An estimated 1 in 250 children are visually impaired as a result of eye disease. Some of these children have nearly normal vision, some are totally blind, but the majority fall into a broad range between these two points. Children are said to have ‘low vision’ or ‘partial sight’ when they have: (a) a corrected visual acuity in the better eye of <6/18 to ‘perception of light’ (or a visual field of less than 10 degrees); and (b) the ability to use their residual vision to orientate themselves or to perform tasks.1 They are identified at eye clinics, school screening programmes, community based rehabilitation (CBR) programmes or special schools for the visually impaired.
The education, employment prospects, independence and quality of life of a child with low vision can all be improved by enhancing vision. Optical devices (spectacles, magnifiers and telescopes) play a key role in achieving this. Studies carried out in East Africa,2 South America3 and West Africa4 indicate that approximately half of children who have low vision show an improvement in distance and/or near visual acuity with the help of spectacles, a magnifier or both. The majority of magnifiers are prescribed for children who have a visual acuity in the better eye of <6/60 to 1/60.3,4
The Role of Optical Services in the Management of Children with Low Vision
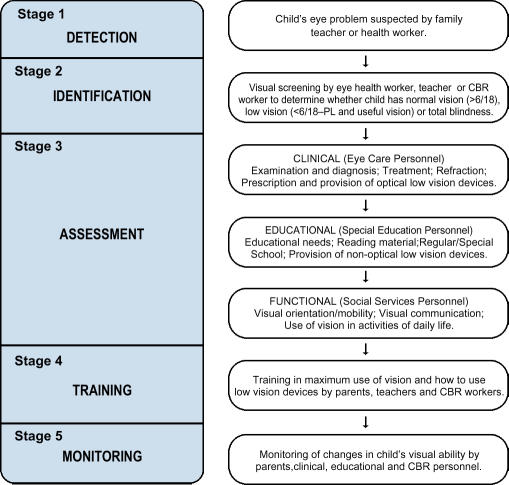
The management of children with low vision requires co-operation between the child, his/her family and eye care educational and social personnel. There are five stages in the management of children with low vision (Fig. 1). Eye care personnel are primarily involved in the assessment and monitoring stages which include: visual acuity measurement (distance and near); eye examination, diagnosis and prognosis; surgical and/or medical treatment; and the provision of optical services.
Fig. 1.
Stages in the Management of Children with Low Vision
Sight is a key source of stimulus during a child'sdevelopment, and so children with low vision should be motivated to make the maximum use of their residual vision. This can be done using both non-optical and optical methods.
Enhancing Vision Using Non-Optical Methods
Move CLOSER, e.g., use an angled reading desk
Use COLOUR to show objects more clearly
Use CONTRAST, e.g., eat white rice off a coloured plate
Pay attention to LIGHTING, e.g., sit near a window in class
Make objects LARGER, e.g., write with larger letters
Use a LINE-GUIDE such as a ruler when reading and writing.
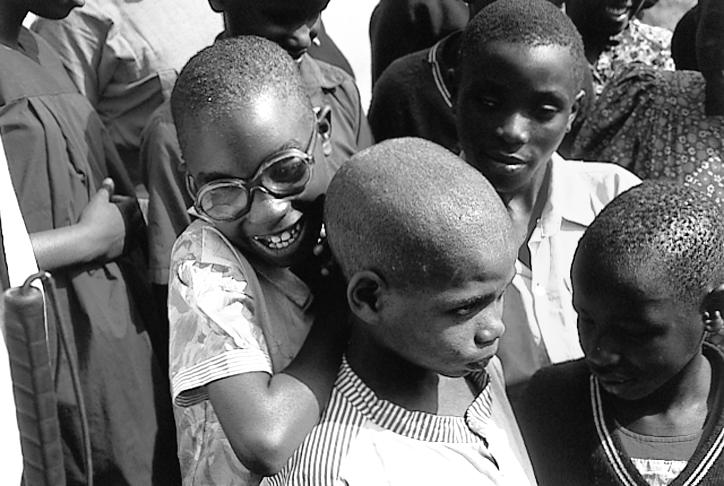
Accurate refraction and spectacle correction help many children with low vision
Photo: Murray McGavin
Enhancing Vision Using Optical Devices
Optical devices play a key role in enhancing vision and reducing visual disability in children with low vision. They include: standard prescription spectacles; optical low vision devices for distance vision; and optical low vision devices for near vision.
Standard prescription spectacles: It is important to ensure that children with low vision are refracted and provided with any spectacles they require. Work in West Africa indicates that at least 30% of children with low vision need spectacles.4 Refraction should always be carried out before a magnification assessment.
Optical low vision devices for distance vision: Distance vision magnification requires a telescopic lens system. Telescopes are expensive and have limited applications. It is often more practical for a child to sit near the front of class to see the backboard than to use a telscope.
Optical low vision devices for near vision: An optical low vision device for near vision uses one or more lenses placed between the eye and an object to alter the retinal image size of the object. This makes the object larger and easier to see. The minimum dioptric power of a device used in this way is +4.00D. These devices are inexpensive and have a wide range of applications. They play a vital role in giving children with low vision access to print and illustrations in standard textbooks.
Prescribing Magnifiers for Near Vision
The power of magnifier prescribed for a child is determined by the child'svisual requirements, recorded near visual acuity and measured working distance. They are prescribed, starting with low power magnifiers and then progressing to higher powers. The higher the power, the smaller the area of visual field seen through the magnifier. More words in a sentence can be viewed through a +10D magnifier than through a +20D magnifier. The power of the magnifier prescribed should be the maximum power which enables the child to perform the task required, but not above requirements so that maximum visual field is maintained. Moving the eye closer to the lens of a hand-held or stand magnifier also increases the field of view. In West Africa 71% of magnifiers prescribed were low power magnifiers (under +25D).4 These were prescribed more frequently for those with a visual acuity of 3/60 or better. High power magnifiers (over +25D) were prescribed in 29% of cases and were mainly prescribed for those with a visual acuity of less than 3/60.

Aphakic spectacle corrections after congenital cataract surgery for two Romanian children
Photo: Clare Gilbert
To determine the appropriate type of magnifier it is important to assess the child'spersonality, co-ordination, motivation and task aims. The same magnification can be provided using different mounting systems and working distances. Optical devices for near vision include: hand-held magnifiers (illuminated or non-illuminated); stand magnifiers (illuminated or non-illuminated); spectacle mounted magnifiers (e.g., high plus spectacle lenses, hyperocular lenses); and spectacle mounted telescopic units. The most widely available optical low vision devices for near vision are non-illuminated hand-held magnifiers, non-illuminated stand magnifiers, and high plus spectacle lenses. Advantages and disadvantages of these three types of magnifier are indicated in Table 1.
Table 1.
Practical Differences Between Magnifiers
| Hand-Held Magnifiers | Stand Magnifiers | High Plus Spectacle Lenses | |
|---|---|---|---|
| Uses |
|
|
|
| Advantages |
|
|
|
| Disadvantages |
|
|
|
There are many benefits in providing magnifiers to children with low vision. The magnifiers encourage children to use their low vision to the full, thereby increasing visual stimulus and helping the children'sdevelopment. The magnifiers promote literacy by increasing access to printed material for educational purposes and private reading. It is also more cost effective to provide children with optical devices enabling them to use standard books than to provide large print books which are expensive and heavy to carry.
There are some limitations in providing magnifiers. Using a magnifier may make a child'svisual disability more noticeable causing the child to feel different from other children. The human and financial resources available to provide the magnifiers may be limited. The child needs to be taught carefully how to use the magnifier as the restricted field of view can prevent a child from perceiving the overall pattern of words or sentences on a page.
Supply of Magnifiers
Low power magnifiers can be made easily using locally available materials. An optical workshop in Nairobi, Kenya developed a design using mounts made from plastic drain-pipe tubing. These are now used world-wide as they are inexpensive (approx. $6 each) and robust. Hand-held and stand magnifiers can be made in a range of powers from +8D to +28D. Instructions for making these are available from Christoffel Blindenmission, Nibelungenstrasse 124, D-64625 Bensheim, Germany. Higher power magnifiers can be imported from Combined Optical Industries Limited (COIL), UK or Eschenbach, Germany. These are made from lightweight, plastic aspheric lenses and cost between $6 (low power hand-held magnifier) and $34 (high power stand magnifier). They range in power from +8D to +76D.
Case Studies
In West Africa, 291 students with low vision were identified at eye clinics, special schools for the visually impaired, integration programmes and CBR programmes during 1995/6. All received an initial visual assessment including distance and near visual acuity measurement, refraction, magnification assessment and a quantitative measure of their level of functional vision. The functional vision tests included orientation, activities of daily life, ability to recognise pictures and reading speed. A follow-up assessment was received by 139 students. At first assessment (128/291) of the students showed an increase in distance or near visual acuity with an optical device. Potential to read normal print (N10 or better), with or without the help of spectacles and/or a magnifier, was shown by 55% (159/291) of students. Those who benefited were provided with optical devices and all the children with low vision received non-optical low vision devices and educational support. At follow-up assessment six months later, 63% (88/139) of students with low vision showed a further improvement in their distance visual acuity, near visual acuity and/or their functional vision. In special schools for the visually impaired in Ghana, 46% of students with low vision showed an improvement in reading and/or writing at their follow-up assessment.
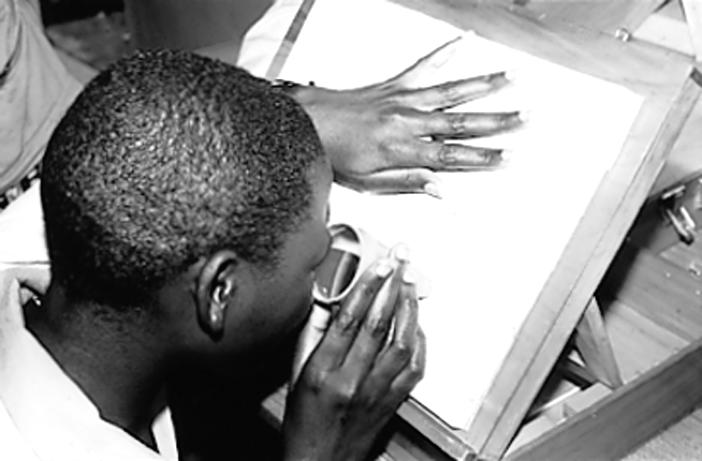
Using a stand magnifier for near vision
Photo: Lynne Ager
These figures indicate that correctly prescribed optical devices can be of significant benefit to the child with low vision and, therefore, the provision of optical services should be an integral part of any low vision service
References
- 1.WHO. The management of low vision in children. Proceedings of WHO/PBL consultation. July 1992. WHO, 1993; Bangkok. [Google Scholar]
- 2.Silver J, Gilbert C, Spoerer P, Foster A. Low vision in East African blind school students: need for optical low vision services. Br J Ophthalmol. 1995;79:814–20. doi: 10.1136/bjo.79.9.814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ager L R. London: Unpublished MSc Community Eye Health Dissertation, ICEH; 1994. Identifying children with low vision who benefit from magnifiers: a visual assessment of children at schools for the blind in Colombia and Ecuador. [Google Scholar]
- 4.Ager L R. Annual report of low vision services, Ghana National Eye Care Programme. 1996.