Abstract
Background: Children with special needs present a challenge to those involved in their care.
Aims: To determine the role of the acute assessment unit for these children.
Methods: Case notes and other records were reviewed for information on referrals, admissions, readmission within 7 and 28 days, length of stay, and management of 86 children registered for special needs. The study covered five years between January 1997 and December 2001.
Results: Of the 86 children, 48 (58%) were boys; 62 children had cerebral palsy and 52 learning disability. There were 914 episodes, with 44% of these being self referrals and 35% from general practitioners; 35.5% of the episodes were managed in the assessment unit. The average length of stay in hospital was 5 days, ranging from <24 hours to 63 days; 37.5% of those admitted to the ward stayed for less than 24 hours. Respiratory tract infections and seizures were the main reasons for referral and admission.
Conclusion: Children with special needs tend to have a predictable pattern of conditions requiring inpatient care. One third of the inpatients episodes did not need a prolonged stay in hospital. This latter group of children could be managed at home with support of community nurses. Integrated care pathways need to be developed to minimise disruption to their lives. Appropriate resources should be made available to achieve these goals.
Full Text
The Full Text of this article is available as a PDF (209.3 KB).
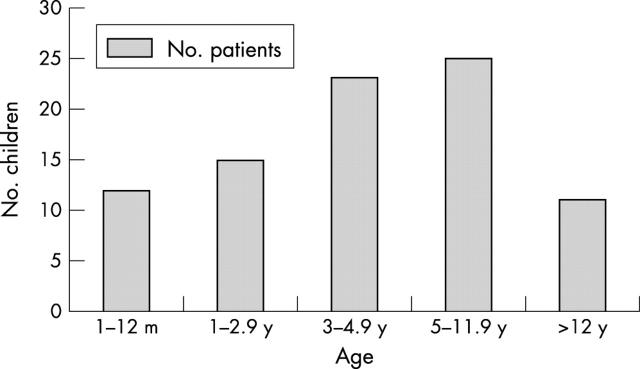
Figure 1 .
Age distribution of patients.
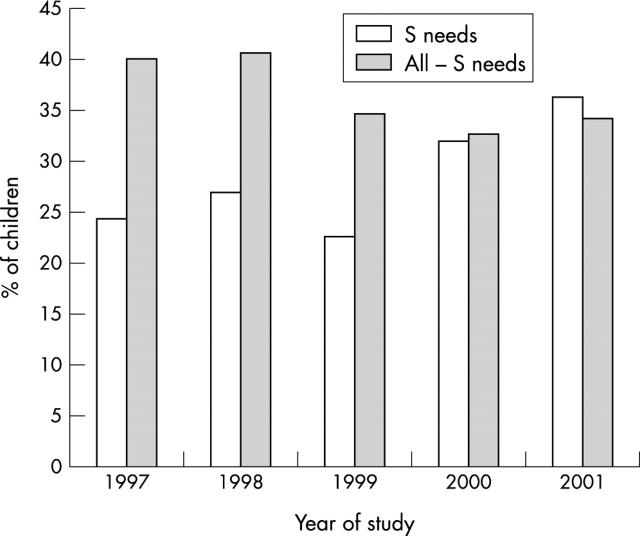
Figure 2 .
Percentage discharges per year from the assessment unit.
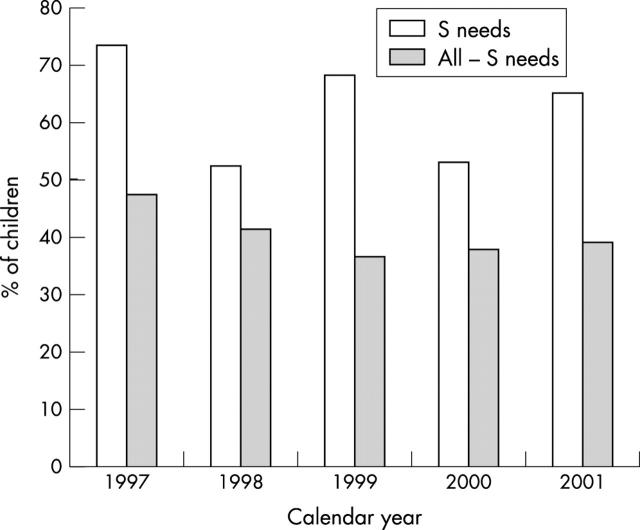
Figure 3 .
Percentage of children staying in hospital over 24 hours.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Armon K., Stephenson T., Gabriel V., MacFaul R., Eccleston P., Werneke U., Smith S. Determining the common medical presenting problems to an accident and emergency department. Arch Dis Child. 2001 May;84(5):390–392. doi: 10.1136/adc.84.5.390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bagust A., Haycox A., Sartain S. A., Maxwell M. J., Todd P. Economic evaluation of an acute paediatric hospital at home clinical trial. Arch Dis Child. 2002 Dec;87(6):489–492. doi: 10.1136/adc.87.6.489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crichton J. U., Mackinnon M., White C. P. The life-expectancy of persons with cerebral palsy. Dev Med Child Neurol. 1995 Jul;37(7):567–576. doi: 10.1111/j.1469-8749.1995.tb12045.x. [DOI] [PubMed] [Google Scholar]
- Depiero A. D., Teach S. J. Febrile seizures. Pediatr Emerg Care. 2001 Oct;17(5):384–387. doi: 10.1097/00006565-200110000-00016. [DOI] [PubMed] [Google Scholar]
- Evans P. M., Evans S. J., Alberman E. Cerebral palsy: why we must plan for survival. Arch Dis Child. 1990 Dec;65(12):1329–1333. doi: 10.1136/adc.65.12.1329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hutton J. L., Colver A. F., Mackie P. C. Effect of severity of disability on survival in north east England cerebral palsy cohort. Arch Dis Child. 2000 Dec;83(6):468–474. doi: 10.1136/adc.83.6.468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hutton J. L., Pharoah P. O. Effects of cognitive, motor, and sensory disabilities on survival in cerebral palsy. Arch Dis Child. 2002 Feb;86(2):84–89. doi: 10.1136/adc.86.2.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lal M. K., Kibirige M. S. Unscheduled return visits within 72 hours to an assessment unit. Arch Dis Child. 1999 May;80(5):455–458. doi: 10.1136/adc.80.5.455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacFaul R., Glass E. J., Jones S. Appropriateness of paediatric admission. Arch Dis Child. 1994 Jul;71(1):50–58. doi: 10.1136/adc.71.1.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacFaul R., Stewart M., Werneke U., Taylor-Meek J., Smith H. E., Smith I. J. Parental and professional perception of need for emergency admission to hospital: prospective questionnaire based study. Arch Dis Child. 1998 Sep;79(3):213–218. doi: 10.1136/adc.79.3.213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mutch L., Ashurst H., Macfarlane A. Birth weight and hospital admission before the age of 2 years. Arch Dis Child. 1992 Jul;67(7):900–904. doi: 10.1136/adc.67.7.900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pachter L. M. Parent's participation and perspectives regarding clinical judgment and clinical guideline development. Curr Opin Pediatr. 1998 Oct;10(5):476–479. doi: 10.1097/00008480-199810000-00004. [DOI] [PubMed] [Google Scholar]
- Scribano P. V., Wiley J. F., 2nd, Platt K. Use of an observation unit by a pediatric emergency department for common pediatric illnesses. Pediatr Emerg Care. 2001 Oct;17(5):321–323. doi: 10.1097/00006565-200110000-00001. [DOI] [PubMed] [Google Scholar]
- Spencer N. J., Lewis M. A., Logan S. Diagnostic and socio-demographic changes in multiple hospital admission in children under two over a five-year period. J Public Health Med. 1993 Dec;15(4):332–336. doi: 10.1093/oxfordjournals.pubmed.a042885. [DOI] [PubMed] [Google Scholar]
- Stewart M., Werneke U., MacFaul R., Taylor-Meek J., Smith H. E., Smith I. J. Medical and social factors associated with the admission and discharge of acutely ill children. Arch Dis Child. 1998 Sep;79(3):219–224. doi: 10.1136/adc.79.3.219. [DOI] [PubMed] [Google Scholar]
- Taylor E. H. Understanding and helping families with neurodevelopmental and neuropsychiatric special needs. Pediatr Clin North Am. 1995 Feb;42(1):143–151. doi: 10.1016/s0031-3955(16)38914-3. [DOI] [PubMed] [Google Scholar]