Abstract
Background: Epidemics of enterovirus 71 infection have caused the death of many children throughout the world. Rhombencephalitis, brain stem encephalitis, and heart failure were present in all of the fatal cases. However, no evidence of myocarditis was noted in the heart specimens, and the mechanism of heart failure remains unknown.
Aims: To characterise the presentation of cardiac complications in children with enterovirus rhombencephalitis and discuss its pathogenesis.
Methods: Ninety one consecutive patients with enterovirus rhombencephalitis underwent echocardiography. Of these, 17 patients (nine male, eight female; median age 14 months, range 4–57 months) with left ventricular dysfunction were studied.
Results: Tachycardia was noted in all patients and systemic hypertension in 12. Muscle-brain fraction of creatine kinase was >5% in 14 patients. Plasma norepinephrine and epinephrine levels were significantly raised in the three patients in whom these were analysed. Electrocardiographic abnormalities were noted in eight patients. Pulmonary oedema was complicated in 15 patients. The initial ejection fraction of the left ventricle was 22–58% (mean 37%, SD 11%). All patients deteriorated to hypotensive shock within 12 hours and 13 died. Heart specimens from seven patients showed no evidence of myocarditis, but significant coagulative myocytolysis, myofibrillar degeneration, and cardiomyocyte apoptosis were observed.
Conclusions: Acute heart failure was noted in 19% of patients with enterovirus rhombencephalitis, which had a fatality rate of 77%. It was not caused by myocarditis but possibly by neurogenic cardiac damage.
Full Text
The Full Text of this article is available as a PDF (796.4 KB).
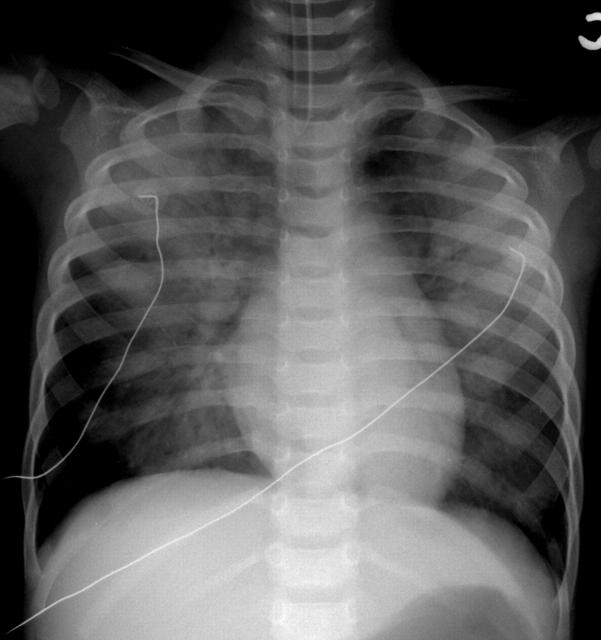
Figure 1 .
Anteroposterior projection of chest radiography in case 17 shows normal heart size and bilateral pulmonary oedema. At the same time, the ejection fraction of the left ventricle was 22% measured by echocardiography.
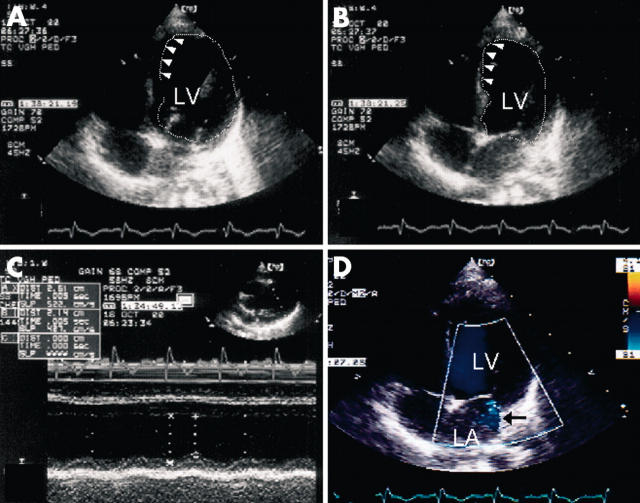
Figure 2 .
Two dimensional echocardiography in 4-chamber view in case 11 shows generalised hypokinesia of the left ventricle with the ejection fraction of 39% (panel A in diastole and panel B in systole). Akinesia of apical septum was also noted (arrowheads). M-mode echocardiography shows poor wall motion of the left ventricle (panel C). Colour Doppler echocardiography shows grade 2+ mitral regurgitation (arrow), flowing into the left atrium (panel D). LA, left atrium; LV, left ventricle.
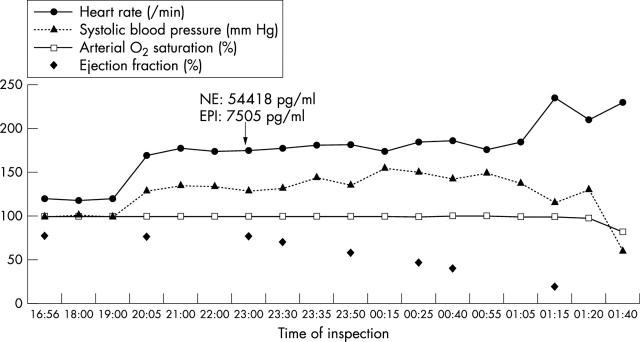
Figure 3 .
Clinical course in case 12 shows that tachycardia, systemic hypertension, and high concentration of plasma catecholamines preceded the occurrence of heart failure. The arterial oxygen saturation was around 100% throughout the course. The patient eventually deteriorated to hypotensive shock.
Figure 4 .
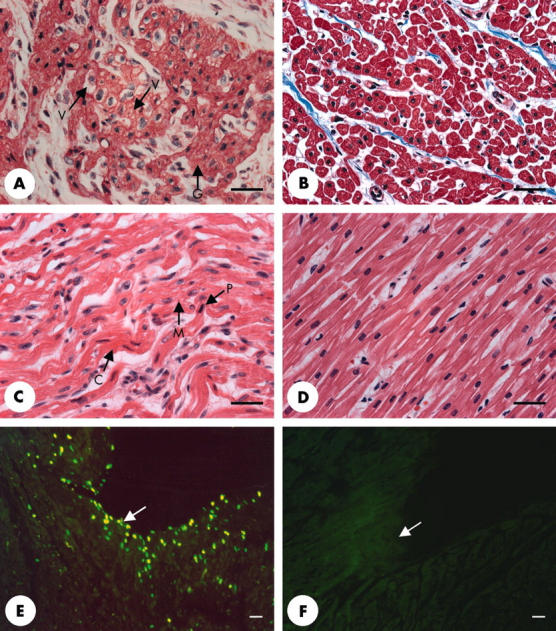
Histopathological examinations of the heart specimens from study patients (left panels) were compared to those from a control, a 4 year old boy who died of sepsis (right panels). Panel A in Masson's trichrome stain and panel C in haematoxylin and eosin stain show significant coagulative myocytolysis and myofibrillar degeneration and waving in the left ventricle, indicated by sarcoplasmic coagulation (C), granulation (G), vacuolisation (V), and myocytolysis (M). Some nuclei became condensed, pyknosis (P), and irregular in shape. Panel E shows significant cardiomyocyte apoptosis, indicated by green fluorescent nuclei and was more remarkable in the subendocardial region (arrow) (in situ TUNEL assay). The bar scales are 30 µm in length.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Brown B. A., Kilpatrick D. R., Oberste M. S., Pallansch M. A. Serotype-specific identification of enterovirus 71 by PCR. J Clin Virol. 2000 Apr;16(2):107–112. doi: 10.1016/s1386-6532(00)00065-2. [DOI] [PubMed] [Google Scholar]
- Chan L. G., Parashar U. D., Lye M. S., Ong F. G., Zaki S. R., Alexander J. P., Ho K. K., Han L. L., Pallansch M. A., Suleiman A. B. Deaths of children during an outbreak of hand, foot, and mouth disease in sarawak, malaysia: clinical and pathological characteristics of the disease. For the Outbreak Study Group. Clin Infect Dis. 2000 Oct 4;31(3):678–683. doi: 10.1086/314032. [DOI] [PubMed] [Google Scholar]
- Cheng F. C., Yang L. L., Chang F. M., Chia L. G., Kuo J. S. Simultaneous measurement of serotonin, catecholamines and their metabolites in cat and human plasma by in vitro microdialysis-microbore high-performance liquid chromatography with amperometric detection. J Chromatogr. 1992 Nov 6;582(1-2):19–27. doi: 10.1016/0378-4347(92)80297-4. [DOI] [PubMed] [Google Scholar]
- Colice G. L. Detecting the presence and cause of pulmonary edema. Postgrad Med. 1993 May 1;93(6):161-6, 169-70. doi: 10.1080/00325481.1993.11701691. [DOI] [PubMed] [Google Scholar]
- Communal C., Singh K., Pimentel D. R., Colucci W. S. Norepinephrine stimulates apoptosis in adult rat ventricular myocytes by activation of the beta-adrenergic pathway. Circulation. 1998 Sep 29;98(13):1329–1334. doi: 10.1161/01.cir.98.13.1329. [DOI] [PubMed] [Google Scholar]
- Connor R. C. Heart damage associated with intracranial lesions. Br Med J. 1968 Jul 6;3(5609):29–31. doi: 10.1136/bmj.3.5609.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heatwole V. M. TUNEL assay for apoptotic cells. Methods Mol Biol. 1999;115:141–148. doi: 10.1385/1-59259-213-9:141. [DOI] [PubMed] [Google Scholar]
- Ho M., Chen E. R., Hsu K. H., Twu S. J., Chen K. T., Tsai S. F., Wang J. R., Shih S. R. An epidemic of enterovirus 71 infection in Taiwan. Taiwan Enterovirus Epidemic Working Group. N Engl J Med. 1999 Sep 23;341(13):929–935. doi: 10.1056/NEJM199909233411301. [DOI] [PubMed] [Google Scholar]
- Huang C. C., Liu C. C., Chang Y. C., Chen C. Y., Wang S. T., Yeh T. F. Neurologic complications in children with enterovirus 71 infection. N Engl J Med. 1999 Sep 23;341(13):936–942. doi: 10.1056/NEJM199909233411302. [DOI] [PubMed] [Google Scholar]
- Huang Fang-Liang, Jan Sheng-Ling, Chen Po-Yen, Chi Ching-Shiang, Wang Teh-Ming, Fu Yun-Ching, Tsai Chi-Ren, Chang Yan. Left ventricular dysfunction in children with fulminant enterovirus 71 infection: an evaluation of the clinical course. Clin Infect Dis. 2002 Mar 4;34(7):1020–1024. doi: 10.1086/339445. [DOI] [PubMed] [Google Scholar]
- Jan S. L., Chi C. S., Hwang B., Fu Y. C., Chen P. Y., Mak S. C. Cardiac manifestations of fatal enterovirus infection during the 1998 outbreak in Taiwan. Zhonghua Yi Xue Za Zhi (Taipei) 2000 Aug;63(8):612–618. [PubMed] [Google Scholar]
- Lum L. C., Wong K. T., Lam S. K., Chua K. B., Goh A. Y., Lim W. L., Ong B. B., Paul G., AbuBakar S., Lambert M. Fatal enterovirus 71 encephalomyelitis. J Pediatr. 1998 Dec;133(6):795–798. doi: 10.1016/s0022-3476(98)70155-6. [DOI] [PubMed] [Google Scholar]
- Marion D. W., Segal R., Thompson M. E. Subarachnoid hemorrhage and the heart. Neurosurgery. 1986 Jan;18(1):101–106. doi: 10.1227/00006123-198601000-00019. [DOI] [PubMed] [Google Scholar]
- Miyatake K., Izumi S., Okamoto M., Kinoshita N., Asonuma H., Nakagawa H., Yamamoto K., Takamiya M., Sakakibara H., Nimura Y. Semiquantitative grading of severity of mitral regurgitation by real-time two-dimensional Doppler flow imaging technique. J Am Coll Cardiol. 1986 Jan;7(1):82–88. doi: 10.1016/s0735-1097(86)80263-7. [DOI] [PubMed] [Google Scholar]
- Nagy G., Takátsy S., Kukán E., Mihály I., Dömök I. Virological diagnosis of enterovirus type 71 infections: experiences gained during an epidemic of acute CNS diseases in Hungary in 1978. Arch Virol. 1982;71(3):217–227. doi: 10.1007/BF01314873. [DOI] [PubMed] [Google Scholar]
- Narula J., Hajjar R. J., Dec G. W. Apoptosis in the failing heart. Cardiol Clin. 1998 Nov;16(4):691-710, ix. doi: 10.1016/s0733-8651(05)70045-x. [DOI] [PubMed] [Google Scholar]
- Pollick C., Cujec B., Parker S., Tator C. Left ventricular wall motion abnormalities in subarachnoid hemorrhage: an echocardiographic study. J Am Coll Cardiol. 1988 Sep;12(3):600–605. doi: 10.1016/s0735-1097(88)80044-5. [DOI] [PubMed] [Google Scholar]
- Samuels M. A. Neurally induced cardiac damage. Definition of the problem. Neurol Clin. 1993 May;11(2):273–292. [PubMed] [Google Scholar]
- Sato K., Masuda T., Izumi T. Subarachnoid hemorrhage and myocardial damage clinical and experimental studies. Jpn Heart J. 1999 Nov;40(6):683–701. doi: 10.1536/jhj.40.683. [DOI] [PubMed] [Google Scholar]
- Satou G. M., Lacro R. V., Chung T., Gauvreau K., Jenkins K. J. Heart size on chest x-ray as a predictor of cardiac enlargement by echocardiography in children. Pediatr Cardiol. 2001 May-Jun;22(3):218–222. doi: 10.1007/s002460010207. [DOI] [PubMed] [Google Scholar]
- Schmidt N. J., Lennette E. H., Ho H. H. An apparently new enterovirus isolated from patients with disease of the central nervous system. J Infect Dis. 1974 Mar;129(3):304–309. doi: 10.1093/infdis/129.3.304. [DOI] [PubMed] [Google Scholar]
- Shindarov L. M., Chumakov M. P., Voroshilova M. K., Bojinov S., Vasilenko S. M., Iordanov I., Kirov I. D., Kamenov E., Leshchinskaya E. V., Mitov G. Epidemiological, clinical, and pathomorphological characteristics of epidemic poliomyelitis-like disease caused by enterovirus 71. J Hyg Epidemiol Microbiol Immunol. 1979;23(3):284–295. [PubMed] [Google Scholar]
- Williams R. S. Apoptosis and heart failure. N Engl J Med. 1999 Sep 2;341(10):759–760. doi: 10.1056/NEJM199909023411012. [DOI] [PubMed] [Google Scholar]
- Zoll G. J., Melchers W. J., Kopecka H., Jambroes G., van der Poel H. J., Galama J. M. General primer-mediated polymerase chain reaction for detection of enteroviruses: application for diagnostic routine and persistent infections. J Clin Microbiol. 1992 Jan;30(1):160–165. doi: 10.1128/jcm.30.1.160-165.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]