Introduction
Primary eye care activities cover the following two areas of community health services.1
Clinical service component
Eye health protection and promotion component
It is most important that most activities are initiated and sustained by community members themselves. The eye sector helps the community, complementing what they do in their day-by-day activities.
The essential elements of primary eye care should be determined by careful study providing a “community diagnosis”, based on an epidemiological approach. The study will list community eye problems in order of priority. To this end the study should be planned to include the following information:
Magnitude: M — prevalence and incidence, given by the number of community members suffering from particular conditions and new cases expected in a given period of time.
Implication: I — social and economic consequences from the condition, given in terms of expenditures, work loss, absence from school, etc.
Vulnerability: V — availability of effective means of intervention.
Cost: C — resources needed for control programmes.
Priority may be known from:2
Priority = (M×I×V) / C
This is a simple model illustrating scientific application in planning. It should avoid instinctive preferences based only on clinical experiences.
Service Components of Primary Eye Care
Service in the community should be sufficiently comprehensive to cover aspects of primary, secondary and tertiary prevention targeted for all community members whether they have or do not have eye problems. This is the point where community-based care differs from hospital-based services.
It begins with an understanding of any community at a point in time, and recognises three groups of people in need of eye care screening:
Healthy group.
The group with certain eye diseases or problems.
The group at risk of eye diseases or problems.
Hence, services should not only be clinical, but equal or more attention is needed for people without disease. Primary eye care, therefore, covers the whole range of eye health care for all community members.
Clinical Service Component
Community diagnosis precedes primary eye care activities and may give a different outlook regarding eye health of individual communities. This leads to adapted service components, according to social and economic standards, as well as the available system of health care. Essential elements, therefore, vary accordingly and may not include only the well known major blinding conditions. In addition, common eye disorders found in individual communities require simple but adequate services particular to that community. Decisions, therefore, should be made, not according to clinical interest, but from a public health point ofview. Conditions which are simple to prevent and manage and common to many communities are included in primary eye care services. This is true, for example, for reading problems among the elderly, and seasonal conjunctivitis may well need equal attention. In general, the World Health Organization provides the guidelines given on page 19.3
WHO GUIDELINES FOR PRIMARY EYE CARE
-
Conditions to be recognised and treated by a trained primary health care worker
-
Conjunctivitis and lid infectionsAcute conjunctivitisOphthalmia neonatorumTrachomaAllergic and irritative conjunctivitisLid lesions, e.g., stye and chalazion
-
TraumaSubconjunctival haemorrhagesSuperficial foreign bodyBlunt trauma
- Blinding malnutrition
-
-
Conditions to be recognised and referred after treatment has been initiated
- Corneal ulcers
- Lacerating or perforating injuries of the eyeball
- Lid lacerations
- Entropion/trichiasis
- Burns: chemical, thermal
-
Conditions that should be recognised and referred for treatment
- Painful red eye with visual loss
- Cataract
- Pterygium
- Visual loss; <6/18 in either eye
Based on the WHO guidelines and available data, the model initiated in Thailand, which started primary eye care in 1981, integrated the following conditions into primary health care:
Cataract (age-related/“senile” type)
-
Trachoma and its late complications
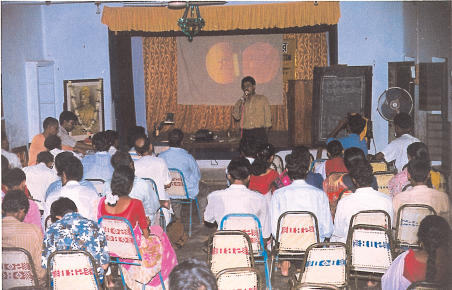
Discussion on the common eye diseases for community volunteers: mostly teachers, traditional healers and senior students. An ICEH slide set is being used. Vivekananda Mission Asram, West Bengal, IndiaPhoto: Anup, New Stylo, Chaitanyapur Eye injuries
Corneal ulcer
Glaucoma, acute attack and cases with one blind eye
Ophthalmia neonatorum
Eye infections
Pterygium∗
Refractive errors and reading difficulties
Conditions with visual acuity less than 0.05(<3/60)∗∗
Almost similar conditions were identified in Myanmar, then Burma, which also began primary eye care in 1981. Hence, all the above are essential elements in the clinical services of primary eye care in this part of the world. The same is also true for primary eye care in Vietnam, Laos and Cambodia, and even in China.
Other regions of the world have their own particular needs. For example, where onchocerciasis is highly prevalent, special action is needed in the primary eye care context.
Integration Matrix
Primary eye care should not be planned separately from primary health care. That is, primary eye care is regarded as an entry point, with primary health care, which goes to the heart of community. It is important to understand that primary health care is the mother system into which primary eye care, or basic eye care, is integrated. Careful situational analysis is, therefore, absolutely necessary for effective primary health care in the targeted community, with special attention to its essential elements.
Cultural evening on health care in India
Photo: Anup, New Stylo, Chaitanyapur
The matrix given in Table 1 shows how integration can proceed on the premise that health care is established.
Table 1.
Primary Eye Care Integration Matrix
| PHC PEC |
Health education | Family planning & MCH | Food & nutrition | Safe Water & basic sanitation | Extended programme of immunisation (∗∗) | Essential drugs | Control of local endemic diseases (∗∗∗∗) | Care for mild ailments (‘simple’ treatment) |
|---|---|---|---|---|---|---|---|---|
| (∗) In many instances, angle-closure glaucoma refers to the acute attack, with one eye already blind and prophylaxis required for the second eye. Secondary glaucoma is common among neglected age-related cataract patients. | ||||||||
| (∗∗) EPI staff are good health communicators, educators and gather community information. | ||||||||
| (∗∗∗) Diabetic retinopathy is common in some communities. This is the category 4 in the WHO categories of visual impairment. | ||||||||
| (∗∗∗∗) The cataract backlog might be regarded as an endemic disease in the given region, like tuberculosis, malaria and leprosy, etc. Trachoma, and its control is also relevant here. When the conditions are welt controlled, they become part of a successful integrated health programme in that locality. | ||||||||
|
Cataract Surgical Non-surgical |
+++ ++ |
+ for congenital cataract | NA | NA | NA | ++ post operation care |
+++ case finding, referral & community care |
+++ case finding, referral & community care |
|
Trachoma Active Complications |
+++ ++ |
+++ | +++ ++ |
NA | +++ tetracycline ointment |
trachoma programme +++ +++ |
trachoma programme +++ +++ |
|
|
Glaucoma Acute attack Angle-closed(∗) |
++ ++ |
+ for congenital glaucoma | NA | NA | NA | ++ pilocarpine eye drops |
++ pilocarpine eye drops |
|
| Eye injuries | ++ | +++ accident prevention |
++ improve environment |
NA | +++ tetracycline ointment |
+++ tetracycline ointment |
||
| Corneal ulcer | +++ | +++ accident prevention |
NA | NA | measles immunisation | +++ tetracycline ointment |
+++ tetracycline ointment |
|
|
Eye infections EKG Chronic |
++ ++ |
+++ ++ |
NA | ++ ++ |
NA | +++ ++ |
disaster management sometimes | +++ tetracycline ointment |
| Ophthalmia neonatorum | +++ | +++ | NA | +++ | +++ immediate referral |
|||
|
Pterygium Surgical Non-surgical |
++ + |
NA | NA | ++ ++ |
NA | NA | ++ referral |
|
| Refractive error & Reading difficulties | ++ | ++ family screening |
NA | NA | NA | + providing simple spectacles |
+ providing simple spectacles |
|
| VA less than 0.05 (< 3/60)(∗∗∗) | ++ | ++ family screening |
NA | NA | NA | NA | ++ referral |
|
Cataract Programmes and Primary Eye Care
A cataract programme can be a good example of primary eye care working effectively within the framework of primary health care. The success of these programmes, within primary eye care, has been seen in many countries.4 Activities largely rely on community involvement, as in case finding and mass referral. The surgical eye team can play its role cost effectively, provided the community preparations are completed well in advance of actual surgery.
The activities start with a short training course for community health workers in the recognition of cataract, followed by door-to-door visits. Multi-stage screening is part of primary eye care in case finding, and encouraging patients to present for surgery. At the same time, information on eye care should be made available throughout the community by all known means. Possible community activities are summarised in Table 2.
Table 2.
Cataract Programme at Community Level
| Level | Individual | Family | Community | 1st level of contact (Health Centre) | 1st level of referral (District Hospital) |
|---|---|---|---|---|---|
| Action | Aware of own vision. Slowly progressing, painless visual impairment, either one or both eyes. Respond to health workers after screening. Prompt report to eye team for operation. | Help bringing the cataract patient to eye unit. Encourage operation and prepare hospitalisation. Adequate postoperative care and suitable home and out-door activites. | Co-operate with health workers and visiting eye personnel in surgical care. Surgical subsidies for the poor. | Co-operate with visiting eye team in community activities. Co-ordinate community in the cataract programmes. | Co-operate with visiting eye team and preparation of service sites. Post-operative follow-up. Proper care for complicated cases. |
| Input | Health education, posters, booklets, etc. | Health education, posters, booklets, etc. | Primary eye care course. Primary eye care kits, manual and guidelines, records and reporting systems. | Primary eye care course, minimum supplies and equipment, records and reporting systems. | Short, clinical training, minimum required supplies and equipment. Monitoring/supervision. |
Footnotes
(∗ Highly prevalent in Thailand)
(∗∗ Implies possible cases with disorders of the posterior segment of the eye, which may need referral).
References
- 1.A Primary Health Care Approach. 1984. Strategies for the Prevention of Blindness in National Programmes; p. 12. WHO/Geneva. [Google Scholar]
- 2.Ruderman A P. General Economic Considerations. In: Reinke W A, editor. Health Planning, Qualitative Aspects and Quantitative Techniques. Baltimore: Wavery Press Inc.; 1978. pp. 114–6. [Google Scholar]
- 3. See 1 above at 26.
- 4.Srisuphan V. Proceedings of WHO Inter-country Workshop on Prevention of Blindness. Vientiane: Lao PDR; 1995. Mass Cataract Intervention in the Context of Primary Health Care; pp. 84–92. [Google Scholar]