Abstract
Aims: (1) To assess the value of cranial magnetic resonance imaging (MRI) scans in the investigation of girls with central precocious puberty (CPP); and (2) to determine the clinical predictors of abnormal cranial MRI scans in these patients.
Methods: A retrospective study of 67 girls diagnosed with CPP who underwent cranial MRI scans at diagnosis. Patients with neurological signs or symptoms at presentation were excluded.
Results: The mean age of onset of puberty was 6.2 years (range 2.0–7.9). Intracranial abnormalities were present in 10 (15%) patients (MR+), while 57 (85%) had no abnormalities (MR-). There was no statistical difference between MR+ patients and MR- patients at presentation with respect to age of onset of puberty, pubertal stage, bone age advance, pelvic ultrasound findings, or height or body mass index standard deviation scores (SDS).
Conclusion: Girls with CPP should have a cranial MRI scan as part of their assessment since clinical features, including age, are not helpful in predicting those with underlying pathology. Implementation of such an approach may have a substantial effect on clinical practice and healthcare cost.
Full Text
The Full Text of this article is available as a PDF (142.0 KB).
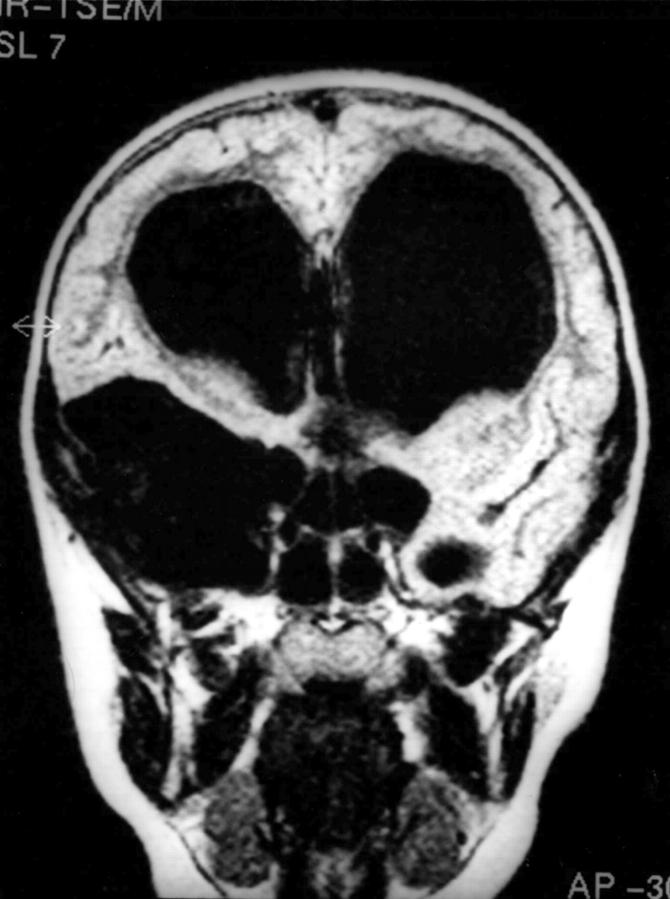
Figure 1.
Large arachnoid cyst.
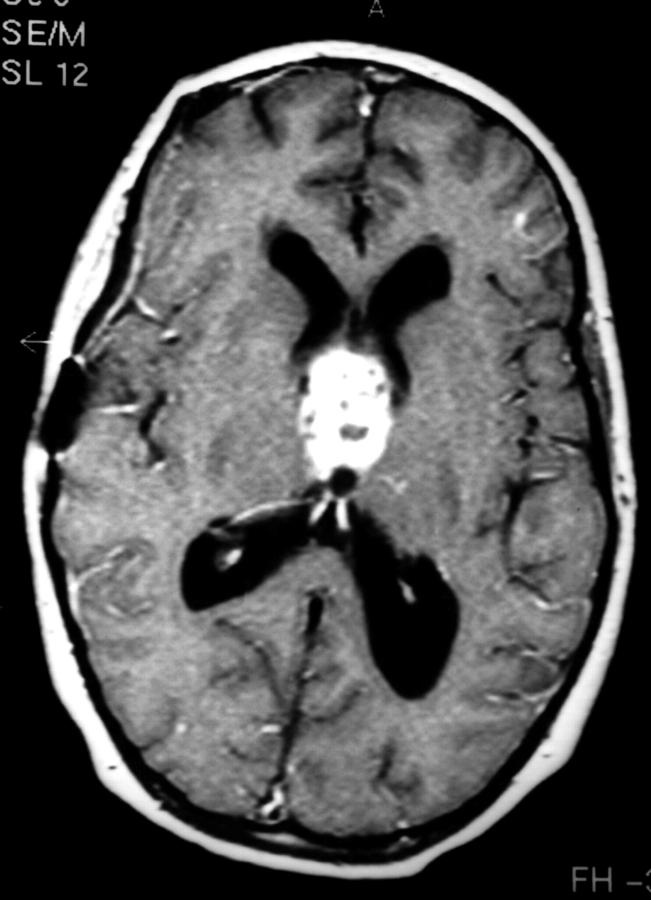
Figure 2.
Hypothalamic pilocytic astrocytoma.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Brauner R., Malandry F., Rappaport R., Zucker J. M., Kalifa C., Pierre-Kahn A., Bataini P., Dufier J. L. Growth and endocrine disorders in optic glioma. Eur J Pediatr. 1990 Sep;149(12):825–828. doi: 10.1007/BF02072067. [DOI] [PubMed] [Google Scholar]
- Bridges N. A., Christopher J. A., Hindmarsh P. C., Brook C. G. Sexual precocity: sex incidence and aetiology. Arch Dis Child. 1994 Feb;70(2):116–118. doi: 10.1136/adc.70.2.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacciari E., Fréjaville E., Cicognani A., Pirazzoli P., Frank G., Balsamo A., Tassinari D., Zappulla F., Bergamaschi R., Cristi G. F. How many cases of true precocious puberty in girls are idiopathic? J Pediatr. 1983 Mar;102(3):357–360. doi: 10.1016/s0022-3476(83)80648-9. [DOI] [PubMed] [Google Scholar]
- Cacciari E., Zucchini S., Carlà G., Pirazzoli P., Cicognani A., Mandini M., Busacca M., Trevisan C. Endocrine function and morphological findings in patients with disorders of the hypothalamo-pituitary area: a study with magnetic resonance. Arch Dis Child. 1990 Nov;65(11):1199–1202. doi: 10.1136/adc.65.11.1199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaussain J. L., Couprie C., Lacaille F., Simon D., Job J. C. Growth and precocious puberty. Acta Paediatr Scand Suppl. 1988;347:38–43. [PubMed] [Google Scholar]
- Chemaitilly W., Trivin C., Adan L., Gall V., Sainte-Rose C., Brauner R. Central precocious puberty: clinical and laboratory features. Clin Endocrinol (Oxf) 2001 Mar;54(3):289–294. doi: 10.1046/j.1365-2265.2001.01229.x. [DOI] [PubMed] [Google Scholar]
- Cisternino M., Arrigo T., Pasquino A. M., Tinelli C., Antoniazzi F., Beduschi L., Bindi G., Borrelli P., De Sanctis V., Farello G. Etiology and age incidence of precocious puberty in girls: a multicentric study. J Pediatr Endocrinol Metab. 2000 Jul;13 (Suppl 1):695–701. doi: 10.1515/jpem.2000.13.s1.695. [DOI] [PubMed] [Google Scholar]
- Cisternino M., Arrigo T., Pasquino A. M., Tinelli C., Antoniazzi F., Beduschi L., Bindi G., Borrelli P., De Sanctis V., Farello G. Etiology and age incidence of precocious puberty in girls: a multicentric study. J Pediatr Endocrinol Metab. 2000 Jul;13 (Suppl 1):695–701. doi: 10.1515/jpem.2000.13.s1.695. [DOI] [PubMed] [Google Scholar]
- Debeneix C., Bourgeois M., Trivin C., Sainte-Rose C., Brauner R. Hypothalamic hamartoma: comparison of clinical presentation and magnetic resonance images. Horm Res. 2001;56(1-2):12–18. doi: 10.1159/000048084. [DOI] [PubMed] [Google Scholar]
- Fontoura M., Brauner R., Prevot C., Rappaport R. Precocious puberty in girls: early diagnosis of a slowly progressing variant. Arch Dis Child. 1989 Aug;64(8):1170–1176. doi: 10.1136/adc.64.8.1170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freeman J. V., Cole T. J., Chinn S., Jones P. R., White E. M., Preece M. A. Cross sectional stature and weight reference curves for the UK, 1990. Arch Dis Child. 1995 Jul;73(1):17–24. doi: 10.1136/adc.73.1.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffin I. J., Cole T. J., Duncan K. A., Hollman A. S., Donaldson M. D. Pelvic ultrasound measurements in normal girls. Acta Paediatr. 1995 May;84(5):536–543. doi: 10.1111/j.1651-2227.1995.tb13689.x. [DOI] [PubMed] [Google Scholar]
- Gupta R., Ammini A. C. Precocious puberty with pituitary gland hyperplasia: two cases in one family. Pediatr Radiol. 1996;26(6):418–420. doi: 10.1007/BF01387318. [DOI] [PubMed] [Google Scholar]
- Hochman H. I., Judge D. M., Reichlin S. Precocious puberty and hypothalamic hamartoma. Pediatrics. 1981 Feb;67(2):236–244. [PubMed] [Google Scholar]
- Jensen A. M., Brocks V., Holm K., Laursen E. M., Müller J. Central precocious puberty in girls: internal genitalia before, during, and after treatment with long-acting gonadotropin-releasing hormone analogues. J Pediatr. 1998 Jan;132(1):105–108. doi: 10.1016/s0022-3476(98)70493-7. [DOI] [PubMed] [Google Scholar]
- Judge D. M., Kulin H. E., Page R., Santen R., Trapukdi S. Hypothalamic hamartoma: a source of luteinizing-hormone-releasing factor in precocious puberty. N Engl J Med. 1977 Jan 6;296(1):7–10. doi: 10.1056/NEJM197701062960102. [DOI] [PubMed] [Google Scholar]
- Jung H., Carmel P., Schwartz M. S., Witkin J. W., Bentele K. H., Westphal M., Piatt J. H., Costa M. E., Cornea A., Ma Y. J. Some hypothalamic hamartomas contain transforming growth factor alpha, a puberty-inducing growth factor, but not luteinizing hormone-releasing hormone neurons. J Clin Endocrinol Metab. 1999 Dec;84(12):4695–4701. doi: 10.1210/jcem.84.12.6185. [DOI] [PubMed] [Google Scholar]
- Kao S. C., Cook J. S., Hansen J. R., Simonson T. M. MR imaging of the pituitary gland in central precocious puberty. Pediatr Radiol. 1992;22(7):481–484. doi: 10.1007/BF02012988. [DOI] [PubMed] [Google Scholar]
- Kornreich L., Horev G., Blaser S., Daneman D., Kauli R., Grunebaum M. Central precocious puberty: evaluation by neuroimaging. Pediatr Radiol. 1995;25(1):7–11. doi: 10.1007/BF02020830. [DOI] [PubMed] [Google Scholar]
- Lyon A. J., De Bruyn R., Grant D. B. Isosexual precocious puberty in girls. Acta Paediatr Scand. 1985 Nov;74(6):950–955. doi: 10.1111/j.1651-2227.1985.tb10063.x. [DOI] [PubMed] [Google Scholar]
- Mahachoklertwattana P., Kaplan S. L., Grumbach M. M. The luteinizing hormone-releasing hormone-secreting hypothalamic hamartoma is a congenital malformation: natural history. J Clin Endocrinol Metab. 1993 Jul;77(1):118–124. doi: 10.1210/jcem.77.1.8325933. [DOI] [PubMed] [Google Scholar]
- Mansfield M. J., Beardsworth D. E., Loughlin J. S., Crawford J. D., Bode H. H., Rivier J., Vale W., Kushner D. C., Crigler J. F., Jr, Crowley W. F., Jr Long-term treatment of central precocious puberty with a long-acting analogue of luteinizing hormone-releasing hormone. Effects on somatic growth and skeletal maturation. N Engl J Med. 1983 Nov 24;309(21):1286–1290. doi: 10.1056/NEJM198311243092104. [DOI] [PubMed] [Google Scholar]
- Rieth K. G., Comite F., Dwyer A. J., Nelson M. J., Pescovitz O., Shawker T. H., Cutler G. B., Loriaux D. L. CT of cerebral abnormalities in precocious puberty. AJR Am J Roentgenol. 1987 Jun;148(6):1231–1238. doi: 10.2214/ajr.148.6.1231. [DOI] [PubMed] [Google Scholar]
- Robben S. G., Oostdijk W., Drop S. L., Tanghe H. L., Vielvoye G. J., Meradji M. Idiopathic isosexual central precocious puberty: magnetic resonance findings in 30 patients. Br J Radiol. 1995 Jan;68(805):34–38. doi: 10.1259/0007-1285-68-805-34. [DOI] [PubMed] [Google Scholar]
- Robben S. G., Oostdijk W., Drop S. L., Tanghe H. L., Vielvoye G. J., Meradji M. Idiopathic isosexual central precocious puberty: magnetic resonance findings in 30 patients. Br J Radiol. 1995 Jan;68(805):34–38. doi: 10.1259/0007-1285-68-805-34. [DOI] [PubMed] [Google Scholar]
- Sigurjonsdottir T. J., Hayles A. B. Precocious puberty. A report of 96 cases. Am J Dis Child. 1968 Mar;115(3):309–321. doi: 10.1001/archpedi.1968.02100010311003. [DOI] [PubMed] [Google Scholar]
- Tanner J. M., Whitehouse R. H., Marshall W. A., Carter B. S. Prediction of adult height from height, bone age, and occurrence of menarche, at ages 4 to 16 with allowance for midparent height. Arch Dis Child. 1975 Jan;50(1):14–26. doi: 10.1136/adc.50.1.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wheeler M. D., Styne D. M. Diagnosis and management of precocious puberty. Pediatr Clin North Am. 1990 Dec;37(6):1255–1271. doi: 10.1016/s0031-3955(16)37010-9. [DOI] [PubMed] [Google Scholar]
- Wu F. C., Butler G. E., Kelnar C. J., Huhtaniemi I., Veldhuis J. D. Ontogeny of pulsatile gonadotropin releasing hormone secretion from midchildhood, through puberty, to adulthood in the human male: a study using deconvolution analysis and an ultrasensitive immunofluorometric assay. J Clin Endocrinol Metab. 1996 May;81(5):1798–1805. doi: 10.1210/jcem.81.5.8626838. [DOI] [PubMed] [Google Scholar]
- Zucchini S., di Natale B., Ambrosetto P., De Angelis R., Cacciari E., Chiumello G. Role of magnetic resonance imaging in hypothalamic-pituitary disorders. Horm Res. 1995;44 (Suppl 3):8–14. doi: 10.1159/000184666. [DOI] [PubMed] [Google Scholar]
- Zucchini S., di Natale B., Ambrosetto P., De Angelis R., Cacciari E., Chiumello G. Role of magnetic resonance imaging in hypothalamic-pituitary disorders. Horm Res. 1995;44 (Suppl 3):8–14. doi: 10.1159/000184666. [DOI] [PubMed] [Google Scholar]