Abstract
Background: The previous epidemiological study of paediatric nephrolithiasis in Britain was conducted more than 30 years ago.
Aims: To examine the presenting features, predisposing factors, and treatment strategies used in paediatric stones presenting to a British centre over the past five years.
Methods: A total of 121 children presented with a urinary tract renal stone, to one adult and one paediatric centre, over a five year period (1997–2001). All children were reviewed in a dedicated stone clinic and had a full infective and metabolic stone investigative work up. Treatment was assessed by retrospective hospital note review.
Results: A metabolic abnormality was found in 44% of children, 30% were classified as infective, and 26% idiopathic. Bilateral stones on presentation occurred in 26% of the metabolic group compared to 12% in the infective/idiopathic group (odds ratio 2.7, 95% CI 1.03 to 7.02). Coexisting urinary tract infection was common (49%) in the metabolic group. Surgically, minimally invasive techniques (lithotripsy, percutaneous nephrolithotomy, and endoscopy) were used in 68% of patients.
Conclusions: There has been a shift in the epidemiology of paediatric renal stone disease in the UK over the past 30 years. Underlying metabolic causes are now the most common but can be masked by coexisting urinary tract infection. Treatment has progressed, especially surgically, with sophisticated minimally invasive techniques now employed. All children with renal stones should have a metabolic screen.
Full Text
The Full Text of this article is available as a PDF (156.0 KB).
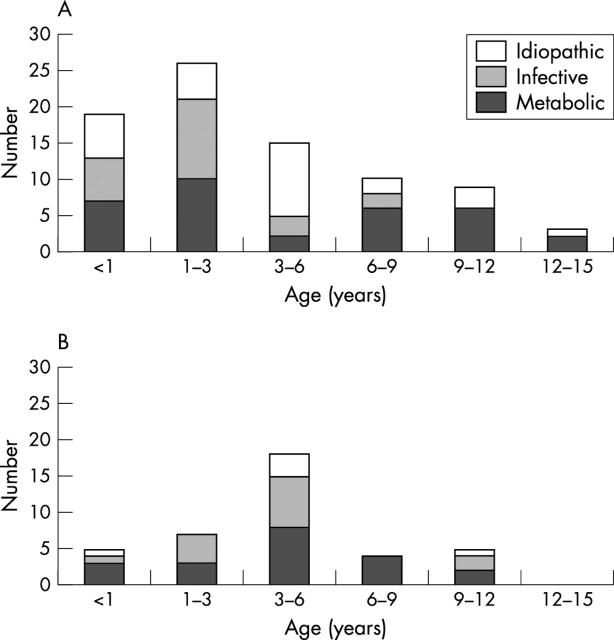
Figure 1 .
Age at presentation, sex distribution, and aetiological type of paediatric stones presenting to Great Ormond Street and the Middlesex hospital 1997–2001. (A) Males (n = 82). (B) Females (n = 39).
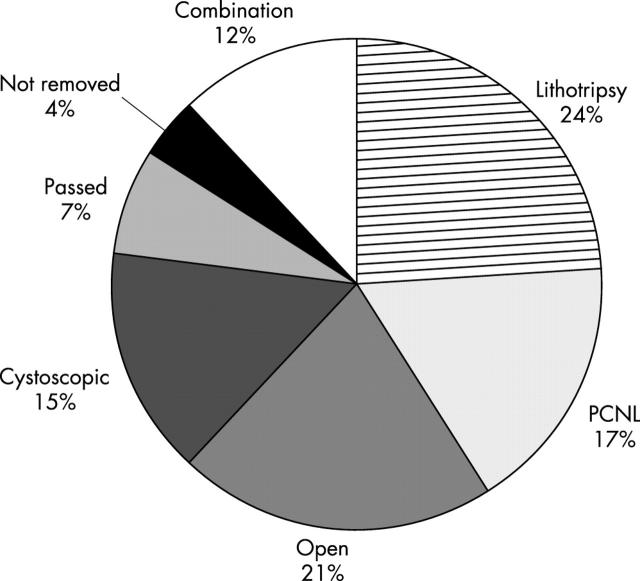
Figure 2 .
Surgical modalities of stone removal (n = 121).
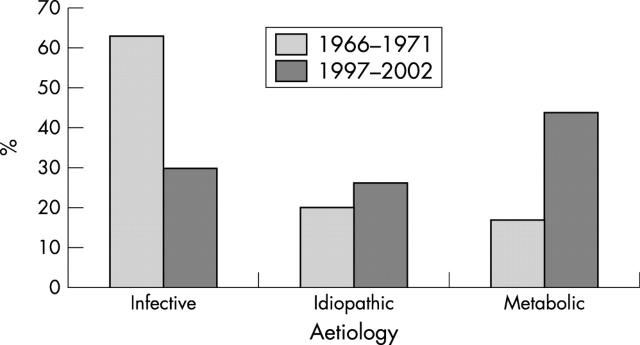
Figure 3 .
Underlying stone aetiologies. Comparison between previous study (1966–71) and present study (1997–2002).
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Ahmad Tariq, Armuzzi Alessandro, Bunce Mike, Mulcahy-Hawes Kim, Marshall Sara E., Orchard Timothy R., Crawshaw Jonathan, Large Oliver, de Silva Arjuna, Cook Julia T. The molecular classification of the clinical manifestations of Crohn's disease. Gastroenterology. 2002 Apr;122(4):854–866. doi: 10.1053/gast.2002.32413. [DOI] [PubMed] [Google Scholar]
- Androulakakis P. A., Barratt T. M., Ransley P. G., Williams D. I. Urinary calculi in children. A 5 to 15-year follow-up with particular reference to recurrent and residual stones. Br J Urol. 1982 Apr;54(2):176–180. doi: 10.1111/j.1464-410x.1982.tb13544.x. [DOI] [PubMed] [Google Scholar]
- Armitage E., Drummond H., Ghosh S., Ferguson A. Incidence of juvenile-onset Crohn's disease in Scotland. Lancet. 1999 May 1;353(9163):1496–1497. doi: 10.1016/S0140-6736(99)00333-5. [DOI] [PubMed] [Google Scholar]
- Ballinger A. B., Camacho-Hübner C., Croft N. M. Growth failure and intestinal inflammation. QJM. 2001 Mar;94(3):121–125. doi: 10.1093/qjmed/94.3.121. [DOI] [PubMed] [Google Scholar]
- Barratt T. M., Kasidas G. P., Murdoch I., Rose G. A. Urinary oxalate and glycolate excretion and plasma oxalate concentration. Arch Dis Child. 1991 Apr;66(4):501–503. doi: 10.1136/adc.66.4.501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barton J. R., Ferguson A. Clinical features, morbidity and mortality of Scottish children with inflammatory bowel disease. Q J Med. 1990 May;75(277):423–439. [PubMed] [Google Scholar]
- Basaklar A. C., Kale N. Experience with childhood urolithiasis. Report of 196 cases. Br J Urol. 1991 Feb;67(2):203–205. doi: 10.1111/j.1464-410x.1991.tb15110.x. [DOI] [PubMed] [Google Scholar]
- Choi H., Snyder H. M., 3rd, Duckett J. W. Urolithiasis in childhood: current management. J Pediatr Surg. 1987 Feb;22(2):158–164. doi: 10.1016/s0022-3468(87)80438-4. [DOI] [PubMed] [Google Scholar]
- Choong S., Whitfield H., Duffy P., Kellett M., Cuckow P., Van't Hoff W., Corry D. The management of paediatric urolithiasis. BJU Int. 2000 Nov;86(7):857–860. doi: 10.1046/j.1464-410x.2000.00909.x. [DOI] [PubMed] [Google Scholar]
- Diamond D. A., Rickwood A. M., Lee P. H., Johnston J. H. Infection stones in children: a twenty-seven-year review. Urology. 1994 Apr;43(4):525–527. doi: 10.1016/0090-4295(94)90247-x. [DOI] [PubMed] [Google Scholar]
- Freeman J. V., Cole T. J., Chinn S., Jones P. R., White E. M., Preece M. A. Cross sectional stature and weight reference curves for the UK, 1990. Arch Dis Child. 1995 Jul;73(1):17–24. doi: 10.1136/adc.73.1.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gearhart J. P., Herzberg G. Z., Jeffs R. D. Childhood urolithiasis: experiences and advances. Pediatrics. 1991 Apr;87(4):445–450. [PubMed] [Google Scholar]
- Ghazali S., Barratt T. M., Williams D. I. Childhood urolithiasis in Britain. Arch Dis Child. 1973 Apr;48(4):291–295. doi: 10.1136/adc.48.4.291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordon G. S., Wallace S. J., Neal J. W. Intracranial tumours during the first two years of life: presenting features. Arch Dis Child. 1995 Oct;73(4):345–347. doi: 10.1136/adc.73.4.345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hildebrand H., Karlberg J., Kristiansson B. Longitudinal growth in children and adolescents with inflammatory bowel disease. J Pediatr Gastroenterol Nutr. 1994 Feb;18(2):165–173. doi: 10.1097/00005176-199402000-00008. [DOI] [PubMed] [Google Scholar]
- Hugot J. P., Chamaillard M., Zouali H., Lesage S., Cézard J. P., Belaiche J., Almer S., Tysk C., O'Morain C. A., Gassull M. Association of NOD2 leucine-rich repeat variants with susceptibility to Crohn's disease. Nature. 2001 May 31;411(6837):599–603. doi: 10.1038/35079107. [DOI] [PubMed] [Google Scholar]
- Kasidas G. P. Plasma and urine measurements for monitoring of treatment in the primary hyperoxaluric patient. Nephrol Dial Transplant. 1995;10 (Suppl 8):8–10. doi: 10.1093/ndt/10.supp8.8. [DOI] [PubMed] [Google Scholar]
- Kroovand R. L. Pediatric urolithiasis. Urol Clin North Am. 1997 Feb;24(1):173–184. doi: 10.1016/s0094-0143(05)70362-1. [DOI] [PubMed] [Google Scholar]
- Kruse K., Kracht U., Kruse U. Reference values for urinary calcium excretion and screening for hypercalciuria in children and adolescents. Eur J Pediatr. 1984 Nov;143(1):25–31. doi: 10.1007/BF00442743. [DOI] [PubMed] [Google Scholar]
- Lenaerts C., Roy C. C., Vaillancourt M., Weber A. M., Morin C. L., Seidman E. High incidence of upper gastrointestinal tract involvement in children with Crohn disease. Pediatrics. 1989 May;83(5):777–781. [PubMed] [Google Scholar]
- Michener W. M., Farmer R. G., Mortimer E. A. Long-term prognosis of ulcerative colitis with onset in childhood or adolescence. J Clin Gastroenterol. 1979 Dec;1(4):301–305. doi: 10.1097/00004836-197912000-00004. [DOI] [PubMed] [Google Scholar]
- Milliner D. S. Cystinuria. Endocrinol Metab Clin North Am. 1990 Dec;19(4):889–907. [PubMed] [Google Scholar]
- Milliner D. S., Murphy M. E. Urolithiasis in pediatric patients. Mayo Clin Proc. 1993 Mar;68(3):241–248. doi: 10.1016/s0025-6196(12)60043-3. [DOI] [PubMed] [Google Scholar]
- Nijman R. J., Ackaert K., Scholtmeijer R. J., Lock T. W., Schröder F. H. Long-term results of extracorporeal shock wave lithotripsy in children. J Urol. 1989 Aug;142(2 Pt 2):609–619. doi: 10.1016/s0022-5347(17)38831-6. [DOI] [PubMed] [Google Scholar]
- O'Donoghue D. P., Dawson A. M. Crohn's disease in childhood. Arch Dis Child. 1977 Aug;52(8):627–632. doi: 10.1136/adc.52.8.627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogura Y., Bonen D. K., Inohara N., Nicolae D. L., Chen F. F., Ramos R., Britton H., Moran T., Karaliuskas R., Duerr R. H. A frameshift mutation in NOD2 associated with susceptibility to Crohn's disease. Nature. 2001 May 31;411(6837):603–606. doi: 10.1038/35079114. [DOI] [PubMed] [Google Scholar]
- Pietrow Paul K., Pope John C., 4th, Adams Mark C., Shyr Yu, Brock John W., 3rd Clinical outcome of pediatric stone disease. J Urol. 2002 Feb;167(2 Pt 1):670–673. doi: 10.1016/S0022-5347(01)69121-3. [DOI] [PubMed] [Google Scholar]
- Polinsky M. S., Kaiser B. A., Baluarte H. J., Gruskin A. B. Renal stones and hypercalciuria. Adv Pediatr. 1993;40:353–384. [PubMed] [Google Scholar]
- Puntis J., McNeish A. S., Allan R. N. Long term prognosis of Crohn's disease with onset in childhood and adolescence. Gut. 1984 Apr;25(4):329–336. doi: 10.1136/gut.25.4.329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodríguez-Soriano J., Vallo A., García-Fuentes M. Hypomagnesaemia of hereditary renal origin. Pediatr Nephrol. 1987 Jul;1(3):465–472. doi: 10.1007/BF00849255. [DOI] [PubMed] [Google Scholar]
- Roos-Hesselink J. W., Schölzel B. E., Heijdra R. J., Spitaels S. E. C., Meijboom F. J., Boersma E., Bogers A. J. J. C., Simoons M. L. Aortic valve and aortic arch pathology after coarctation repair. Heart. 2003 Sep;89(9):1074–1077. doi: 10.1136/heart.89.9.1074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubin G. P., Hungin A. P., Kelly P. J., Ling J. Inflammatory bowel disease: epidemiology and management in an English general practice population. Aliment Pharmacol Ther. 2000 Dec;14(12):1553–1559. doi: 10.1046/j.1365-2036.2000.00886.x. [DOI] [PubMed] [Google Scholar]
- Sarkissian A., Babloyan A., Arikyants N., Hesse A., Blau N., Leumann E. Pediatric urolithiasis in Armenia: a study of 198 patients observed from 1991 to 1999. Pediatr Nephrol. 2001 Sep;16(9):728–732. doi: 10.1007/s004670100647. [DOI] [PubMed] [Google Scholar]
- Sawczenko A., Lynn R., Sandhu B. K. Variations in initial assessment and management of inflammatory bowel disease across Great Britain and Ireland. Arch Dis Child. 2003 Nov;88(11):990–994. doi: 10.1136/adc.88.11.990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sawczenko A., Sandhu B. K., Logan R. F., Jenkins H., Taylor C. J., Mian S., Lynn R. Prospective survey of childhood inflammatory bowel disease in the British Isles. Lancet. 2001 Apr 7;357(9262):1093–1094. doi: 10.1016/s0140-6736(00)04309-9. [DOI] [PubMed] [Google Scholar]
- So N. P., Osorio A. V., Simon S. D., Alon U. S. Normal urinary calcium/creatinine ratios in African-American and Caucasian children. Pediatr Nephrol. 2001 Feb;16(2):133–139. doi: 10.1007/s004670000510. [DOI] [PubMed] [Google Scholar]
- Spray C., Debelle G. D., Murphy M. S. Current diagnosis, management and morbidity in paediatric inflammatory bowel disease. Acta Paediatr. 2001 Apr;90(4):400–405. [PubMed] [Google Scholar]
- Stapleton F. B. Clinical approach to children with urolithiasis. Semin Nephrol. 1996 Sep;16(5):389–397. [PubMed] [Google Scholar]
- Stapleton F. B., Linshaw M. A., Hassanein K., Gruskin A. B. Uric acid excretion in normal children. J Pediatr. 1978 Jun;92(6):911–914. doi: 10.1016/s0022-3476(78)80359-x. [DOI] [PubMed] [Google Scholar]
- Stapleton F. B., McKay C. P., Noe H. N. Urolithiasis in children: the role of hypercalciuria. Pediatr Ann. 1987 Dec;16(12):980-1,984-92. doi: 10.3928/0090-4481-19871201-09. [DOI] [PubMed] [Google Scholar]
- Vandeursen H., Devos P., Baert L. Electromagnetic extracorporeal shock wave lithotripsy in children. J Urol. 1991 Jun;145(6):1229–1231. doi: 10.1016/s0022-5347(17)38583-x. [DOI] [PubMed] [Google Scholar]
- el-Damanhoury H., Bürger R., Hohenfellner R. Surgical aspects of urolithiasis in children. Pediatr Nephrol. 1991 May;5(3):339–347. doi: 10.1007/BF00867499. [DOI] [PubMed] [Google Scholar]