU, using mouse anti-BrdU (1:1,000 dilution; Caltag Laboratories) as primary antibody. Following incubation with the primary antibody, sections were exposed to biotinylated horse anti-mouse IgG (1:200 dilution; Vector Laboratories) and subsequently stained with HRP-conjugated Ultra-Streptavidin (ID Labs Inc.), and color was developed with freshly made nickel-diaminobenzidine (NiDAB; Vector Laboratories Inc.) solution. The sections were examined using a Leica DMR microscope equipped with a Leica DC 300F video camera (Leica Microsystems) and connected to a computer with imaging software (QWin; Leica Microsystems). We quantified β cell area (area represented by insulin-immunopositive cells) using multiple histological sections from each pancreas and expressed the result as a percentage of total pancreatic area.
Insulin tolerance tests.
WT and single incretin receptor knockout mice were fasted for 5 hours and given 1.7 U/kg insulin (Humulin R, 100 U/ml; Lilly) by i.p. injection. However, DIRKO mice (and their respective WT controls) were instead given 1.2 U/kg insulin due to results of our pilot studies demonstrating significant, prolonged hypoglycemia after administration of 1.7 U/kg insulin (our unpublished observations).
Pancreatic insulin content.
The pancreas was homogenized twice in 5 ml of extraction medium [1 N HCl containing 5% (vol/vol) formic acid, 1% (vol/vol) trifluoroacetic acid, and 1% (wt/vol) NaCl] at 4°C. Peptides and small proteins were adsorbed from extracts by passage through a C18 silica cartridge (Waters). Adsorbed peptides were eluted with 4 ml of 80% (vol/vol) isopropanol containing 0.1% (vol/vol) trifluoroacetic acid. Pancreatic insulin levels were measured using a mouse insulin radioimmunoassay kit (Linco). Total protein levels in extracts were determined using the Bradford method with dye reagent (Bio-Rad).
Assessment of food intake.
Mice were fasted overnight (16–18 hours), weighed, and then placed into individual cages containing preweighed rodent chow, with free access to water. Food was reweighed after 24 hours, and food intake was expressed both as kcal consumed per gram body weight per day and as kcal per day.
Indirect calorimetry and locomotor activity.
After 15 weeks of HFF, mice were placed into individual metabolic chambers, with free access to food and water. Oxygen consumption was determined by indirect calorimetry using an Oxymax System (Columbus Instruments). Oxygen consumption was measured at 15-minute intervals for a total of 21 hours and was normalized to body weight.
Locomotor activity was measured in an independent group of WT mice, single incretin receptor knockout mice, and DIRKO mice. Locomotor activity was assessed as the total distance traveled, calculated from measurement of beam breaks in Opto M3 activity monitors (Columbus Instruments).
RNA preparation and quantitative real-time RT-PCR.
Total RNA was extracted from the pancreas using TRI zol (Sigma-Aldrich) and from epididymal and brown fat using the RNeasy Lipid Tissue Mini kit (Qiagen). First-strand cDNA was synthesized from total RNA using the SuperScript II synthesis system (Invitrogen) and random hexamers. Real-time quantitative PCR analysis was performed using TaqMan Gene Expression Assays and TaqMan Universal PCR Master Mix (Applied Biosystems) using the ABI Prism 7900 Sequence Detection System according to the protocols provided by the manufacturer (Applied Biosystems). The relative mRNA transcript levels were calculated according to the 2–ΔCT method (33), in which ΔCT represents the difference in threshold cycle values between the target mRNA and the 18S internal control.
Liver and adipose tissue morphologic analyses.
Livers were harvested, fixed in 10% neutral buffered formalin, and embedded in paraffin. Epididymal and brown fat pads were excised and embedded in paraffin. Sections were obtained and stained with H&E using standard protocols.
Measurement of plasma adipokines.
Following 20 weeks on RC or HF diet, mice were euthanized, and cardiac blood was obtained. Ambient levels of plasma leptin, resistin, and total PAI-1 were measured using the Mouse Serum Adipokine Lincoplex kit (Linco). Plasma adiponectin levels were determined using a mouse adiponectin ELISA kit (Linco).
Acute assessment of plasma adipokines in mice.
For analysis of the acute effects of the GLP-1R agonist Ex-4 or the GIPR agonist [D-Ala2]GIP (both from California Peptide Research) on plasma adipokines, 10-week-old male WT, Glp1r–/–, and Gipr–/– mice were fasted overnight, then injected i.p. with 24 nmol/kg of either [D-Ala2]GIP or Ex-4 immediately prior to oral glucose loading. At 45 minutes after administration of peptide and glucose, mice were euthanized, and cardiac blood was obtained and mixed with a 10% volume of a chilled solution containing 5,000 KIU/ml trasylol, 1.2 mg/ml EDTA, and 0.1 nM diprotin A. Plasma was separated by centrifugation at 4°C and stored at –80°C until assayed. Plasma leptin, PAI-1, and resistin were measured as described above.
Chronic administration of incretin receptor agonists to HF diet–fed WT mice.
WT mice were maintained on HF diet (45% kcal from fat) for 4 weeks starting at 6 weeks of age, following which mice were injected twice daily with 24 nmol/kg [D-Ala2]GIP or Ex-4 for 2 weeks.
Statistics.
All results are expressed as mean ± SEM. Statistical significance was assessed by ANOVA and, where appropriate, Student’s t test using GraphPad Prism (version 3; GraphPad Software). A P value less than 0.05 was considered to be statistically significant.
Supplementary Material
Acknowledgments
T. Hansotia was supported by a Canadian Institutes of Health Research (CIHR) Canadian Graduate Scholarship Doctoral Award and a studentship award from the Banting and Best Diabetes Centre. These studies were supported in part by operating grants from the Canadian Diabetes Association and the Juvenile Diabetes Research Foundation. D.J. Drucker is supported by a Canada Research Chair in Regulatory Peptides.
Footnotes
Nonstandard abbreviations used: β3AR, β3 adrenergic receptor; AUC, area under the curve; DIRKO, double incretin receptor knockout; Ex-4, exendin-4; GIP, glucose-dependent insulinotropic polypeptide; GIPR, GIP receptor; GLP-1, glucagon-like peptide–1; GLP-1R, GLP-1 receptor; HF, high-fat; HFF, high-fat feeding; PAI-1, plasminogen activator inhibitor–1; RC, regular chow; UCP-1, uncoupling protein–1.
Conflict of interest: D.J. Drucker has served as a consultant to Abbott Laboratories, Amgen Inc., Amylin Pharmaceuticals, Arisaph Pharmaceuticals Inc., Bayer Inc., Chugai Inc., Conjuchem Inc., Eli Lilly Inc., GlaxoSmithKline, Glenmark Pharmaceuticals, Johnson & Johnson, Merck Research Laboratories, Novartis Pharmaceuticals, NPS Pharmaceuticals Inc., Phenomix Inc., Takeda, and Transition Pharmaceuticals Inc. regarding the development of drugs based on incretin action for the treatment of type 2 diabetes. The remaining authors have declared that no conflict of interest exists.
Citation for this article: J. Clin. Invest. 117:143–152 (2007). doi:10.1172/JCI25483
Yuichiro Yamada’s present address is: Akita University School of Medicine, Akita, Japan.
Yutaka Seino’s present address is: Kansai Electric Power Hospital, Osaka, Japan.
Adriano Maida and Grace Flock contributed equally to this work.
References
- 1.Badman M.K., Flier J.S. The gut and energy balance: visceral allies in the obesity wars. Science. 2005;307:1909–1914. doi: 10.1126/science.1109951. [DOI] [PubMed] [Google Scholar]
- 2.Perley M.J., Kipnis D.M. Plasma insulin responses to oral and intravenous glucose: studies in normal and diabetic subjects. J. Clin. Invest. 1967;46:1954–1962. doi: 10.1172/JCI105685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Creutzfeldt W. The incretin concept today. Diabetologia. 1979;16:75–85. doi: 10.1007/BF01225454. [DOI] [PubMed] [Google Scholar]
- 4.Mayo K.E., et al. International Union of Pharmacology. XXXV. The glucagon receptor family. Pharmacol. Rev. 2003;55:167–194. doi: 10.1124/pr.55.1.6. [DOI] [PubMed] [Google Scholar]
- 5.Drucker D.J. Glucagon-like peptides: regulators of cell proliferation, differentiation, and apoptosis. Mol. Endocrinol. 2003;17:161–171. doi: 10.1210/me.2002-0306. [DOI] [PubMed] [Google Scholar]
- 6.Hansotia T., Drucker D.J. GIP and GLP-1 as incretin hormones: lessons from single and double incretin receptor knockout mice. Regul. Pept. 2005;128:125–134. doi: 10.1016/j.regpep.2004.07.019. [DOI] [PubMed] [Google Scholar]
- 7.Nauck M.A., et al. Preserved incretin activity of glucagon-like peptide 1 [7–36 amide] but not of synthetic human gastric inhibitory polypeptide in patients with type-2 diabetes mellitus. J. Clin. Invest. 1993;91:301–307. doi: 10.1172/JCI116186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gutniak M., Orskov C., Holst J.J., Ahren B., Efendic S. Antidiabetogenic effect of glucagon-like peptide-1 (7-36)amide in normal subjects and patients with diabetes mellitus. N. Engl. J. Med. 1992;326:1316–1322. doi: 10.1056/NEJM199205143262003. [DOI] [PubMed] [Google Scholar]
- 9.Dupre J., et al. Glucagon-like peptide I reduces postprandial glycemic excursions in IDDM. Diabetes. 1995;44:626–630. doi: 10.2337/diab.44.6.626. [DOI] [PubMed] [Google Scholar]
- 10.Turton M.D., et al. A role for glucagon-like peptide-1 in the central regulation of feeding. Nature. 1996;379:69–72. doi: 10.1038/379069a0. [DOI] [PubMed] [Google Scholar]
- 11.Young A.A., et al. Glucose-lowering and insulin-sensitizing actions of exendin-4: studies in obese diabetic (ob/ob, db/db) mice, diabetic fatty Zucker rats, and diabetic rhesus monkeys (Macaca mulatta). Diabetes. 1999;48:1026–1034. doi: 10.2337/diabetes.48.5.1026. [DOI] [PubMed] [Google Scholar]
- 12.Zander M., Madsbad S., Madsen J.L., Holst J.J. Effect of 6-week course of glucagon-like peptide 1 on glycaemic control, insulin sensitivity, and beta-cell function in type 2 diabetes: a parallel-group study. Lancet. 2002;359:824–830. doi: 10.1016/S0140-6736(02)07952-7. [DOI] [PubMed] [Google Scholar]
- 13.Tsukiyama K., et al. Gastric inhibitory polypeptide as an endogenous factor promoting new bone formation after food ingestion. Mol. Endocrinol. 2006;20:1644–1651. doi: 10.1210/me.2005-0187. [DOI] [PubMed] [Google Scholar]
- 14.Yip R.G., Wolfe M.M. GIP biology and fat metabolism. Life Sci. 2000;66:91–103. doi: 10.1016/s0024-3205(99)00314-8. [DOI] [PubMed] [Google Scholar]
- 15.Miyawaki K., et al. Inhibition of gastric inhibitory polypeptide signaling prevents obesity. Nat. Med. 2002;8:738–742. doi: 10.1038/nm727. [DOI] [PubMed] [Google Scholar]
- 16.Baggio L., Kieffer T.J., Drucker D.J. Glucagon-like peptide-1, but not glucose-dependent insulinotropic peptide, regulates fasting glycemia and nonenteral glucose clearance in mice. Endocrinology. 2000;141:3703–3709. doi: 10.1210/endo.141.10.7720. [DOI] [PubMed] [Google Scholar]
- 17.Scrocchi L.A., et al. Glucose intolerance but normal satiety in mice with a null mutation in the glucagon-like peptide 1 receptor gene. Nat. Med. 1996;2:1254–1258. doi: 10.1038/nm1196-1254. [DOI] [PubMed] [Google Scholar]
- 18.Miyawaki K., et al. Glucose intolerance caused by a defect in the entero-insular axis: a study in gastric inhibitory polypeptide receptor knockout mice. Proc. Natl. Acad. Sci. U. S. A. 1999;96:14843–14847. doi: 10.1073/pnas.96.26.14843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Scrocchi L.A., Marshall B.A., Cook S.M., Brubaker P.L., Drucker D.J. Identification of glucagon-like peptide 1 (GLP-1) actions essential for glucose homeostasis in mice with disruption of GLP-1 receptor signaling. Diabetes. 1998;47:632–639. doi: 10.2337/diabetes.47.4.632. [DOI] [PubMed] [Google Scholar]
- 20.Edwards C.M., et al. Glucagon-like peptide 1 has a physiological role in the control of postprandial glucose in humans: studies with the antagonist exendin 9- 39. Diabetes. 1999;48:86–93. doi: 10.2337/diabetes.48.1.86. [DOI] [PubMed] [Google Scholar]
- 21.Pederson R.A., et al. Enhanced glucose-dependent insulinotropic polypeptide secretion and insulinotropic action in glucagon-like peptide 1 receptor –/– mice. Diabetes. 1998;47:1046–1052. doi: 10.2337/diabetes.47.7.1046. [DOI] [PubMed] [Google Scholar]
- 22.Pamir N., et al. Glucose-dependent insulinotropic polypeptide receptor null mice exhibit compensatory changes in the enteroinsular axis. Am. J. Physiol. Endocrinol. Metab. 2003;284:E931–E939. doi: 10.1152/ajpendo.00270.2002. [DOI] [PubMed] [Google Scholar]
- 23.Preitner F., et al. Gluco-incretins control insulin secretion at multiple levels as revealed in mice lacking GLP-1 and GIP receptors. J. Clin. Invest. 2004;113:635–645. doi: 10.1172/JCI200420518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hansotia T., et al. Double incretin receptor knockout (DIRKO) mice reveal an essential role for the enteroinsular axis in transducing the glucoregulatory actions of DPP-IV inhibitors. Diabetes. 2004;53:1326–1335. doi: 10.2337/diabetes.53.5.1326. [DOI] [PubMed] [Google Scholar]
- 25.Drucker D.J., Philippe J., Mojsov S., Chick W.L., Habener J.F. Glucagon-like peptide I stimulates insulin gene expression and increases cyclic AMP levels in a rat islet cell line. Proc. Natl. Acad. Sci. U. S. A. 1987;84:3434–3438. doi: 10.1073/pnas.84.10.3434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fehmann H.C., Goke B. Characterization of GIP(1-30) and GIP(1-42) as stimulators of proinsulin gene transcription. Peptides. 1995;16:1149–1152. doi: 10.1016/0196-9781(95)00090-7. [DOI] [PubMed] [Google Scholar]
- 27.Robidoux J., Martin T.L., Collins S. Beta-adrenergic receptors and regulation of energy expenditure: a family affair. Annu. Rev. Pharmacol. Toxicol. 2004;44:297–323. doi: 10.1146/annurev.pharmtox.44.101802.121659. [DOI] [PubMed] [Google Scholar]
- 28.Unger R.H., Eisentraut A.M. Entero-insular axis. Arch. Intern. Med. 1969;123:261–266. [PubMed] [Google Scholar]
- 29.Nauck M.A., Bartels E., Orskov C., Ebert R., Creutzfeldt W. Additive insulinotropic effects of exogenous synthetic human gastric inhibitory polypeptide and glucagon-like peptide-1-(7-36) amide infused at near-physiological insulinotropic hormone and glucose concentrations. . J. Clin. Endocrinol. Metab. 1993;76:912–917. doi: 10.1210/jcem.76.4.8473405. [DOI] [PubMed] [Google Scholar]
- 30.Drucker D.J. Glucagon-like peptide-1 and the islet beta-cell: augmentation of cell proliferation and inhibition of apoptosis. Endocrinology. 2003;144:5145–5148. doi: 10.1210/en.2003-1147. [DOI] [PubMed] [Google Scholar]
- 31.Scrocchi L.A., Drucker D.J. Effects of aging and a high fat diet on body weight and glucose tolerance in glucagon-like peptide-1 receptor –/– mice. Endocrinology. 1998;139:3127–3132. doi: 10.1210/endo.139.7.6092. [DOI] [PubMed] [Google Scholar]
- 32.Flamez D., et al. Mouse pancreatic beta-cells exhibit preserved glucose competence after disruption of the glucagon-like peptide-1 receptor gene. Diabetes. 1998;47:646–652. doi: 10.2337/diabetes.47.4.646. [DOI] [PubMed] [Google Scholar]
- 33.Livak K.J., Schmittgen T.D. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) method. Methods. 2001;25:402–408.. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.