Abstract
Aims: To determine whether current and postpartum maternal depression and low maternal intelligence are risk factors for malnutrition in children.
Methods: In rural South India 72 children with malnutrition were identified from a central register; 72 controls were matched for age, gender, and residence.
Results: Major depression in the postpartum period (OR 5.0, 95% CI 1.0 to 24.0), current major depression (OR 3.2, 95% CI 1.1 to 9.5), and low maternal intelligence (OR 3.8, 95% CI 1.3 to 11.1) were associated with malnutrition in the child. Low birth weight (OR 2.9, 95% CI 1.2 to 6.8) was also significantly associated with infant malnutrition. Conditional logistic regression adjusting for all other determinants yielded the following results: major depression during the postpartum period (OR 7.8; 95% CI 1.6 to 38.51), current major depression (OR 3.1; 95% CI 0.9 to 9.7), low maternal intelligence (OR 4.6; 95% CI 1.5 to 14.1), and low birth weight (OR 2.7; 95% CI 2.5 to 6.8). The interactions between current maternal depression and low birth weight and between postpartum depression and low maternal intelligence were statistically significant. The level of maternal intelligence was associated with nutritional status. The severity of malnutrition was also significantly associated with major depression during the postpartum period and low maternal intelligence.
Conclusion: There is evidence for an association between postpartum maternal depression, low maternal intelligence, and low birth weight with malnutrition in children aged 6–12 months.
Full Text
The Full Text of this article is available as a PDF (258.5 KB).
Figure 1 .
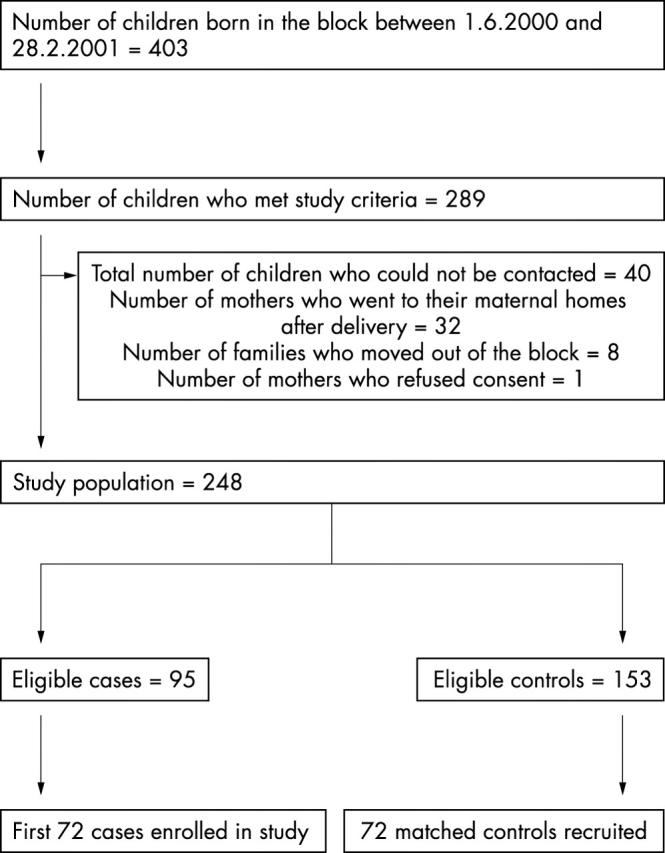
Flow chart of recruitment of cases and controls.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Chandran Mani, Tharyan Prathap, Muliyil Jayaprakash, Abraham Sulochana. Post-partum depression in a cohort of women from a rural area of Tamil Nadu, India. Incidence and risk factors. Br J Psychiatry. 2002 Dec;181:499–504. doi: 10.1192/bjp.181.6.499. [DOI] [PubMed] [Google Scholar]
- Cooper P. J., Murray L. Postnatal depression. BMJ. 1998 Jun 20;316(7148):1884–1886. doi: 10.1136/bmj.316.7148.1884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper P. J., Tomlinson M., Swartz L., Woolgar M., Murray L., Molteno C. Post-partum depression and the mother-infant relationship in a South African peri-urban settlement. Br J Psychiatry. 1999 Dec;175:554–558. doi: 10.1192/bjp.175.6.554. [DOI] [PubMed] [Google Scholar]
- Flaherty J. A., Gaviria F. M., Pathak D., Mitchell T., Wintrob R., Richman J. A., Birz S. Developing instruments for cross-cultural psychiatric research. J Nerv Ment Dis. 1988 May;176(5):257–263. [PubMed] [Google Scholar]
- Gupta S. P. Nutrition--an Indian perspective. Indian J Public Health. 1999 Jan-Mar;43(1):11–16. [PubMed] [Google Scholar]
- Hakeem R. Socio-economic differences in height and body mass index of children and adults living in urban areas of Karachi, Pakistan. Eur J Clin Nutr. 2001 May;55(5):400–406. doi: 10.1038/sj.ejcn.1601172. [DOI] [PubMed] [Google Scholar]
- Islam M. A., Rahman M. M., Mahalanabis D. Maternal and socioeconomic factors and the risk of severe malnutrition in a child: a case-control study. Eur J Clin Nutr. 1994 Jun;48(6):416–424. [PubMed] [Google Scholar]
- Mueller I., Vounatsou P., Allen B. J., Smith T. Spatial patterns of child growth in Papua New Guinea and their relation to environment, diet, socio-economic status and subsistence activities. Ann Hum Biol. 2001 May-Jun;28(3):263–280. doi: 10.1080/030144601300119089. [DOI] [PubMed] [Google Scholar]
- Rauh V. A., Wasserman G. A., Brunelli S. A. Determinants of maternal child-rearing attitudes. J Am Acad Child Adolesc Psychiatry. 1990 May;29(3):375–381. doi: 10.1097/00004583-199005000-00007. [DOI] [PubMed] [Google Scholar]
- Sandiford P., Cassel J., Sanchez G., Coldham C. Does intelligence account for the link between maternal literacy and child survival? Soc Sci Med. 1997 Oct;45(8):1231–1239. doi: 10.1016/s0277-9536(97)00042-7. [DOI] [PubMed] [Google Scholar]
- Spitzer R. L., Williams J. B., Gibbon M., First M. B. The Structured Clinical Interview for DSM-III-R (SCID). I: History, rationale, and description. Arch Gen Psychiatry. 1992 Aug;49(8):624–629. doi: 10.1001/archpsyc.1992.01820080032005. [DOI] [PubMed] [Google Scholar]
- Weinberg M. K., Tronick E. Z. The impact of maternal psychiatric illness on infant development. J Clin Psychiatry. 1998;59 (Suppl 2):53–61. [PubMed] [Google Scholar]


