Abstract
Background and Aims: Using current WHO guidelines, children with wheezing are being over prescribed antibiotics and bronchodilators are underutilised. To improve the WHO case management guidelines, more data is needed about the clinical outcome in children with wheezing/pneumonia overlap.
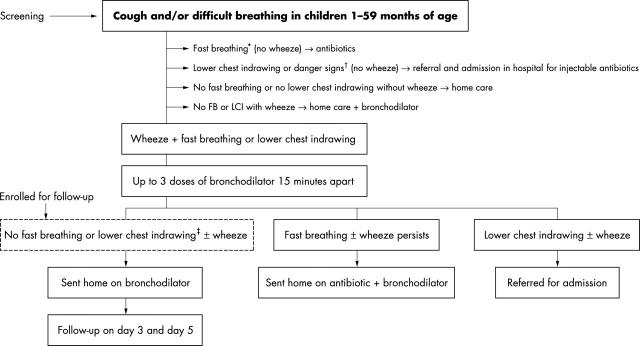
Methodology: In a multicentre prospective study, children aged 1–59 months with auscultatory/audible wheeze and fast breathing and/or lower chest indrawing were screened. Response to up to three cycles of inhaled salbutamol was recorded. The responders were enrolled and sent home on inhaled bronchodilators, and followed up on days 3 and 5.
Results: A total of 1622 children with wheeze were screened from May 2001 to April 2002, of which 1004 (61.8%) had WHO defined non-severe and 618 (38.2%) severe pneumonia. Wheeze was audible in only 595 (36.7%) of children. Of 1004 non-severe pneumonia children, 621 (61.8%) responded to up to three cycles of bronchodilator. Of 618 severe pneumonia children, only 166 (26.8%) responded. Among responders, 93 (14.9%) in the non-severe and 63 (37.9%) children in the severe pneumonia group showed subsequent deterioration on follow ups. No family history of wheeze, temperature >100°F, and lower chest indrawing were identified as predictors of subsequent deterioration.
Conclusions: Two third of children with wheeze are not identified by current WHO ARI (acute respiratory infections) guidelines. Antibiotics are over prescribed and bronchodilators under utilised in children with wheeze. Children with wheeze constitute a special ARI group requiring a separate management algorithm. In countries where wheeze is common it would be worthwhile to train health workers in use of the stethoscope to identify wheeze.
Full Text
The Full Text of this article is available as a PDF (215.2 KB).
Figure 1.
Flow chart of the study. *Children with fast breathing were categorised as non-severe pneumonia. Fast breathing is defined as ⩾60 breaths per minute for up to 2 months of age, ⩾50 breaths per minute for 2–11 months of age, and ⩾ 40 breaths per minute for 12–59 months of age. †Children with lower chest indrawing were categorised as severe pneumonia, whereas those with danger signs (inability to drink, convulsions, vomiting everything, lethargy or unconscious, severe malnutrition) were categorised as very severe disease. ‡These patients were enrolled and followed up at day 3 and day 5. Day of enrolment was considered as day 0. Information on all the patients who presented with wheeze and were screened for the study, whether they were enrolled or not, were recorded by filling in the screening form. These data were also analysed.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bettenay F. A., de Campo J. F., McCrossin D. B. Differentiating bacterial from viral pneumonias in children. Pediatr Radiol. 1988;18(6):453–454. doi: 10.1007/BF00974077. [DOI] [PubMed] [Google Scholar]
- Courtoy I., Lande A. E., Turner R. B. Accuracy of radiographic differentiation of bacterial from nonbacterial pneumonia. Clin Pediatr (Phila) 1989 Jun;28(6):261–264. doi: 10.1177/000992288902800604. [DOI] [PubMed] [Google Scholar]
- McCarthy P. L., Spiesel S. Z., Stashwick C. A., Ablow R. C., Masters S. J., Dolan T. F., Jr Radiographic findings and etiologic diagnosis in ambulatory childhood pneumonias. Clin Pediatr (Phila) 1981 Nov;20(11):686–691. doi: 10.1177/000992288102001101. [DOI] [PubMed] [Google Scholar]
- Panitch H. B. Bronchiolitis in infants. Curr Opin Pediatr. 2001 Jun;13(3):256–260. doi: 10.1097/00008480-200106000-00008. [DOI] [PubMed] [Google Scholar]
- Putto A., Ruuskanen O., Meurman O. Fever in respiratory virus infections. Am J Dis Child. 1986 Nov;140(11):1159–1163. doi: 10.1001/archpedi.1986.02140250085040. [DOI] [PubMed] [Google Scholar]
- Sachdev H. P., Vasanthi B., Satyanarayana L., Puri R. K. Simple predictors to differentiate acute asthma from ARI in children: implications for refining case management in the ARI Control Programme. Indian Pediatr. 1994 Oct;31(10):1251–1259. [PubMed] [Google Scholar]
- Turner R. B., Lande A. E., Chase P., Hilton N., Weinberg D. Pneumonia in pediatric outpatients: cause and clinical manifestations. J Pediatr. 1987 Aug;111(2):194–200. doi: 10.1016/S0022-3476(87)80066-5. [DOI] [PMC free article] [PubMed] [Google Scholar]