Abstract
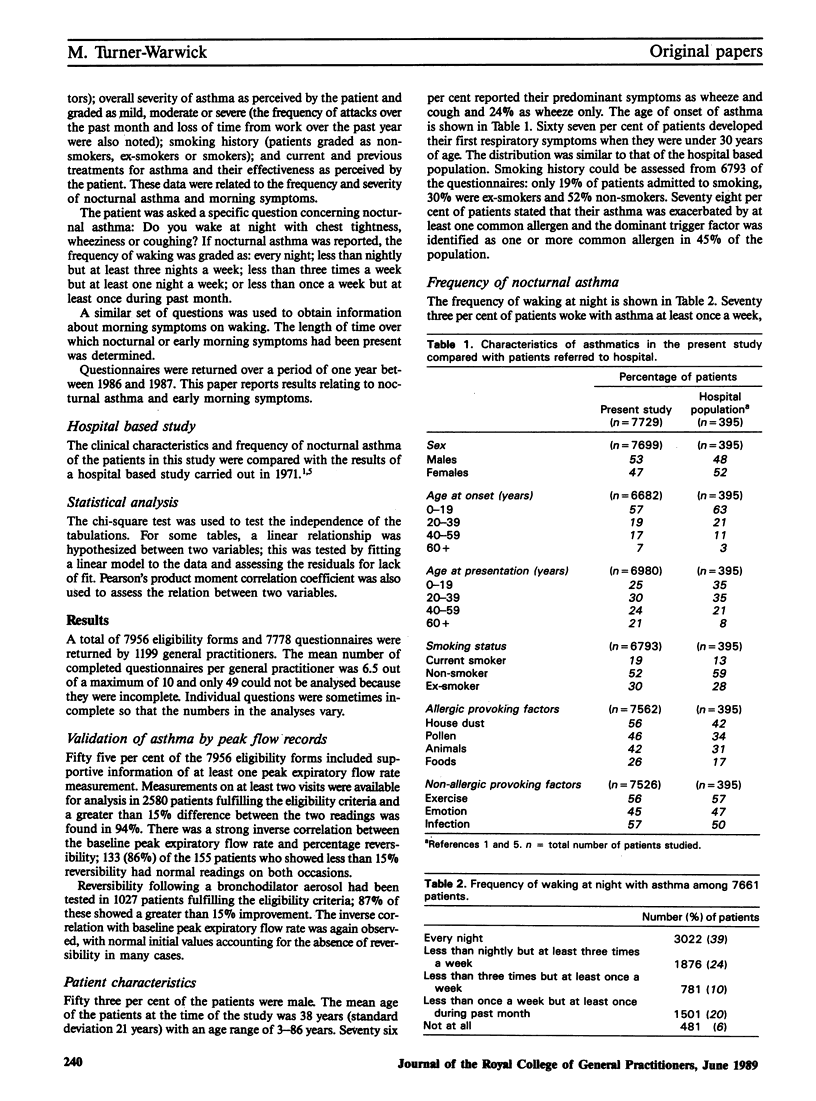
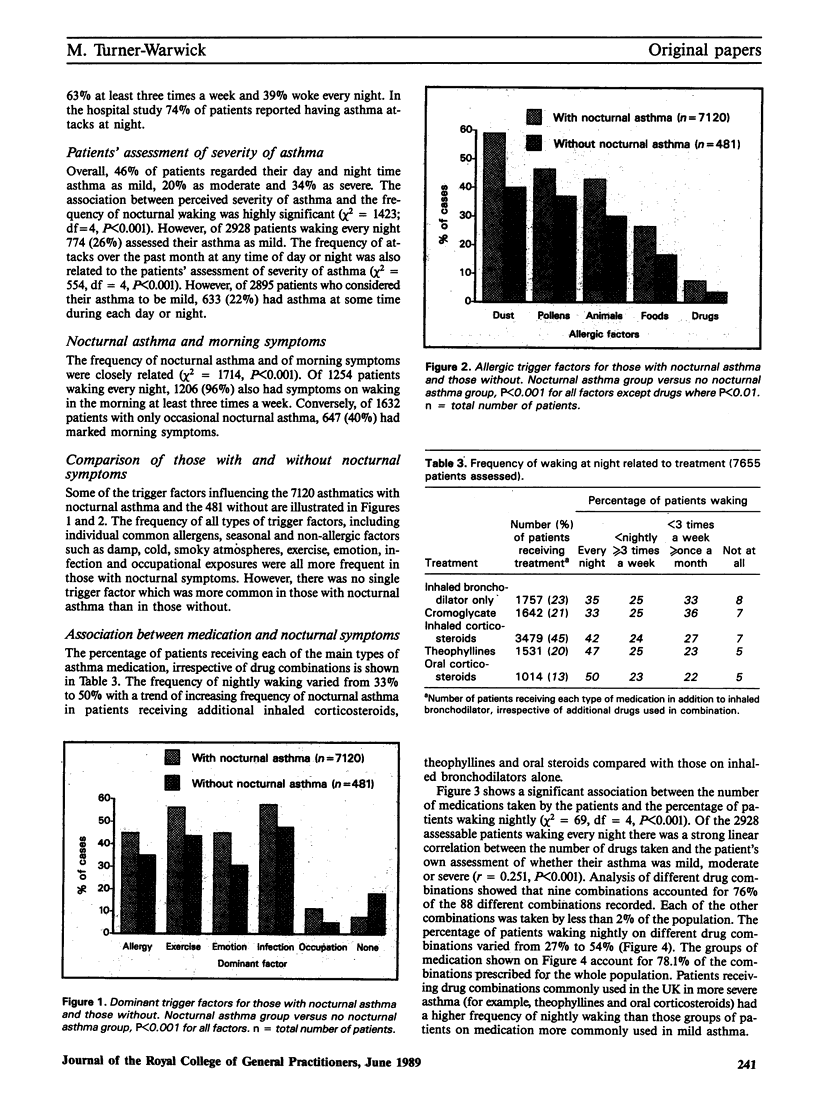
Symptoms of nocturnal asthma were studied using questionnaires returned by 1199 general practitioners throughout the United Kingdom. Of 7729 asthmatic patients seen consecutively and prescribed a bronchodilator aerosol, 73% woke with asthma at least once a week and 39% woke nightly. The percentage of asthmatics waking at night at least once a week in this population, where 48% were prescribed corticosteroid aerosols, was very similar to the 74% found to have asthma attacks at night in an earlier study of new hospital referrals at a time when such medication was not available. While sampling bias cannot be excluded, the clinical characteristics and profile of medications found in this study are similar to other reports and the evidence suggests that the general practitioners were managing these patients carefully. There was an overall association between the patients' perception of the severity of their asthma and frequency of waking at night (P less than 0.001). However, 26% of 2928 patients waking every night regarded their asthma as mild. These patients were taking significantly less medication than those also waking nightly but assessing their asthma as severe (P less than 0.001). The seriousness of nocturnal symptoms may be underestimated by asthmatics and they should be asked specifically about the frequency of nocturnal waking. Those with nocturnal asthma had a generally higher frequency of allergic and non-allergic provoking factors, but no single factor distinguished these patients from those without nocturnal symptoms. There was a strong correlation between the frequency of nightly waking and the number of medications used (P less than 0.001).(ABSTRACT TRUNCATED AT 250 WORDS)
Full text
PDF


Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Barnes P. J., Greening A. P., Neville L., Timmers J., Poole G. W. Single-dose slow-release aminophylline at night prevents nocturnal asthma. Lancet. 1982 Feb 6;1(8267):299–301. doi: 10.1016/s0140-6736(82)91566-5. [DOI] [PubMed] [Google Scholar]
- Broder I., Higgins M. W., Mathews K. P., Keller J. B. Epidemiology of asthma and allergic rhinitis in a total community, Tecumseh, Michigan. 3. Second survey of the community. J Allergy Clin Immunol. 1974 Mar;53(3):127–138. doi: 10.1016/0091-6749(74)90001-3. [DOI] [PubMed] [Google Scholar]
- Connolly C. K. Diurnal rhythms in airway obstruction. Br J Dis Chest. 1979 Oct;73(4):357–366. [PubMed] [Google Scholar]
- Dodge R. R., Burrows B. The prevalence and incidence of asthma and asthma-like symptoms in a general population sample. Am Rev Respir Dis. 1980 Oct;122(4):567–575. doi: 10.1164/arrd.1980.122.4.567. [DOI] [PubMed] [Google Scholar]
- Hay I. F., Higenbottam T. W. Has the management of asthma improved? Lancet. 1987 Sep 12;2(8559):609–611. doi: 10.1016/s0140-6736(87)92995-3. [DOI] [PubMed] [Google Scholar]
- Hendrick D. J., Davies R. J., D'Souza M. F., Pepys J. An analysis of skin prick test reactions in 656 asthmatic patients. Thorax. 1975 Feb;30(1):2–8. doi: 10.1136/thx.30.1.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li J. T., Reed C. E. Nocturnal asthma and timing of treatment. Am J Med. 1985 Dec 20;79(6A):10–15. doi: 10.1016/0002-9343(85)90081-6. [DOI] [PubMed] [Google Scholar]
- Welsh P. W., Reed C. E., Conrad E. Timing of once-a-day theophylline dose to match peak blood level with diurnal variation in severity of asthma. Am J Med. 1986 Jun;80(6):1098–1102. doi: 10.1016/0002-9343(86)90671-6. [DOI] [PubMed] [Google Scholar]