Cataract outcome is the result of surgical intervention for visual impairment or blindness due to cataract. It can be measured as visual acuity in the operated eye or in the patient, in terms of function, as quality of life and as economic rehabilitation. Of these, visual acuity is most suited to measure performance and monitor quality of service.
Clinical Trials: India and Nepal
Table 1 shows the outcome of cataract surgery in clinical trials under optimal conditions. More than 90% of eyes with cataract achieve a best-corrected visual acuity of 6/18 or better. The variation in visual outcome between various surgical techniques is minimal. Less than 3% of the operated patients had a best-corrected vision of less than 6/60. These clinical trial results may reflect one end of the spectrum, suggesting what may be possible in an ideal setting under very controlled circumstances. While setting general standards for hospitals in a developing country situation, this aspect would have to taken into account.
Table 1.
Visual Acuity by Percentage in the Operated Eye Following Cataract Surgery at 1-Year Follow-Up, in Hospital Based Studies in India and Nepal.1
| Visual acuity | Madurai, India | Lahan, Nepal | ||||
|---|---|---|---|---|---|---|
| ICCE + specs (n=1401) | ECCE + PC-IOL (n=1469) | ICCE + AC-IOL (n=311) | ECCE + PC-IOL (n=311) | ICCE + specs (n=259) | ECCE + specs (n=259) | |
| Presenting acuity | ||||||
| 6/6 – 6/18 | 84.9 | 83.9 | 44.7 | 54.3 | 59.8 | 58.3 |
| <6/18 – 6/60 | 2.9 | 15.4 | 49.8 | 42.4 | 36.7 | 39.4 |
| <6/60 | 12.2 | 0.6 | 5.5 | 3.2 | 3.5 | 2.3 |
| Best acuity | ||||||
| 6/6 – 6/18 | 95.5 | 98.1 | 90.4 | 93.3 | 93.0 | 91.5 |
| <6/18 – 6/60 | 2.9 | 1.3 | 7.1 | 4.8 | 6.6 | 7.3 |
| <6/60 | 1.6 | 0.6 | 2.6 | 1.9 | 0.4 | 1.2 |
Population-based Surveys in Asia
However, recent population-based surveys have shown that of all the patients operated on for cataract, 21–53% had a presenting visual acuity of less than 6/60. With best correction, 11–21% still had acuity less than 6/60 (Table 2). These figures include patients operated on recently as well as those who had surgery decades earlier. They include operations done under excellent as well as less favourable conditions, by experienced as well as less experienced eye surgeons. In brief, these results reflect the vision after cataract surgery in a cross-section of the population.
Table 2.
Long-term Outcome of Cataract Surgery from Population-based Studies in Asia
| % eyes with VA < 6/60 (95% CI) | ||||
|---|---|---|---|---|
| Place | Year published | No. of eyes | With available correction | With best correction |
| ∗40% <6/60 with pinhole correction | ||||
| Nepal2 | 1998 | 220 | 30.5 (24.4–36.6) | 10.9 (6.8–15.0) |
| Shunyi, China3 | 1998 | 116 | 44.8 (35.8–53.8) | |
| Doumen, China4 | 1999 | 152 | 52.6 (44.7–60.5) | 21.0 (14.5–27.5)∗ |
| Karnataka, India5 | 1999 | 2401 | 26.4 (24.6–28.2) | - |
| Ahmedabad, India5 | 1999 | 776 | 24.0 (21.0–27.0) | - |
| Hyderabad, India6 | 1999 | 131 | 21.4 (14.4 – 28.4) | 16.8 (10.4–23.2) |
| Punjab, India7 | 2000 | 428 | 23.1 (19.1–27.1) | - |
WHO Workshop on Outcomes, 1998
Poor visual acuity following surgery will affect the demand and uptake of cataract surgical services. Concerned about these results, the World Health Organization convened a workshop on Outcome in Prevention of Blindness Programmes in 1998. It recommended the development of a simple method to monitor and evaluate outcome following cataract surgery in terms of visual acuity, which can be assessed with full spectacle correction (‘best vision’) or with available correction (‘presenting vision’).8 The purposes of such a tool would be:

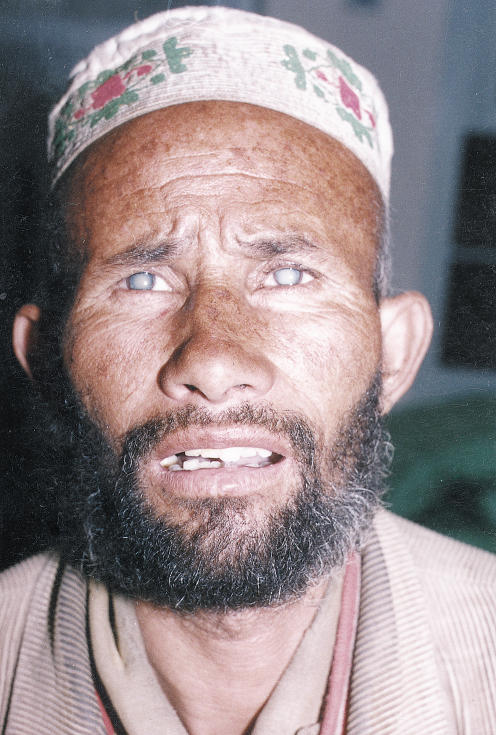
Right eye: mature cataract Left eye: aphakia
Photo: Pak Sang Lee
to identify causes of poor outcome of cataract surgery
to improve the outcome of cataract surgery
to increase the output of cataract surgical services.
Table 3 indicates outcome results which have been suggested to be adequate. These guidelines, however, do not specify a time frame for the assessment of outcome, the condition ‘cataract’ has not been specified, the cause of poor outcome is not assessed, and an instrument to measure outcome of cataract surgery has not been provided. Hence, there is a need for more operational research into these issues, and to standardise follow-up periods and conditions for visual acuity assessment. The aim of the monitoring tool is self-audit, not to compare outcomes between surgeons or institutions.
Table 3.
Adequate Outcome Results
| Post-operative acuity | Available correction | Best correction | |
|---|---|---|---|
| Good | 6/6 – 6/18 | >80% | > 90% |
| Borderline | <6/18 – 6/60 | <15% | <5% |
| Poor | <6/60 | <5% | <5% |
To measure visual outcome, individual patient records with well recorded pre- and post-operative visual acuity have to be analysed by tally sheet or by computer. Operated eyes with a presenting vision less than 6/60 should be examined to assess the major cause of poor visual outcome. Causes of poor outcome can be classified as:
pre-existing eye disease
surgical or post-operative complications
refractive errors
late post-operative complications.
In most of the population-based studies listed in Table 2, inadequate refractive correction and surgical complications were the major causes of poor outcome. Knowing the cause of poor outcome will enable eye surgeons and centres to address these causes and improve outcome, thereby increasing visual rehabilitation and the output of cataract surgical services.
Rapid Assessment and Monitoring Outcomes
Population-based rapid assessments of cataract surgical services are very useful to assess prevalence of cataract blindness and (pseudo) aphakia, cataract surgical coverage, barriers to cataract surgery and outcome. This is an average, long-term outcome, since past surgery varies greatly and patients would have been operated on by many surgeons in various settings. The causes of poor visual outcome can also be assessed. But because the impact of new improvements will be ‘diluted’ by old cases, population-based assessments are not the right tool to monitor short-term change. Routine monitoring of visual outcome of cataract surgery by individual surgeons or eye centres will increase awareness of outcome and provide a tool to achieve better results, thereby resulting in better ability and capacity to reduce cataract blindness.
Bilateral mature cataracts (with dilated pupils)
Photo: M Murtaza Farrahmand
Contributor Information
Lalit Dandona, Director, International Centre for Advancement of Rural Eye Care, L V Prasad Eye Institute, Banjara Hills, Hyderabad – 500 034, India.
Hans Limburg, Senior Research Fellow, International Centre for Eye Health, Institute of Ophthalmology, London ECIV 9EL, UK.
References
- 1.Foster A. Cataract – a global perspective: output, outcome and outlay. Eye. 1999;13:449–53. doi: 10.1038/eye.1999.120. [DOI] [PubMed] [Google Scholar]
- 2.Pokharel GP, Selvaraj S, Ellwein LB. Visual function and quality of life outcomes among cataract operated and unoperated blind populations in Nepal. Br J Ophthalmol. 1998;82:606–10. doi: 10.1136/bjo.82.6.606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhao J, Sui R, Jia L, et al. Visual acuity and quality of life outcomes in patients with cataract in Shunyi county, China. Am J Ophthalmol. 1998;126:515–23. doi: 10.1016/s0002-9394(98)00274-8. [DOI] [PubMed] [Google Scholar]
- 4.He M, Xu J, Li S, et al. Visual acuity and quality of life in patients with cataract in Doumen county, China. Ophthalmology. 1999;106:1609–15. doi: 10.1016/S0161-6420(99)90460-8. [DOI] [PubMed] [Google Scholar]
- 5.Limburg H, Foster A, Vaidyanathan K, et al. Monitoring visual acuity outcome of cataract surgery in India. Bull WHO. 1999;77:455–60. [PMC free article] [PubMed] [Google Scholar]
- 6.Dandona L, Dandona R, Naduvilath TJ, et al. Population-based assessment of the outcome of cataract surgery in an urban population in southern India. Am J Ophthalmol. 1999;127:650–58. doi: 10.1016/s0002-9394(99)00044-6. [DOI] [PubMed] [Google Scholar]
- 7.Anand R, Gupta A, Ram J, et al. Visual outcome following cataract surgery in rural Punjab. Indian J Ophthalmol. 2000;48:153–58. [PubMed] [Google Scholar]
- 8.Geneva: World Health Organization. WHO/PBL/98.68; Informal consultation on analysis of blindness prevention outcomes. [Google Scholar]