Abstract
Increased insulin secretion and expansion of pancreatic β cell mass work together to maintain normal glucose levels when insulin resistance develops. Changes in glucose concentration have long been known to have profound effects upon the rates of insulin secretion and β cell mass, but various other agents can also cause changes, raising questions about which mechanisms are dominant. Evidence favoring a dominant role for glucose is provided by Terauchi et al. in this issue of the JCI (see the related article beginning on page 246). Mice haploinsufficient for β cell glucokinase (Gck) were unable to increase their β cell mass in response to insulin resistance produced by high-fat feeding. Gck is known to be the glucose sensor for glucose metabolism in β cells. The study also provides strong evidence that insulin receptor substrate 2 (Irs2), which is known to have major effects on β cell growth and survival, is a key downstream mediator of the effects of glucose found in this study.
When faced with the insulin resistance imposed by obesity and the sedentary life-styles of our industrialized societies, blood glucose levels remain in the normal range thanks to precisely regulated increases of insulin secretion. Some of this increase is due to increases in pancreatic β cell mass that can be dramatic in rodents (1) but are more modest in humans. Obese humans have β cell masses about 50% greater than those of normal-weight controls, but this mean value does not reflect the considerable variability found in a large number of autopsy specimens from obese individuals (2, 3). The mass of β cells can be increased through β cell replication, β cell hypertrophy, or formation of new islets through neogenesis (4). In adult rodents the dominant mechanism appears to be β cell replication, while the dominant mechanism in humans remains unclear.
The capacity of β cell mass to increase in the face of insulin resistance is very important because it usually prevents the development of type 2 diabetes (T2D), yet this compensation fails often enough to be a major culprit in the current epidemic of diabetes. It is now accepted that β cell mass in T2D is about 50% of normal and that this reduction is fundamental to T2D pathogenesis (2). There is great interest in the mechanisms of β cell expansion and maintenance, and the study by Terauchi and colleagues in this issue of the JCI highlights the importance of glucose signaling in this process (5). While normal mice in response to high-fat feeding have an increase in β cell mass, mice haploinsufficient for β cell glucokinase (Gck+/– mice) do not. Gck is the key rate-limiting enzyme in glucose metabolism in β cells and has been convincingly shown to be the glucose sensor for glucose-stimulated insulin secretion (GSIS) (6). While it has long been known that glucose can stimulate β cell replication, the role of Gck in this process was previously not well defined.
Physiologic arguments that glucose is the dominant factor in β cell compensation for insulin resistance
There has been much debate about whether the increased insulin secretion and β cell mass accompanying insulin resistance can be explained by glucose signaling. An often-asked question is: How can glucose be the signal for increased insulin secretion in individuals who have “normal” glucose levels? It can be argued that regulation is so precise that changes in glucose levels cannot be measured, like a good thermostat system, or that subtle glucose increases after meals or at night might be influential. Another possibility is that the activity of Gck could be enhanced and/or that hexokinase expression is increased such that the set point for GSIS could be lowered (7, 8).
Although these hypotheses are attractive because control of β cell function is so dominated by glucose, other possibilities must be considered. In a canine model of high-fat feeding, a combination of low to normal fasting glucose levels and high plasma insulin levels could possibly be explained by a stimulatory effect of high free fatty acid levels on insulin secretion (9). It is instructive, however, that in the present Gck-deficient model, expansion of β cell mass did not occur in spite of an increase in circulating free fatty acids equal to that in high-fat–fed controls (5). Other circulating factors capable of stimulating β cell replication include prolactin, growth hormone, Igf1, and glucagon-like peptide 1 (Glp1), but there is little reason to implicate these as having a major role in common insulin-resistant states. Nonetheless, various plasma factors are likely to have important permissive or contributing roles in the regulation of β cell mass, which are secondary to the dominant effects of glucose. The hypothesis that insulin may serve as a paracrine or autocrine signal for growth is discussed below.
Downstream pathways of glucose signaling in β cells
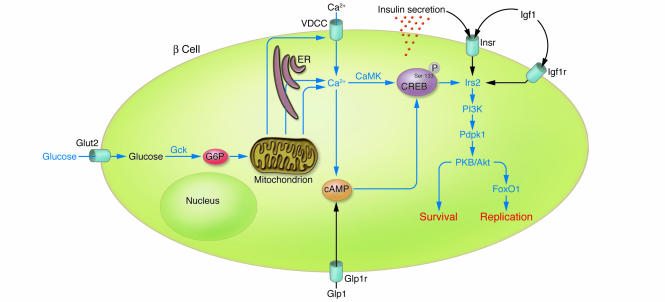
The present work by Terauchi et al. (5) provides strong evidence that glucose signaling is important for the expansion of β cell mass that is associated with insulin resistance and shines a spotlight on Irs2, which has already been implicated as a key mediator of β cell growth and survival (10, 11). Two strong mediators of β cell replication, glucose and Glp1 (the latter acting through cAMP), depend upon Irs2 for their efficacy (12). How does glucose enhance the expression of Irs2 and then β cell replication? The present study, building on other work, provides an outline of underlying mechanisms (Figure 1). Terauchi et al. (5) hypothesize that impaired intracellular calcium responses to glucose fail to trigger cAMP-responsive element–binding protein (CREB) Ser133 phosphorylation, which would in turn account for the lack of change in Irs2 levels (13). Although decreased glucose oxidation in isolated islets might be expected to correlate with these calcium changes, no such relationship was found. We should not make too much of this lack of correlation. Glucose oxidation is only one aspect of glucose metabolism; in vitro measurement of oxidation on isolated islets may have missed some important signal from metabolism in vivo. The search for signals from glucose metabolism that are responsible for the KATP-independent pathway of GSIS underscores the complexity of these glucose signaling mechanisms.
Figure 1. The pathway from glucose metabolism to increased β cell mass through enhanced β cell replication and survival.
Glucose enters the β cell via glucose transporter 2 (Glut2; also known as Slc2a2) and is phosphorylated to glucose-6-phosphate (G6P) by the rate-limiting enzyme of glycolysis, Gck. Further metabolism of glucose increases the expression of Irs2, possibly through CREB phosphorylation at residue Ser133 as a result of increased cytosolic calcium levels generated via voltage-dependent calcium channels (VDCCs), the ER, and mitochondria. The calcium effect is likely mediated by calmodulin-dependent protein kinases (CaMKs). Calcium can also increase cAMP levels in β cells. Increased Irs2 activity can then activate a signalling cascade that leads to β cell replication (via FoxO1 nuclear exclusion) and β cell survival (via PKB/Akt). This pathway can be augmented by cAMP signaling through GLP1 receptors (Glp1r). The contributions of the insulin and Igf1 receptors (Insr and Igf1r, respectively) are likely to be permissive. P, phosphate group.
In addition, downstream of Irs2 is the presumed cascade of PI3K, 3-phosphoinositide–dependent protein kinase-1 (Pdpk1), and PKB/Akt signaling. Downstream of PKB/Akt, the signaling steps are less clear, but the finding of decreased nuclear exclusion of the forkhead transcription factor FoxO1 in the Gck+/– mice (5) seems important because of its previously demonstrated role in β cell compensation for insulin resistance (14). How activation of PKB and FoxO1 nuclear exclusion affect cell cycle mechanisms of replication is more difficult to understand, but clues may be provided by the finding in the present study that in the Gck+/– mice, expression of cyclin D2 was decreased and that of p15 inhibitor was increased (5).
Glucose versus insulin as a mediator of β cell growth
The issue of insulin versus glucose signaling also merits discussion. It can be argued that glucose exerts its effects on β cell growth by stimulating insulin secretion, which then feeds back on the β cell to promote growth. This is challenged by a recent report that demonstrated glucose stimulation of Irs2 expression can be dissociated from insulin secretion by using somatostatin, which inhibits the distal steps of insulin secretion (15). Also instructive is the observation that separately knocking out the insulin or Igf1 receptors on β cells has surprisingly little effect upon β cell mass (16, 17). The double knockout of both receptors is associated with β cell mass that is normal at birth but then decreases as glucose levels increase, demonstrating that glucose signaling alone cannot maintain β cell mass (18). While it is tempting to conclude that the ligands insulin and/or Igf1 are important, it is possible that loss of the receptors alone, even in the absence of the ligand, can lead to impairment of the insulin signaling pathways upon which glucose effects depend. A mysterious, but likely important, finding of the present study is the increase in expression of the Igf1 receptor in the islets of high-fat–fed wild-type mice (5). Was this change influenced by either the Igf1 or insulin ligands? Perhaps not. Another instructive result is that a double knockout of the genes encoding insulin 1 and 2 in mice results in an increase in β cell mass at birth followed by death of the mice from hyperglycemia (19). Because insulin deficiency in the fetus can raise fetal blood glucose levels (20), and because maternal diabetes leads to fetal β cell expansion, it is attractive to propose that glucose is driving the hyperplasia in the absence of insulin. The primacy of glucose (over insulin) is also demonstrated by the hypoglycemia caused by insulin-producing tumors, which leads to marked reduction of β cell mass (21). Another test of the insulin signaling hypothesis comes from experiments with global heterozygous knockouts of Irs1 and the insulin receptor, which result in severe insulin resistance and massive β cell hyperplasia (1). In this situation, haploinsufficiency of insulin receptors on β cells has no discernible inhibitory effect on β cell expansion. Taken together, these findings cast doubt on the likelihood that insulin or Igf1 play more than a possible permissive role in the β cell expansion of insulin resistance. Perhaps what have been called the insulin signaling pathways in β cells should be viewed as growth and survival pathways used by glucose, cAMP, and a variety of growth factors. Although we have focused on the obviously important Irs2/PI3K/PKB pathway, the complete picture of the signals responsible for β cell growth is no doubt far more complex.
The fact that this tidy reduction of Gck in β cells prevents β cell expansion in an excellent model of insulin resistance (5) adds great strength to the hypothesis that glucose is the dominant force responsible for this important compensatory mechanism. But, as with any hypothesis, future rigorous challenge is awaited. Nonetheless, because of the importance of β cell failure in T2D and the power of new therapeutic approaches, it is essential that glucose signals involved in β cell replication in both health and disease be carefully defined.
Acknowledgments
The authors thank Christopher J. Rhodes for helpful discussion and advice.
Footnotes
Nonstandard abbreviations used: CREB, cAMP-responsive element–binding protein; Gck, glucokinase; Glp1, glucagon-like peptide 1; GSIS, glucose-stimulated insulin secretion; Irs, insulin receptor substrate; T2D, type 2 diabetes.
Conflict of interest: The authors have declared that no conflict of interest exists.
Citation for this article: J. Clin. Invest. 117:81–83 (2007). doi:10.1172/JCI30862.
See the related article beginning on page 246.
References
- 1.Bruning J.C., et al. Development of a novel polygenic model of NIDDM in mice heterozygous for IR and IRS-1 null alleles. Cell. 1997;88:561–572. doi: 10.1016/s0092-8674(00)81896-6. [DOI] [PubMed] [Google Scholar]
- 2.Butler A.E., et al. Beta-cell deficit and increased beta-cell apoptosis in humans with type 2 diabetes. Diabetes. 2003;52:102–110. doi: 10.2337/diabetes.52.1.102. [DOI] [PubMed] [Google Scholar]
- 3.Ritzel R.A., Butler A.E., Rizza R.A., Veldhuis J.D., Butler P.C. Relationship between beta-cell mass and fasting blood glucose concentration in humans. Diabetes Care. 2006;29:717–718. doi: 10.2337/diacare.29.03.06.dc05-1538. [DOI] [PubMed] [Google Scholar]
- 4.Bonner-Weir S. Perspective: postnatal pancreatic beta cell growth. Endocrinology. 2000;141:1926–1929. doi: 10.1210/endo.141.6.7567. [DOI] [PubMed] [Google Scholar]
- 5.Terauchi Y., et al. Glucokinase and IRS-2 are required for compensatory β cell hyperplasia in response to high-fat diet–induced insulin resistance. J. Clin. Invest. 2007;117:246–257. doi: 10.1172/JCI17645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Matschinsky F.M. A lesson in metabolic regulation inspired by the glucokinase glucose sensor paradigm. Diabetes. 1996;45:223–241. doi: 10.2337/diab.45.2.223. [DOI] [PubMed] [Google Scholar]
- 7.Chen C., Hosokawa H., Bumbalo L.M., Leahy J.L. Regulatory effects of glucose on the catalytic activity and cellular content of glucokinase in the pancreatic B cell. J. Clin. Invest. 1994;94:1616–1620. doi: 10.1172/JCI117503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hosokawa H., Hosokawa Y.A., Leahy J.L. Upregulated hexokinase activity in isolated islets from diabetic 90% pancreatectomized rats. Diabetes. 1995;44:1328–1333. doi: 10.2337/diab.44.11.1328. [DOI] [PubMed] [Google Scholar]
- 9.Kim S.P., Catalano K.J., Hsu I.R., Chiu J.D., Bergman R. Elevated nocturnal FFA may be the signal for compensatory hyperinsulinemia for insulin resistance induced by a high fat diet in the dog model [abstract]. Obes. Res. . 2004;11(Suppl. 1):A14. [Google Scholar]
- 10.Withers D.J., et al. Disruption of IRS-2 causes type 2 diabetes in mice. Nature. 1998;391:900–904. doi: 10.1038/36116. [DOI] [PubMed] [Google Scholar]
- 11.Rhodes C.J. Type 2 diabetes-a matter of beta-cell life and death? Science. 2005;307:380–384. doi: 10.1126/science.1104345. [DOI] [PubMed] [Google Scholar]
- 12.Park S., et al. Exendin-4 uses Irs2 signaling to mediate pancreatic beta cell growth and function. . J. Biol. Chem. 2006;281:1159–1168. doi: 10.1074/jbc.M508307200. [DOI] [PubMed] [Google Scholar]
- 13.Jhala U.S., et al. cAMP promotes pancreatic beta-cell survival via CREB-mediated induction of IRS2. Genes Dev. 2003;17:1575–1580. doi: 10.1101/gad.1097103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Okamoto H., et al. Role of the forkhead protein FoxO1 in β cell compensation to insulin resistance. . J. Clin. Invest. 2006;116:775–782. doi: 10.1172/JCI24967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lingohr M.K., et al. Specific regulation of IRS-2 expression by glucose in rat primary pancreatic islet beta-cells. J. Biol. Chem. 2006;281:15884–15892. doi: 10.1074/jbc.M600356200. [DOI] [PubMed] [Google Scholar]
- 16.Kulkarni R.N., et al. Tissue-specific knockout of the insulin receptor in pancreatic b cells creates an insulin secretory defect similar to that in type 2 diabetes. Cell. 1999;96:329–339. doi: 10.1016/s0092-8674(00)80546-2. [DOI] [PubMed] [Google Scholar]
- 17.Kulkarni R.N., et al. beta-cell-specific deletion of the Igf1 receptor leads to hyperinsulinemia and glucose intolerance but does not alter beta-cell mass. Nat. Genet. 2002;31:111–115. doi: 10.1038/ng872. [DOI] [PubMed] [Google Scholar]
- 18.Ueki K., et al. Total insulin and IGF-I resistance in pancreatic beta cells causes overt diabetes. Nat. Genet. 2006;38:583–588. doi: 10.1038/ng1787. [DOI] [PubMed] [Google Scholar]
- 19.Duvillie B., et al. Phenotypic alterations in insulin-deficient mutant mice. Proc. Natl. Acad. Sci. U. S. A. 1997;94:5137–5140. doi: 10.1073/pnas.94.10.5137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Laybutt D.R., et al. Overexpression of c-Myc in beta-cells of transgenic mice causes proliferation and apoptosis, downregulation of insulin gene expression, and diabetes. Diabetes. 2002;51:1793–1804. doi: 10.2337/diabetes.51.6.1793. [DOI] [PubMed] [Google Scholar]
- 21.Miyaura C., et al. Expression of reg/PSP, a pancreatic exocrine gene: relationship to changes in islet beta-cell mass. Mol. Endocrinol. 1991;5:226–234. doi: 10.1210/mend-5-2-226. [DOI] [PubMed] [Google Scholar]