Abstract
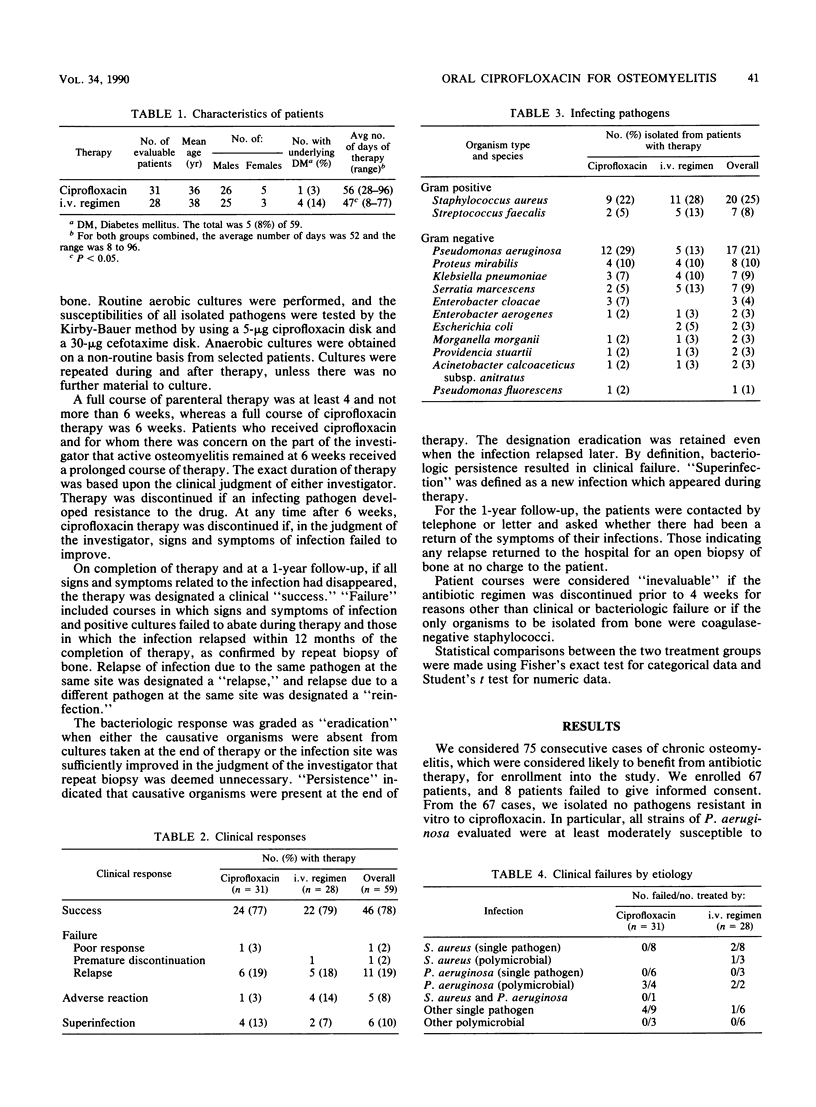
We undertook a prospective, randomized comparison of oral ciprofloxacin with standard parenteral therapies for the treatment of biopsy-proven osteomyelitis caused by susceptible organisms. Following surgical debridement, the ciprofloxacin patients received 750 mg twice a day, and the other patients received a broad-spectrum cephalosporin or a nafcillin-aminoglycoside combination intravenously (i.v.). There were 31 evaluable patients in the ciprofloxacin group, treated an average of 56 days, and 28 in the i.v. group, treated an average of 47 days. Clinical success rates were 24 of 31 (77%) for the ciprofloxacin group and 22 of 28 (79%) for the i.v. group. Of the seven failures in the ciprofloxacin group, one was due to a persistent Klebsiella pneumoniae infection and six were due to relapse of the infection within 1 year of therapy. Of the six failures in the i.v. group, one was due to an Enterobacter aerogenes strain which emerged resistant and five were due to relapse. The most troublesome etiology was polymicrobial osteomyelitis involving Pseudomonas aeruginosa, in which five of six (83%) regimens failed. Adverse reactions occurred infrequently, i.e., in 1 of 31 (3%) of the ciprofloxacin patients and in 4 of 28 (14%) of the i.v. patients, yet all reactions responded to therapy and none required protocol deviation. Our data indicate that oral ciprofloxacin monotherapy is as safe and effective as conventional parenteral therapy in cases of osteomyelitis caused by susceptible organisms.
Full text
PDF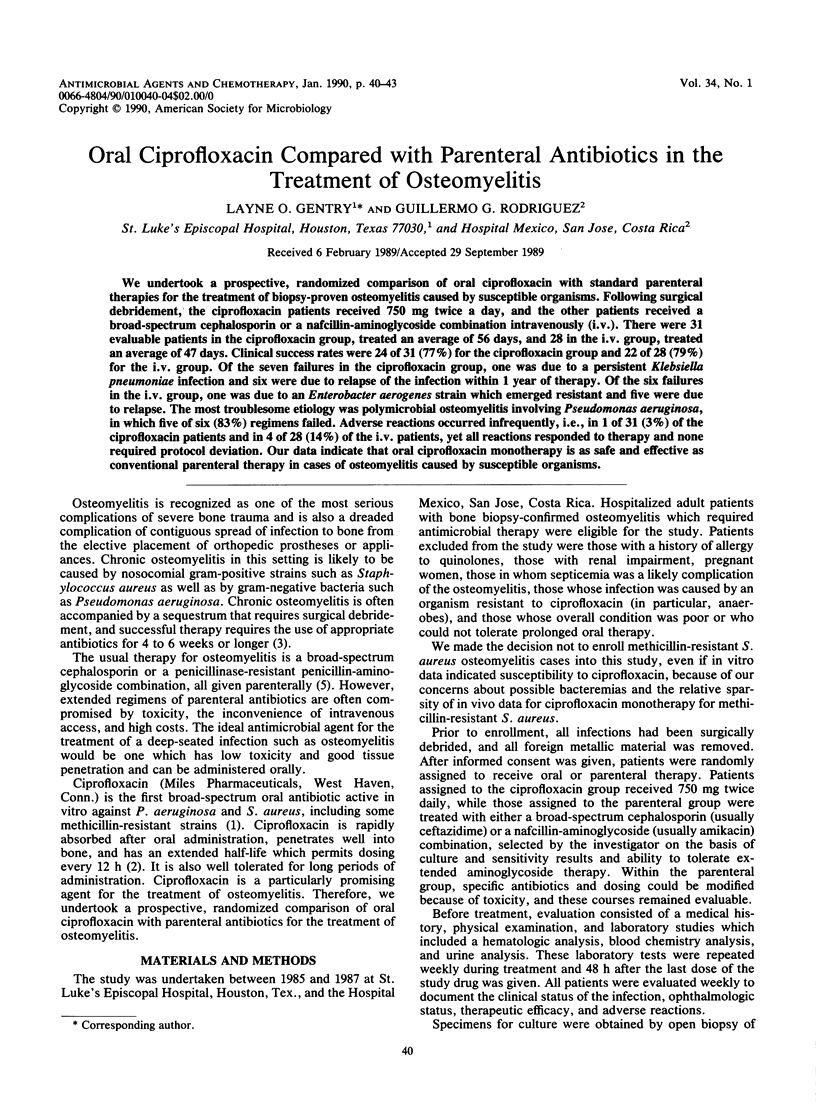


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Chin N. X., Neu H. C. Ciprofloxacin, a quinolone carboxylic acid compound active against aerobic and anaerobic bacteria. Antimicrob Agents Chemother. 1984 Mar;25(3):319–326. doi: 10.1128/aac.25.3.319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crump B., Wise R., Dent J. Pharmacokinetics and tissue penetration of ciprofloxacin. Antimicrob Agents Chemother. 1983 Nov;24(5):784–786. doi: 10.1128/aac.24.5.784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gentry L. O. Osteomyelitis: options for diagnosis and management. J Antimicrob Chemother. 1988 Apr;21 (Suppl 100):115–131. doi: 10.1093/jac/21.suppl_c.115. [DOI] [PubMed] [Google Scholar]
- Smith J. T. The mode of action of 4-quinolones and possible mechanisms of resistance. J Antimicrob Chemother. 1986 Nov;18 (Suppl 500):21–29. doi: 10.1093/jac/18.supplement_d.21. [DOI] [PubMed] [Google Scholar]
- Waldvogel F. A., Papageorgiou P. S. Osteomyelitis: the past decade. N Engl J Med. 1980 Aug 14;303(7):360–370. doi: 10.1056/NEJM198008143030703. [DOI] [PubMed] [Google Scholar]


