Everybody is aware of the annoyance and irritation caused by flies as they buzz around food and crawl over skin. In trachoma endemic areas, flies are frequently seen clustering around the face and eyes of children where they feed on mucus and discharge (Fig.1). This association of flies with the faces of infected children has not gone unnoticed, and they have been considered as vectors of trachoma for at least 400 years.1
Fig. 1.

Everted upper eyelid of a Gambian child with follicular trachoma and a feeding female bazaar fly (Musca sorbens)
Photo: Paul Emerson & Robin Bailey
Flies act as mechanical vectors of disease by picking up pathogens from infectious material and transferring them to an uninfected host. Flies have taste receptors on their front feet and when feeding they dip these into the food source as well as their proboscis. Thus, flies may be transferring Chlamydia trachomatis from the eyes of infected children to the eyes of uninfected people, on their feet and proboscis. However, the transmission of trachoma is poorly understood and there are other suggested routes which may be important in different places and at different times. Trying to prove that a particular route is operating, and establishing the relative importance of one route over another, is difficult. Until a recent intervention trial in The Gambia2 there has been little strong evidence to prove that flies actually are important in the transmission of trachoma.
In The Gambia, to determine whether flies were important in the transmission of trachoma, we removed them from the environment by ultra low volume spraying with an insecticide, deltamethrin. The study was conducted in two pairs of villages; one pair in the wet season, the other in the dry season. Spraying to control flies was carried out for three months in one village of each pair whilst the other acted as a control. The fly populations were monitored with traps and trachoma surveys were conducted across all age groups at baseline and at three months. Fly-eye contacts were monitored using handnets to collect flies landing on the faces of children to feed (Fig. 2). The prevalence of active trachoma was similar in the intervention and control villages at baseline, but after three months of fly control the prevalence of active trachoma was significantly lower in the intervention villages compared to the controls, in both seasons. Overall there was a reduction in the community prevalence of active trachoma associated with fly control of 61% (rate ratio 0.39 [95% confidence interval 0.20–0.77] p=0.007). Moreover, the number of new cases was significantly lower in the intervention villages than controls with an overall reduction of 75% in villages where fly control was practised (rate ratio 0.25 [0.09–0.64] p=0.003).
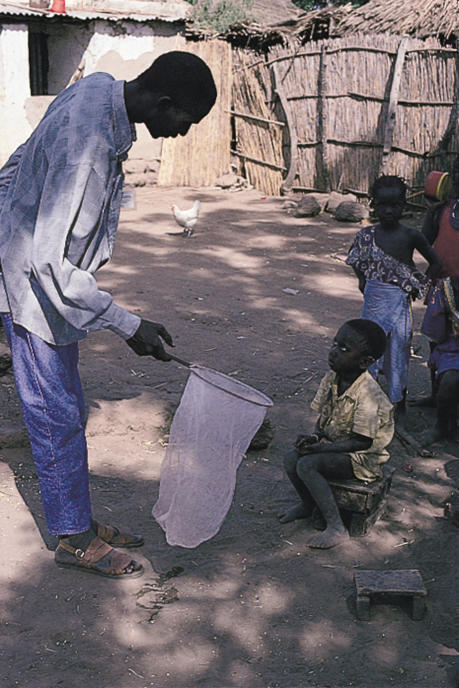
Fig. 2.
A Gambian field worker performing handnet collection of flies feeding on the ocular discharge of a child with active trachoma
Photo: Paul Emerson & Robin Bailey
In the same way that all mosquitoes do not transmit malaria - all flies do not transmit trachoma. In The Gambia, we have found evidence to suggest that the most likely vector of trachoma is the bazaar fly, Musca sorbens, and that other flies are not involved.3 The prevalence of trachoma falls when M. sorbens is removed from the environment. In addition, these flies are also present throughout the year in trachoma endemic communities, and frequently contact the eyes of children – particularly those with ocular discharge and Chlamydia trachomatis has been found on them.
Although our study suggested that insecticide spraying was effective in reducing trachoma transmission, it is unlikely to be feasible or sustainable in most trachoma-endemic areas.
Musca sorbens breeds in solid faeces lying on the ground, but does not breed in latrines, where the contents liquefy rapidly. In Egypt, less trachoma was found in households in which simple pit latrines were presen4 and this may be because they reduce the M. sorbens population by restricting its breeding habitat. Measures such as the identification and removal of faecal contamination in the environment and the provision of latrines need to be evaluated. We are currently investigating whether the community wide provision of pit latrines can have an impact on trachoma control. Any measures that can reduce fly-eye contact are likely to be of public health benefit in the control of trachoma and, therefore, the importance of flies should be incorporated into health/hygiene promotion programmes and school curricula. Though eyelid surgery and antibiotic treatment make an immediate impact, the ultimate success of the SAFE strategy for trachoma control is likely to depend on finding sustainable ways of reducing trachoma transmission. The neglected area of fly control deserves some attention.
References
- 1.Duke-Elder S, editor. Diseases of the Outer Eye. Part 1. London, Kimpton: 1965. Conjunctival diseases; pp. 260–99. Memoirs of the Bohemian Baron Harant of Poljitz(1598) [Google Scholar]
- 2.Emerson PM, Lindsay S, Walraven G, Faal H, Bogh C, Lowe K, Bailey RL. Effect of fly control on trachoma and diarrhoea. Lancet. 1999;353:1401–3. doi: 10.1016/S0140-6736(98)09158-2. [DOI] [PubMed] [Google Scholar]
- 3.Emerson PM, Bailey RL, Mahdi OSM, Lindsay SW. Transmission ecology of Musca sorbens, a putative vector of trachoma in The Gambia. Manuscript submitted to Transactions of the Royal Society of Tropical Medicine and Hygiene. [DOI] [PubMed]
- 4.Courtright P, Sheppard J, Lane S, Sadek A, Schachter J, Dawson CR. Latrine ownership as a protective factor in inflammatory trachoma in Egypt. Br J Ophthalmol. 1991;75(6):322–5. doi: 10.1136/bjo.75.6.322. [DOI] [PMC free article] [PubMed] [Google Scholar]