Abstract
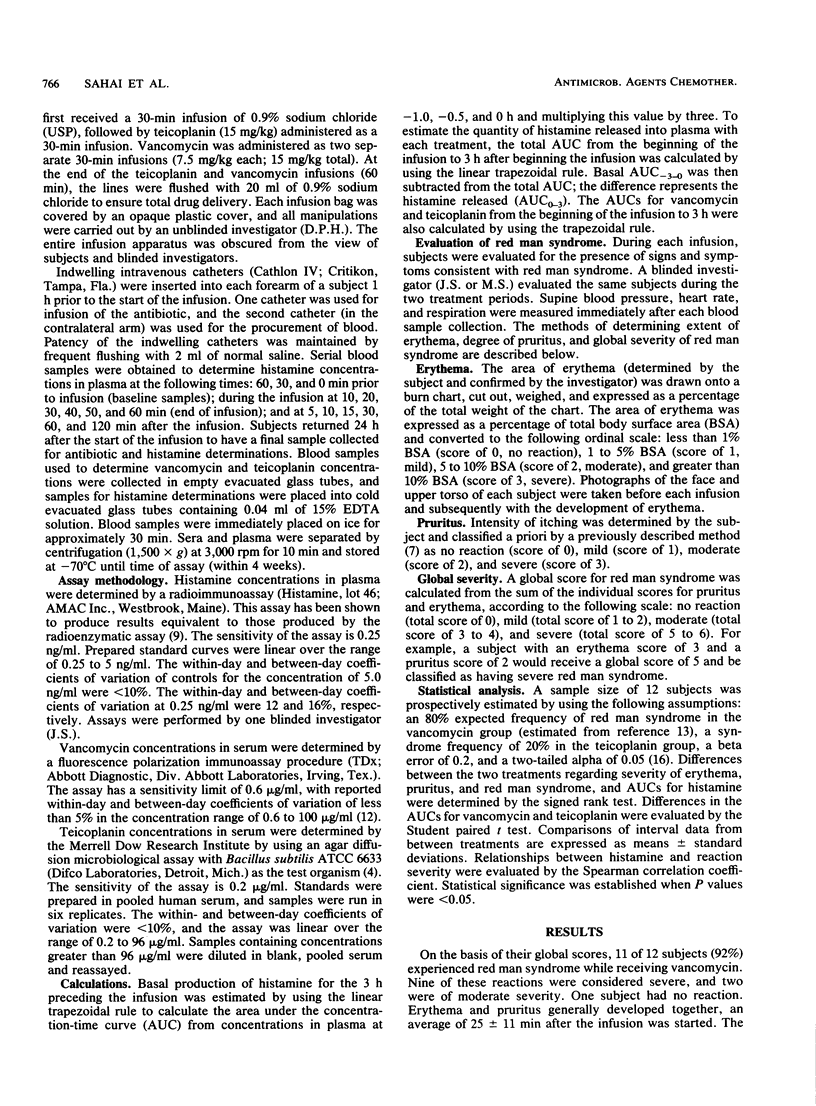
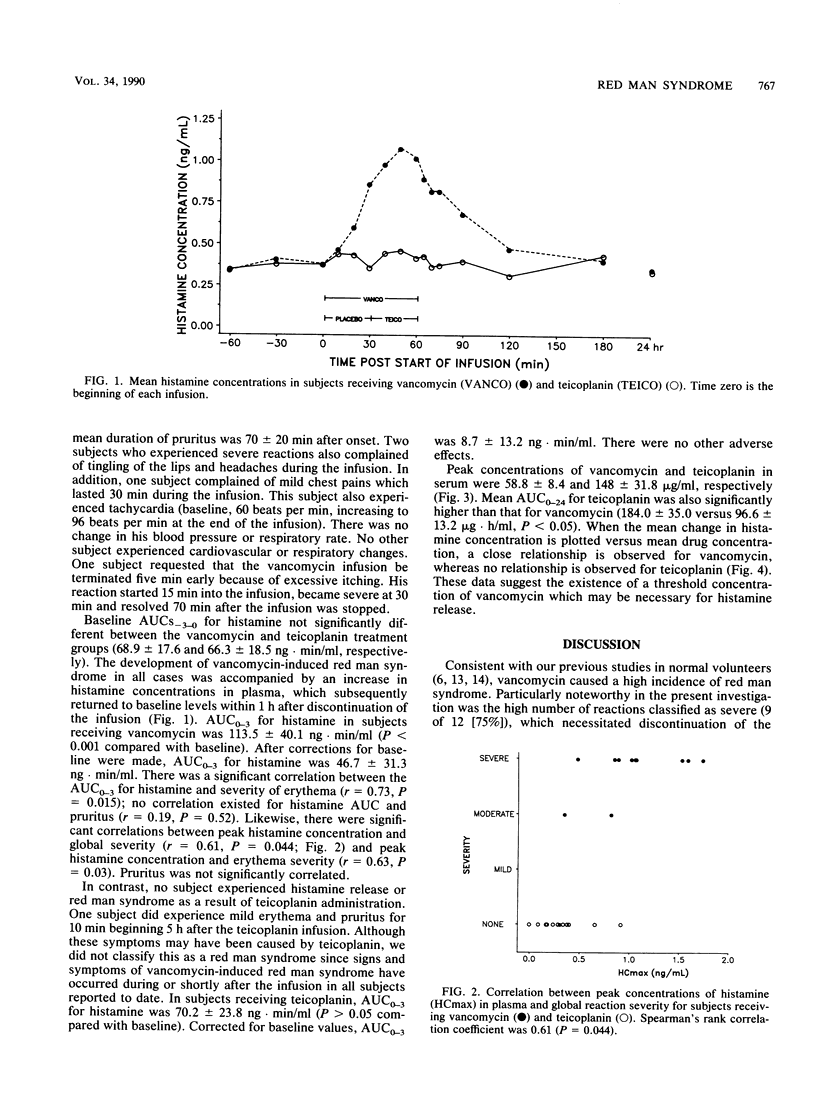
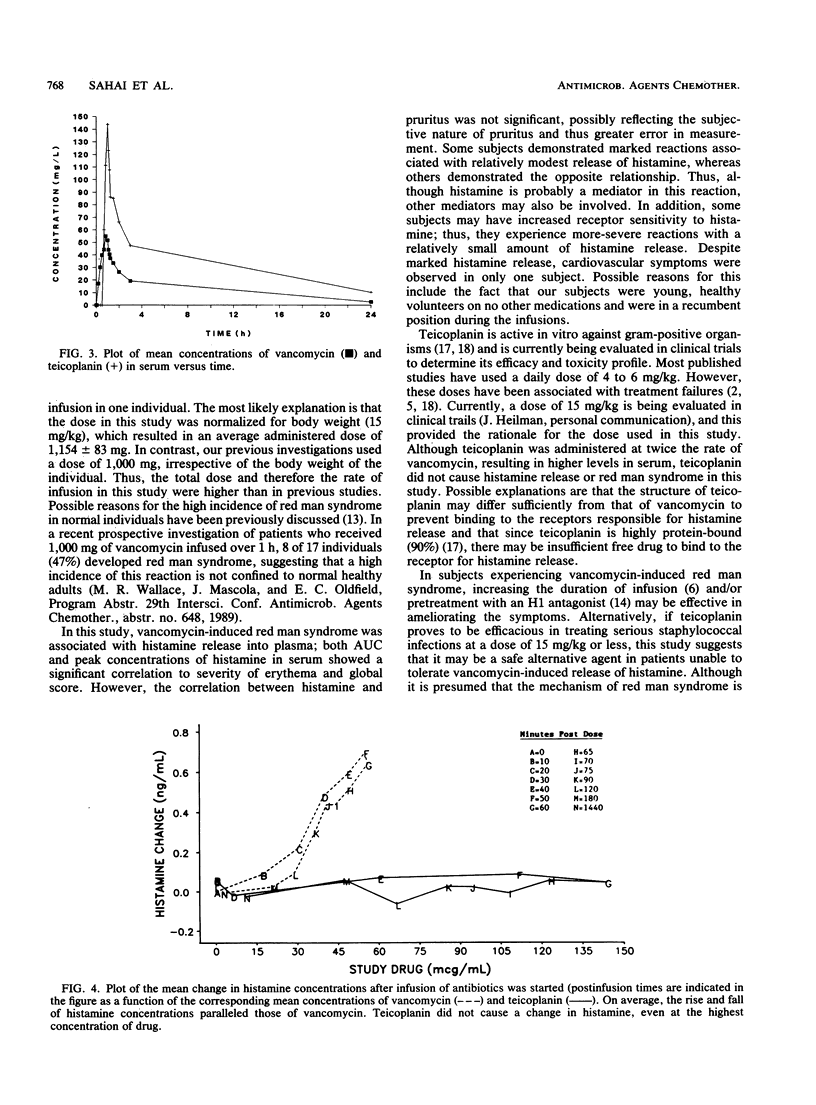
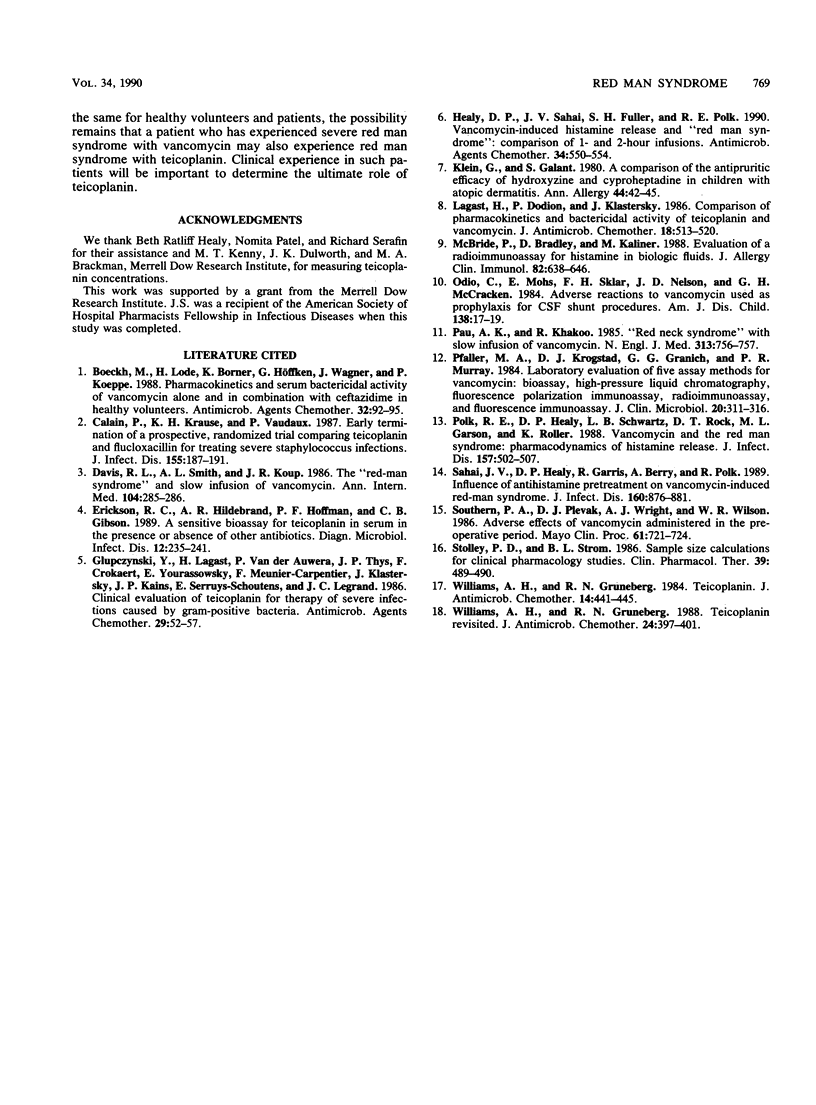
Twelve healthy adult males participated in a double-blind, randomized, two-way crossover study to determine histamine release and the frequency and severity of "red man syndrome" (RMS) following intravenous administration of vancomycin (15 mg/kg of body weight over 60 min) and teicoplanin (15 mg/kg over 30 min). Concentrations of vancomycin and teicoplanin in serum and concentrations of histamine in plasma were measured at baseline and during and after each infusion. Erythema and pruritus were classified a priori as mild, moderate, or severe. The extent of erythema was determined by the use of a burn chart, and pruritus was assessed by the subject with a rank scale. Global severity of RMS was determined by summation of the individual scores for pruritus and erythema. Baseline areas under the concentration-time curve for histamine were not significantly different for the vancomycin and teicoplanin treatments. Vancomycin caused RMS in 11 of 12 subjects (9 severe and 2 moderate cases) and was associated with a significant increase in plasma histamine (46.7 +/- 31.3 ng.min/ml, P less than 0.05). In contrast, teicoplanin did not cause RMS or elicit significant histamine release (8.7 +/- 13.2 ng.min/ml). Peak concentrations of vancomycin and teicoplanin in serum were 58.8 +/- 8.4 and 148.0 +/- 31.8 micrograms/ml, respectively (P less than 0.05). Assuming equal efficacy, these data suggest that teicoplanin may be a safe alternative agent in subjects experiencing severe RMS due to vancomycin; however, further studies in the clinical setting are needed.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Boeckh M., Lode H., Borner K., Höffken G., Wagner J., Koeppe P. Pharmacokinetics and serum bactericidal activity of vancomycin alone and in combination with ceftazidime in healthy volunteers. Antimicrob Agents Chemother. 1988 Jan;32(1):92–95. doi: 10.1128/aac.32.1.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calain P., Krause K. H., Vaudaux P., Auckenthaler R., Lew D., Waldvogel F., Hirschel B. Early termination of a prospective, randomized trial comparing teicoplanin and flucloxacillin for treating severe staphylococcal infections. J Infect Dis. 1987 Feb;155(2):187–191. doi: 10.1093/infdis/155.2.187. [DOI] [PubMed] [Google Scholar]
- Davis R. L., Smith A. L., Koup J. R. The "red man's syndrome" and slow infusion of vancomycin. Ann Intern Med. 1986 Feb;104(2):285–286. doi: 10.7326/0003-4819-104-2-285_2. [DOI] [PubMed] [Google Scholar]
- Erickson R. C., Hildebrand A. R., Hoffman P. F., Gibson C. B. A sensitive bioassay for teicoplanin in serum in the presence or absence of other antibiotics. Diagn Microbiol Infect Dis. 1989 May-Jun;12(3):235–241. doi: 10.1016/0732-8893(89)90020-5. [DOI] [PubMed] [Google Scholar]
- Glupczynski Y., Lagast H., Van der Auwera P., Thys J. P., Crokaert F., Yourassowsky E., Meunier-Carpentier F., Klastersky J., Kains J. P., Serruys-Schoutens E. Clinical evaluation of teicoplanin for therapy of severe infections caused by gram-positive bacteria. Antimicrob Agents Chemother. 1986 Jan;29(1):52–57. doi: 10.1128/aac.29.1.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Healy D. P., Sahai J. V., Fuller S. H., Polk R. E. Vancomycin-induced histamine release and "red man syndrome": comparison of 1- and 2-hour infusions. Antimicrob Agents Chemother. 1990 Apr;34(4):550–554. doi: 10.1128/aac.34.4.550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lagast H., Dodion P., Klastersky J. Comparison of pharmacokinetics and bactericidal activity of teicoplanin and vancomycin. J Antimicrob Chemother. 1986 Oct;18(4):513–520. doi: 10.1093/jac/18.4.513. [DOI] [PubMed] [Google Scholar]
- McBride P., Bradley D., Kaliner M. Evaluation of a radioimmunoassay for histamine measurement in biologic fluids. J Allergy Clin Immunol. 1988 Oct;82(4):638–646. doi: 10.1016/0091-6749(88)90977-3. [DOI] [PubMed] [Google Scholar]
- Odio C., Mohs E., Sklar F. H., Nelson J. D., McCracken G. H., Jr Adverse reactions to vancomycin used as prophylaxis for CSF shunt procedures. Am J Dis Child. 1984 Jan;138(1):17–19. doi: 10.1001/archpedi.1984.02140390009004. [DOI] [PubMed] [Google Scholar]
- Pau A. K., Khakoo R. "Red-neck syndrome" with slow infusion of vancomycin. N Engl J Med. 1985 Sep 19;313(12):756–757. doi: 10.1056/NEJM198509193131214. [DOI] [PubMed] [Google Scholar]
- Pfaller M. A., Krogstad D. J., Granich G. G., Murray P. R. Laboratory evaluation of five assay methods for vancomycin: bioassay, high-pressure liquid chromatography, fluorescence polarization immunoassay, radioimmunoassay, and fluorescence immunoassay. J Clin Microbiol. 1984 Sep;20(3):311–316. doi: 10.1128/jcm.20.3.311-316.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polk R. E., Healy D. P., Schwartz L. B., Rock D. T., Garson M. L., Roller K. Vancomycin and the red-man syndrome: pharmacodynamics of histamine release. J Infect Dis. 1988 Mar;157(3):502–507. doi: 10.1093/infdis/157.3.502. [DOI] [PubMed] [Google Scholar]
- Sahai J., Healy D. P., Garris R., Berry A., Polk R. E. Influence of antihistamine pretreatment on vancomycin-induced red-man syndrome. J Infect Dis. 1989 Nov;160(5):876–881. doi: 10.1093/infdis/160.5.876. [DOI] [PubMed] [Google Scholar]
- Southorn P. A., Plevak D. J., Wright A. J., Wilson W. R. Adverse effects of vancomycin administered in the perioperative period. Mayo Clin Proc. 1986 Sep;61(9):721–724. doi: 10.1016/s0025-6196(12)62773-6. [DOI] [PubMed] [Google Scholar]
- Stolley P. D., Strom B. L. Sample size calculations for clinical pharmacology studies. Clin Pharmacol Ther. 1986 May;39(5):489–490. doi: 10.1038/clpt.1986.85. [DOI] [PubMed] [Google Scholar]
- Williams A. H., Grüneberg R. N. Teicoplanin revisited. J Antimicrob Chemother. 1988 Oct;22(4):397–401. doi: 10.1093/jac/22.4.397. [DOI] [PubMed] [Google Scholar]
- Williams A. H., Grüneberg R. N. Teicoplanin. J Antimicrob Chemother. 1984 Nov;14(5):441–445. [PubMed] [Google Scholar]


