Abstract
Background: The diagnosis of childhood pulmonary tuberculosis presents a major challenge as symptoms traditionally associated with tuberculosis are extremely common in children from endemic areas. The natural history of tuberculosis in children shows that progressive disease is associated with symptoms which have a persistent, non-remitting character. The aims of this study were to investigate whether improved symptom definition is possible in a clinical setting, and whether use of these well defined symptoms has improved value in the diagnosis of childhood pulmonary tuberculosis.
Methods: A prospective, community based study was conducted in two suburbs of Cape Town, South Africa. All children (<13 years) presenting to the local community clinic with a cough of >2 weeks duration, were referred to the investigator. Parents completed a symptom based questionnaire, whereafter reported symptoms were characterised in a standard fashion.
Results: Of the 151 children enrolled, 21 (15.6%) reported symptoms with a persistent, non-remitting character. Tuberculosis was diagnosed in 16 (10.5%) children, all of whom reported these symptom characteristics. A persistent, non-remitting cough was reported in 15/16 (93.8%) children with tuberculosis and in 2/135 (1.5%) children without tuberculosis, indicating a specificity of 98.5% (135/137). Persistent fatigue of recent onset was also sensitive (13/16, 81.3%) and specific (134/135, 99.3%). Persistent fever and/or chest pain were exclusively reported in children with tuberculosis, but were present in only 4/16 (25.0%) children with tuberculosis.
Conclusion: The use of well defined symptoms is feasible, even in resource limited settings, and may offer significantly improved value in the diagnosis of childhood pulmonary tuberculosis.
Full Text
The Full Text of this article is available as a PDF (73.7 KB).
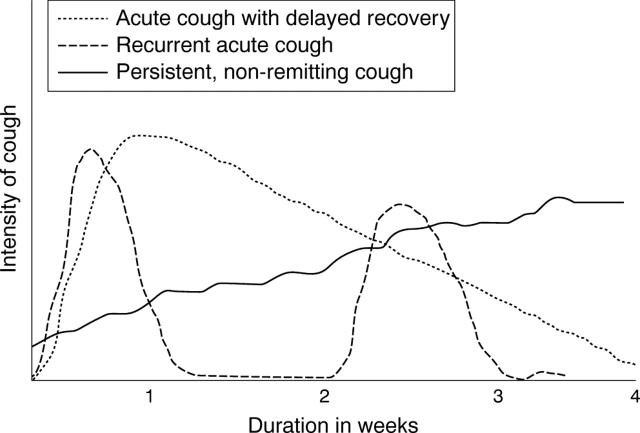
Figure 1.
Differentiated cough patterns.
Figure 2.
The frequency of specific cough patterns associated with different clinical diagnoses (n = 151).
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Eamranond P., Jaramillo E. Tuberculosis in children: reassessing the need for improved diagnosis in global control strategies. Int J Tuberc Lung Dis. 2001 Jul;5(7):594–603. [PubMed] [Google Scholar]
- GEDDE-DAHL T. Tuberculous infection in the light of tuberculin matriculation. Am J Hyg. 1952 Sep;56(2):139–214. doi: 10.1093/oxfordjournals.aje.a119547. [DOI] [PubMed] [Google Scholar]
- Hesseling A. C., Schaaf H. S., Gie R. P., Starke J. R., Beyers N. A critical review of diagnostic approaches used in the diagnosis of childhood tuberculosis. Int J Tuberc Lung Dis. 2002 Dec;6(12):1038–1045. [PubMed] [Google Scholar]
- Houwert K. A., Borggreven P. A., Schaaf H. S., Nel E., Donald P. R., Stolk J. Prospective evaluation of World Health Organization criteria to assist diagnosis of tuberculosis in children. Eur Respir J. 1998 May;11(5):1116–1120. doi: 10.1183/09031936.98.11051116. [DOI] [PubMed] [Google Scholar]
- Marais B. J., Gie R. P., Schaaf H. S., Hesseling A. C., Obihara C. C., Starke J. J., Enarson D. A., Donald P. R., Beyers N. The natural history of childhood intra-thoracic tuberculosis: a critical review of literature from the pre-chemotherapy era. Int J Tuberc Lung Dis. 2004 Apr;8(4):392–402. [PubMed] [Google Scholar]
- Marais B. J., Obihara C. C., Gie R. P., Schaaf H. S., Hesseling A. C., Lombard C., Enarson D., Bateman E., Beyers N. The prevalence of symptoms associated with pulmonary tuberculosis in randomly selected children from a high burden community. Arch Dis Child. 2005 Nov;90(11):1166–1170. doi: 10.1136/adc.2004.060640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Brien Richard J., Talbot Elizabeth A. The utility of an antibiotic trial for diagnosis of AFB-negative tuberculosis. Int J Tuberc Lung Dis. 2003 Feb;7(2):198–198. [PubMed] [Google Scholar]
- Osborne C. M. The challenge of diagnosing childhood tuberculosis in a developing country. Arch Dis Child. 1995 Apr;72(4):369–374. doi: 10.1136/adc.72.4.369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salazar G. E., Schmitz T. L., Cama R., Sheen P., Franchi L. M., Centeno G., Valera C., Leyva M., Montenegro-James S., Oberhelman R. Pulmonary tuberculosis in children in a developing country. Pediatrics. 2001 Aug;108(2):448–453. doi: 10.1542/peds.108.2.448. [DOI] [PubMed] [Google Scholar]
- Schaaf H. S., Beyers N., Gie R. P., Nel E. D., Smuts N. A., Scøtt F. E., Donald P. R., Fourie P. B. Respiratory tuberculosis in childhood: the diagnostic value of clinical features and special investigations. Pediatr Infect Dis J. 1995 Mar;14(3):189–194. [PubMed] [Google Scholar]
- Starke J. R. Childhood tuberculosis. A diagnostic dilemma. Chest. 1993 Aug;104(2):329–330. doi: 10.1378/chest.104.2.329. [DOI] [PubMed] [Google Scholar]
- Stoltz A. P., Donald P. R., Strebel P. M., Talent J. M. Criteria for the notification of childhood tuberculosis in a high-incidence area of the western Cape Province. S Afr Med J. 1990 Apr 21;77(8):385–386. [PubMed] [Google Scholar]
- Verver Suzanne, Warren Robin M., Munch Zahn, Richardson Madalene, van der Spuy Gian D., Borgdorff Martien W., Behr Marcel A., Beyers Nulda, van Helden Paul D. Proportion of tuberculosis transmission that takes place in households in a high-incidence area. Lancet. 2004 Jan 17;363(9404):212–214. doi: 10.1016/S0140-6736(03)15332-9. [DOI] [PubMed] [Google Scholar]
- Wilkinson D., De Cock K. M., Sturm A. W. Diagnosing tuberculosis in a resource-poor setting: the value of a trial of antibiotics. Trans R Soc Trop Med Hyg. 1997 Jul-Aug;91(4):422–424. doi: 10.1016/s0035-9203(97)90264-9. [DOI] [PubMed] [Google Scholar]