Abstract
Background: The classical extrapyramidal movement disorder following ß haemolytic streptococcus (BHS) infection is Sydenham's chorea (SC). Recently, other post-streptococcal movement disorders have been described, including motor tics and dystonia. Associated emotional and behavioural alteration is characteristic.
Aims: To describe experience of post-streptococcal dyskinesias and associated co-morbid psychiatric features presenting to a tertiary referral centre 1999–2002.
Methods: In all patients, dyskinetic movement disorders followed BHS pharyngeal infection. BHS infection was defined by pharyngeal culture of the organism, or paired streptococcal serology. Movement disorders were classified according to international criteria, and validated by experienced child neurologists. Psychiatric complications were defined using ICD-10 criteria using a validated psychiatric interview.
Results: In the 40 patients, the following dyskinetic movement disorders were present: chorea (n = 20), motor tics (n = 16), dystonia (n = 5), tremor (n = 3), stereotypies (n = 2), opsoclonus (n = 2), and myoclonus (n = 1). Sixty five per cent of the chorea patients were female, whereas 69% of the tic patients were male. ICD-10 psychiatric diagnoses were made in 62.5%. Using the same psychiatric instrument, only 8.9% of UK children would be expected to have an ICD-10 psychiatric diagnosis. Emotional disorders occurred in 47.5%, including obsessive-compulsive disorder (27.5%), generalised anxiety (25%), and depressive episode (17.5%). Additional psychiatric morbidity included conduct disorders (27.5%) and hyperkinetic disorders (15%). Psychiatric, movement, and post-streptococcal autoimmune disorders were commonly observed in family members. At a mean follow up of 2.7 years, 72.5% had continuing movement and psychiatric disorders.
Conclusion: Post-streptococcal dyskinesias occur with significant and disabling psychiatric co-morbidity and are potential autoimmune models of common "idiopathic" movement and psychiatric disorders in children. Multiple factors may be involved in disease expression including genetic predisposition, developmental status, and the patient's sex.
Full Text
The Full Text of this article is available as a PDF (105.2 KB).
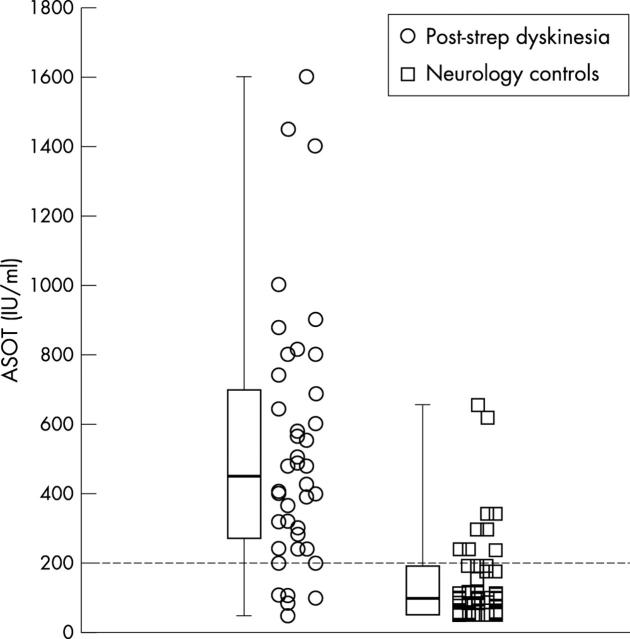
Figure 1.
ASOT in post-streptococcal dyskinesia and neurological controls. Bars presented are 0th, 25th, 50th, 75th, and 100th centiles.
Figure 2.
Anti-DNase B in post-streptococcal dyskinesia and neurological controls. Bars presented are 0th, 25th, 50th, 75th, and 100th centiles.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Albin R. L., Young A. B., Penney J. B. The functional anatomy of basal ganglia disorders. Trends Neurosci. 1989 Oct;12(10):366–375. doi: 10.1016/0166-2236(89)90074-x. [DOI] [PubMed] [Google Scholar]
- Asbahr F. R., Ramos R. T., Negrão A. B., Gentil V. Case series: increased vulnerability to obsessive-compulsive symptoms with repeated episodes of Sydenham chorea. J Am Acad Child Adolesc Psychiatry. 1999 Dec;38(12):1522–1525. doi: 10.1097/00004583-199912000-00013. [DOI] [PubMed] [Google Scholar]
- Cardoso F., Vargas A. P., Oliveira L. D., Guerra A. A., Amaral S. V. Persistent Sydenham's chorea. Mov Disord. 1999 Sep;14(5):805–807. doi: 10.1002/1531-8257(199909)14:5<805::aid-mds1013>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- Church A. J., Cardoso F., Dale R. C., Lees A. J., Thompson E. J., Giovannoni G. Anti-basal ganglia antibodies in acute and persistent Sydenham's chorea. Neurology. 2002 Jul 23;59(2):227–231. doi: 10.1212/wnl.59.2.227. [DOI] [PubMed] [Google Scholar]
- Church A. J., Dale R. C., Giovannoni G. Anti-basal ganglia antibodies: a possible diagnostic utility in idiopathic movement disorders? Arch Dis Child. 2004 Jul;89(7):611–614. doi: 10.1136/adc.2003.031880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dajani A. S., Bisno A. L., Chung K. J., Durack D. T., Gerber M. A., Kaplan E. L., Millard H. D., Randolph M. F., Shulman S. T., Watanakunakorn C. Prevention of rheumatic fever: a statement for health professionals by the Committee on Rheumatic Fever, Endocarditis and Kawasaki Disease of the Council on Cardiovascular Disease in the young, the American Heart Association. Pediatr Infect Dis J. 1989 May;8(5):263–266. [PubMed] [Google Scholar]
- Dale R. C., Church A. J., Cardoso F., Goddard E., Cox T. C., Chong W. K., Williams A., Klein N. J., Neville B. G., Thompson E. J. Poststreptococcal acute disseminated encephalomyelitis with basal ganglia involvement and auto-reactive antibasal ganglia antibodies. Ann Neurol. 2001 Nov;50(5):588–595. doi: 10.1002/ana.1250. [DOI] [PubMed] [Google Scholar]
- Dale Russell C., Church Andrew J., Benton Sarah, Surtees Robert A., Lees Andrew, Thompson Edward J., Giovannoni Gavin, Neville Brian G. Post-streptococcal autoimmune dystonia with isolated bilateral striatal necrosis. Dev Med Child Neurol. 2002 Jul;44(7):485–489. doi: 10.1017/s0012162201002390. [DOI] [PubMed] [Google Scholar]
- Dale Russell C., Church Andrew J., Surtees Robert A. H., Thompson Edward J., Giovannoni Gavin, Neville Brian G. R. Post-streptococcal autoimmune neuropsychiatric disease presenting as paroxysmal dystonic choreoathetosis. Mov Disord. 2002 Jul;17(4):817–820. doi: 10.1002/mds.10169. [DOI] [PubMed] [Google Scholar]
- DiFazio M. P., Morales J., Davis R. Acute myoclonus secondary to group A beta-hemolytic streptococcus infection: A PANDAS variant. J Child Neurol. 1998 Oct;13(10):516–518. doi: 10.1177/088307389801301010. [DOI] [PubMed] [Google Scholar]
- FREEMAN J. M., ARON A. M., COLLARD J. E., MACKAY M. C. THE EMOTIONAL CORRELATES OF SYDENHAM'S CHOREA. Pediatrics. 1965 Jan;35:42–49. [PubMed] [Google Scholar]
- Garvey M. A., Perlmutter S. J., Allen A. J., Hamburger S., Lougee L., Leonard H. L., Witowski M. E., Dubbert B., Swedo S. E. A pilot study of penicillin prophylaxis for neuropsychiatric exacerbations triggered by streptococcal infections. Biol Psychiatry. 1999 Jun 15;45(12):1564–1571. doi: 10.1016/s0006-3223(99)00020-7. [DOI] [PubMed] [Google Scholar]
- Gibofsky A., Khanna A., Suh E., Zabriskie J. B. The genetics of rheumatic fever: relationship to streptococcal infection and autoimmune disease. J Rheumatol Suppl. 1991 Aug;30:1–5. [PubMed] [Google Scholar]
- Giedd J. N., Rapoport J. L., Garvey M. A., Perlmutter S., Swedo S. E. MRI assessment of children with obsessive-compulsive disorder or tics associated with streptococcal infection. Am J Psychiatry. 2000 Feb;157(2):281–283. doi: 10.1176/appi.ajp.157.2.281. [DOI] [PubMed] [Google Scholar]
- Giedd J. N., Rapoport J. L., Kruesi M. J., Parker C., Schapiro M. B., Allen A. J., Leonard H. L., Kaysen D., Dickstein D. P., Marsh W. L. Sydenham's chorea: magnetic resonance imaging of the basal ganglia. Neurology. 1995 Dec;45(12):2199–2202. doi: 10.1212/wnl.45.12.2199. [DOI] [PubMed] [Google Scholar]
- Goodman R., Ford T., Richards H., Gatward R., Meltzer H. The Development and Well-Being Assessment: description and initial validation of an integrated assessment of child and adolescent psychopathology. J Child Psychol Psychiatry. 2000 Jul;41(5):645–655. [PubMed] [Google Scholar]
- Goodman R. Psychometric properties of the strengths and difficulties questionnaire. J Am Acad Child Adolesc Psychiatry. 2001 Nov;40(11):1337–1345. doi: 10.1097/00004583-200111000-00015. [DOI] [PubMed] [Google Scholar]
- Green L. N. Corticosteroids in the treatment of Sydenham's chorea. Arch Neurol. 1978 Jan;35(1):53–54. doi: 10.1001/archneur.1978.00500250057015. [DOI] [PubMed] [Google Scholar]
- Husby G., van de Rijn I., Zabriskie J. B., Abdin Z. H., Williams R. C., Jr Antibodies reacting with cytoplasm of subthalamic and caudate nuclei neurons in chorea and acute rheumatic fever. J Exp Med. 1976 Oct 1;144(4):1094–1110. doi: 10.1084/jem.144.4.1094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jankovic J., Ashizawa T. Tourettism associated with Huntington's disease. Mov Disord. 1995 Jan;10(1):103–105. doi: 10.1002/mds.870100116. [DOI] [PubMed] [Google Scholar]
- Jankovic J. International Classification of Diseases, tenth revision: neurological adaptation (ICD-10 NA): extrapyramidal and movement disorders. Mov Disord. 1995 Sep;10(5):533–540. doi: 10.1002/mds.870100502. [DOI] [PubMed] [Google Scholar]
- Kerbeshian J., Burd L., Pettit R. A possible post-streptococcal movement disorder with chorea and tics. Dev Med Child Neurol. 1990 Jul;32(7):642–644. [PubMed] [Google Scholar]
- Khanna A. K., Buskirk D. R., Williams R. C., Jr, Gibofsky A., Crow M. K., Menon A., Fotino M., Reid H. M., Poon-King T., Rubinstein P. Presence of a non-HLA B cell antigen in rheumatic fever patients and their families as defined by a monoclonal antibody. J Clin Invest. 1989 May;83(5):1710–1716. doi: 10.1172/JCI114071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiessling L. S., Marcotte A. C., Culpepper L. Antineuronal antibodies in movement disorders. Pediatrics. 1993 Jul;92(1):39–43. [PubMed] [Google Scholar]
- Loiselle Christopher R., Wendlandt John T., Rohde Charles A., Singer Harvey S. Antistreptococcal, neuronal, and nuclear antibodies in Tourette syndrome. Pediatr Neurol. 2003 Feb;28(2):119–125. doi: 10.1016/s0887-8994(02)00507-6. [DOI] [PubMed] [Google Scholar]
- Lougee L., Perlmutter S. J., Nicolson R., Garvey M. A., Swedo S. E. Psychiatric disorders in first-degree relatives of children with pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections (PANDAS). J Am Acad Child Adolesc Psychiatry. 2000 Sep;39(9):1120–1126. doi: 10.1097/00004583-200009000-00011. [DOI] [PubMed] [Google Scholar]
- Mercadante M. T., Busatto G. F., Lombroso P. J., Prado L., Rosário-Campos M. C., do Valle R., Marques-Dias M. J., Kiss M. H., Leckman J. F., Miguel E. C. The psychiatric symptoms of rheumatic fever. Am J Psychiatry. 2000 Dec;157(12):2036–2038. doi: 10.1176/appi.ajp.157.12.2036. [DOI] [PubMed] [Google Scholar]
- Mercadante M. T., Campos M. C., Marques-Dias M. J., Miguel E. C., Leckman J. Vocal tics in Sydenham's chorea. J Am Acad Child Adolesc Psychiatry. 1997 Mar;36(3):305–306. doi: 10.1097/00004583-199703000-00007. [DOI] [PubMed] [Google Scholar]
- Moore D. P. Neuropsychiatric aspects of Sydenham's chorea: a comprehensive review. J Clin Psychiatry. 1996 Sep;57(9):407–414. [PubMed] [Google Scholar]
- Murphy Marie Lynd, Pichichero Michael E. Prospective identification and treatment of children with pediatric autoimmune neuropsychiatric disorder associated with group A streptococcal infection (PANDAS). Arch Pediatr Adolesc Med. 2002 Apr;156(4):356–361. doi: 10.1001/archpedi.156.4.356. [DOI] [PubMed] [Google Scholar]
- Murphy T. K., Goodman W. K., Ayoub E. M., Voeller K. K. On defining Sydenham's chorea: where do we draw the line? Biol Psychiatry. 2000 May 15;47(10):851–857. doi: 10.1016/s0006-3223(00)00843-x. [DOI] [PubMed] [Google Scholar]
- Nausieda P. A., Grossman B. J., Koller W. C., Weiner W. J., Klawans H. L. Sydenham chorea: an update. Neurology. 1980 Mar;30(3):331–334. doi: 10.1212/wnl.30.3.331. [DOI] [PubMed] [Google Scholar]
- Nausieda P. A., Koller W. C., Weiner W. J., Klawans H. L. Chorea induced by oral contraceptives. Neurology. 1979 Dec;29(12):1605–1609. doi: 10.1212/wnl.29.12.1605. [DOI] [PubMed] [Google Scholar]
- Perlmutter S. J., Leitman S. F., Garvey M. A., Hamburger S., Feldman E., Leonard H. L., Swedo S. E. Therapeutic plasma exchange and intravenous immunoglobulin for obsessive-compulsive disorder and tic disorders in childhood. Lancet. 1999 Oct 2;354(9185):1153–1158. doi: 10.1016/S0140-6736(98)12297-3. [DOI] [PubMed] [Google Scholar]
- Rye David B., Jankovic Joseph. Emerging views of dopamine in modulating sleep/wake state from an unlikely source: PD. Neurology. 2002 Feb 12;58(3):341–346. doi: 10.1212/wnl.58.3.341. [DOI] [PubMed] [Google Scholar]
- Sacks O. W. Acquired Tourettism in adult life. Adv Neurol. 1982;35:89–92. [PubMed] [Google Scholar]
- Silvestri R., Raffaele M., De Domenico P., Tisano A., Mento G., Casella C., Tripoli M. C., Serra S., Di Perri R. Sleep features in Tourette's syndrome, neuroacanthocytosis and Huntington's chorea. Neurophysiol Clin. 1995;25(2):66–77. doi: 10.1016/0987-7053(96)81034-3. [DOI] [PubMed] [Google Scholar]
- Singer H. S., Giuliano J. D., Hansen B. H., Hallett J. J., Laurino J. P., Benson M., Kiessling L. S. Antibodies against human putamen in children with Tourette syndrome. Neurology. 1998 Jun;50(6):1618–1624. doi: 10.1212/wnl.50.6.1618. [DOI] [PubMed] [Google Scholar]
- Singer H. S., Walkup J. T. Tourette syndrome and other tic disorders. Diagnosis, pathophysiology, and treatment. Medicine (Baltimore) 1991 Jan;70(1):15–32. doi: 10.1097/00005792-199101000-00002. [DOI] [PubMed] [Google Scholar]
- Singer Harvey S., Loiselle Christopher. PANDAS: a commentary. J Psychosom Res. 2003 Jul;55(1):31–39. doi: 10.1016/s0022-3999(02)00582-2. [DOI] [PubMed] [Google Scholar]
- Swedo S. E., Leonard H. L., Garvey M., Mittleman B., Allen A. J., Perlmutter S., Lougee L., Dow S., Zamkoff J., Dubbert B. K. Pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections: clinical description of the first 50 cases. Am J Psychiatry. 1998 Feb;155(2):264–271. doi: 10.1176/ajp.155.2.264. [DOI] [PubMed] [Google Scholar]
- Swedo S. E., Leonard H. L., Mittleman B. B., Allen A. J., Rapoport J. L., Dow S. P., Kanter M. E., Chapman F., Zabriskie J. Identification of children with pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections by a marker associated with rheumatic fever. Am J Psychiatry. 1997 Jan;154(1):110–112. doi: 10.1176/ajp.154.1.110. [DOI] [PubMed] [Google Scholar]
- Swedo S. E., Rapoport J. L., Cheslow D. L., Leonard H. L., Ayoub E. M., Hosier D. M., Wald E. R. High prevalence of obsessive-compulsive symptoms in patients with Sydenham's chorea. Am J Psychiatry. 1989 Feb;146(2):246–249. doi: 10.1176/ajp.146.2.246. [DOI] [PubMed] [Google Scholar]
- van Dijk J. G., van der Velde E. A., Roos R. A., Bruyn G. W. Juvenile Huntington disease. Hum Genet. 1986 Jul;73(3):235–239. doi: 10.1007/BF00401235. [DOI] [PubMed] [Google Scholar]