Abstract
Background: There are no published data from Great Britain and Ireland detailing the initial management of children with inflammatory bowel disease (IBD).
Aims: To prospectively record the initial investigation and treatment of children aged less than 16 years with newly diagnosed IBD.
Methods: For 13 months, between June 1998 and June 1999, 3247 paediatricians, adult gastroenterologists, and surgeons across the UK and Ireland were prospectively surveyed each month and asked to report every newly diagnosed case of childhood IBD. Reporters subsequently completed a postal questionnaire about each case.
Results: A total of 739 new IBD cases were reported from 172 institutions. Significant variations were observed in the investigation and treatment of these cases, when examined by number of cases reported per institution, or by the specialists providing care. There were wide regional variations in the proportion of children having access to paediatric gastroenterology services. Overall, one third of children received care from an adult service, and a tenth care exclusively from an adult gastroenterologist. Children with Crohn's disease who had some or all of their care from adult services were more likely to receive systemic steroids and less likely to receive dietary therapy; those with ulcerative colitis were more likely to receive rectal steroids and to have surgery. Height and weight were also less likely to be recorded in those whose care involved adult services.
Conclusion: Current specialist provision, and initial investigation and treatment of IBD, is heterogeneous. Optimisation of care is likely to be achieved by greater access to specialist paediatric gastroenterology services for all those with suspected IBD.
Full Text
The Full Text of this article is available as a PDF (237.4 KB).
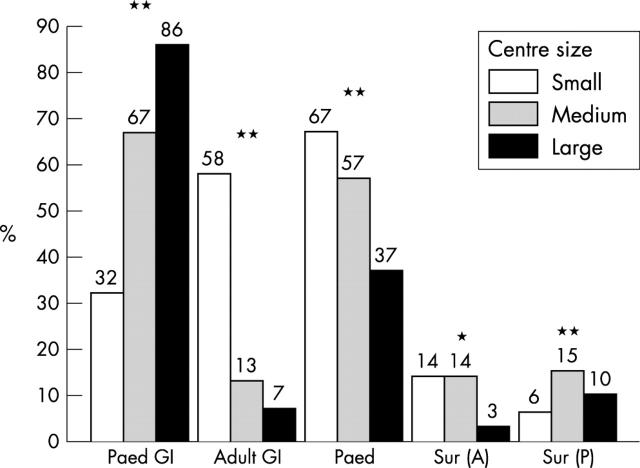
Figure 1 .
Treatment of Crohn's disease by reporting centre size.
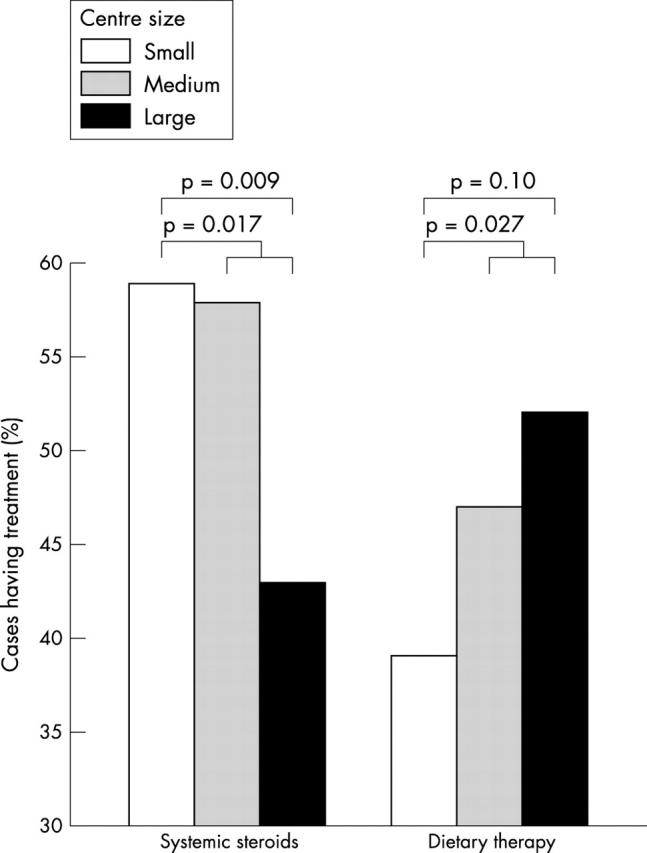
Figure 2 .
Specialist involvement by centre size. GI, gastroenterologist; Sur (A), adult surgeon; Sur (P), paediatric surgeon. *p < 0.05, **p < 0.001, χ2 test.
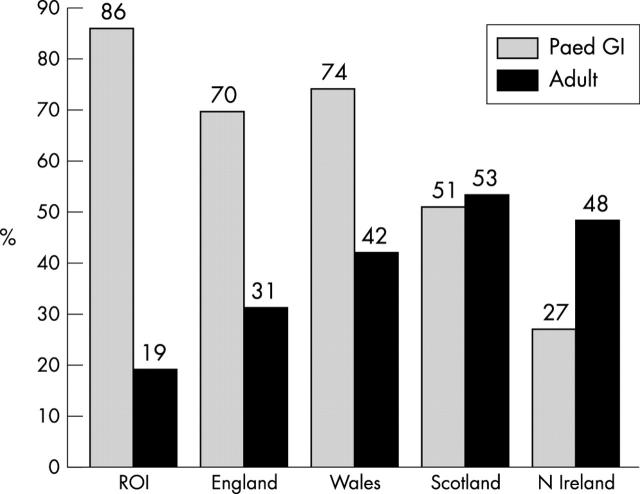
Figure 3 .
Selected specialist involvement by country. Paed GI, paediatric gastroenterologist; adult, adult gastroenterologist and/or adult surgeon; ROI, Republic of Ireland. Variations between countries for Paed GI and Adult, both p < 0.001, χ2 test.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Armitage E., Drummond H., Ghosh S., Ferguson A. Incidence of juvenile-onset Crohn's disease in Scotland. Lancet. 1999 May 1;353(9163):1496–1497. doi: 10.1016/S0140-6736(99)00333-5. [DOI] [PubMed] [Google Scholar]
- Arul G. S., Spicer R. D. Where should paediatric surgery be performed? Arch Dis Child. 1998 Jul;79(1):65–72. doi: 10.1136/adc.79.1.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barton J. R., Ferguson A. Clinical features, morbidity and mortality of Scottish children with inflammatory bowel disease. Q J Med. 1990 May;75(277):423–439. [PubMed] [Google Scholar]
- Barton J. R., Gillon S., Ferguson A. Incidence of inflammatory bowel disease in Scottish children between 1968 and 1983; marginal fall in ulcerative colitis, three-fold rise in Crohn's disease. Gut. 1989 May;30(5):618–622. doi: 10.1136/gut.30.5.618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baumer J. H., Hunt L. P., Shield J. P. Audit of diabetes care by caseload. Arch Dis Child. 1997 Aug;77(2):102–108. doi: 10.1136/adc.77.2.102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cosgrove M., Al-Atia R. F., Jenkins H. R. The epidemiology of paediatric inflammatory bowel disease. Arch Dis Child. 1996 May;74(5):460–461. doi: 10.1136/adc.74.5.460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engström I., Lindquist B. L. Inflammatory bowel disease in children and adolescents: a somatic and psychiatric investigation. Acta Paediatr Scand. 1991 Jun-Jul;80(6-7):640–647. doi: 10.1111/j.1651-2227.1991.tb11923.x. [DOI] [PubMed] [Google Scholar]
- Field D., Hodges S., Mason E., Burton P. Survival and place of treatment after premature delivery. Arch Dis Child. 1991 Apr;66(4 Spec No):408–411. doi: 10.1136/adc.66.4_spec_no.408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghosh S., Drummond H. E., Ferguson A. Neglect of growth and development in the clinical monitoring of children and teenagers with inflammatory bowel disease: review of case records. BMJ. 1998 Jul 11;317(7151):120–121. doi: 10.1136/bmj.317.7151.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffiths A. M., Nguyen P., Smith C., MacMillan J. H., Sherman P. M. Growth and clinical course of children with Crohn's disease. Gut. 1993 Jul;34(7):939–943. doi: 10.1136/gut.34.7.939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall S. M., Nicoll A. The British Paediatric Surveillance Unit--a pioneering method for investigating the less common disorders of childhood. Report of a seminar held in June 1995. Child Care Health Dev. 1998 Mar;24(2):129–143. doi: 10.1046/j.1365-2214.1998.00052.x. [DOI] [PubMed] [Google Scholar]
- Heuschkel R. B., Menache C. C., Megerian J. T., Baird A. E. Enteral nutrition and corticosteroids in the treatment of acute Crohn's disease in children. J Pediatr Gastroenterol Nutr. 2000 Jul;31(1):8–15. doi: 10.1097/00005176-200007000-00005. [DOI] [PubMed] [Google Scholar]
- Hildebrand H., Karlberg J., Kristiansson B. Longitudinal growth in children and adolescents with inflammatory bowel disease. J Pediatr Gastroenterol Nutr. 1994 Feb;18(2):165–173. doi: 10.1097/00005176-199402000-00008. [DOI] [PubMed] [Google Scholar]
- Holmquist L., Rudic N., Ahren C., Fällström S. P. The diagnostic value of colonoscopy compared with rectosigmoidoscopy in children and adolescents with symptoms of chronic inflammatory bowel disease of the colon. Scand J Gastroenterol. 1988 Jun;23(5):577–584. doi: 10.3109/00365528809093915. [DOI] [PubMed] [Google Scholar]
- Kirschner B. S. Differences in the management of inflammatory bowel disease in children and adolescents compared to adults. Neth J Med. 1998 Dec;53(6):S13–S18. doi: 10.1016/s0300-2977(98)00118-1. [DOI] [PubMed] [Google Scholar]
- Macfarlane B., Leicester R., Romaya C., Epstein O. Colonoscopy services in the United Kingdom. Endoscopy. 1999 Aug;31(6):409–411. doi: 10.1055/s-1999-8040. [DOI] [PubMed] [Google Scholar]
- Mahadeva R., Webb K., Westerbeek R. C., Carroll N. R., Dodd M. E., Bilton D., Lomas D. A. Clinical outcome in relation to care in centres specialising in cystic fibrosis: cross sectional study. BMJ. 1998 Jun 13;316(7147):1771–1775. doi: 10.1136/bmj.316.7147.1771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKiernan P. J., Baker A. J., Kelly D. A. The frequency and outcome of biliary atresia in the UK and Ireland. Lancet. 2000 Jan 1;355(9197):25–29. doi: 10.1016/S0140-6736(99)03492-3. [DOI] [PubMed] [Google Scholar]
- Pearson G., Shann F., Barry P., Vyas J., Thomas D., Powell C., Field D. Should paediatric intensive care be centralised? Trent versus Victoria. Lancet. 1997 Apr 26;349(9060):1213–1217. doi: 10.1016/S0140-6736(96)12396-5. [DOI] [PubMed] [Google Scholar]
- Puntis J., McNeish A. S., Allan R. N. Long term prognosis of Crohn's disease with onset in childhood and adolescence. Gut. 1984 Apr;25(4):329–336. doi: 10.1136/gut.25.4.329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanderson I. R., Udeen S., Davies P. S., Savage M. O., Walker-Smith J. A. Remission induced by an elemental diet in small bowel Crohn's disease. Arch Dis Child. 1987 Feb;62(2):123–127. doi: 10.1136/adc.62.2.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sawczenko A., Sandhu B. K., Logan R. F., Jenkins H., Taylor C. J., Mian S., Lynn R. Prospective survey of childhood inflammatory bowel disease in the British Isles. Lancet. 2001 Apr 7;357(9262):1093–1094. doi: 10.1016/s0140-6736(00)04309-9. [DOI] [PubMed] [Google Scholar]
- Sharples A., O'Neill M., Dearlove O. Impact of specialised paediatric retrieval teams. Children are still transferred by non-specialist teams. BMJ. 1996 Jan 13;312(7023):120–121. doi: 10.1136/bmj.312.7023.120c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spray C., Debelle G. D., Murphy M. S. Current diagnosis, management and morbidity in paediatric inflammatory bowel disease. Acta Paediatr. 2001 Apr;90(4):400–405. [PubMed] [Google Scholar]