Abstract
Aims: To review clinical features and outcome of children with severe Staphylococcus aureus sepsis (SAS) presenting to a paediatric intensive care unit (PICU) with particular focus on ethnicity, clinical presentation, cardiac involvement, and outcome.
Methods: Retrospective chart review of patients coded for SAS over 10 years (October 1993 to April 2004).
Results: There were 58 patients identified with SAS over the 10 year study period; 55 were community acquired. This accounted for 4% of hospital admissions for SAS over this time; children with staphylococcal illness comprised 1% of all admissions to the PICU. Maori and Pacific children with SAS were overly represented in the PICU (81%) from a paediatric population where they contribute 21.6%. Musculoskeletal symptoms (79%) dominated presentation rather than isolated pneumonia (10%). An aggressive search for foci and surgical drainage of infective foci was required in 50% of children. Most children had multifocal disease (67%) and normal cardiac valves (95%); the few children (12%) presenting with methicillin resistant S aureus (MRSA) had community acquired infection. The median length of stay in the PICU was 3 (mean 5.8, SD 7.6, range 1–44) days. The median length of stay in hospital was 15 (mean 21, SD 22.7, range 2–149) days. Mortality due to SAS was 8.6% (95% CI 1.4–15.8%) compared with the overall mortality for the PICU of 6% (95% CI 5.3–6.7%). Ten children had significant morbidity after discharge.
Conclusions: Community acquired SAS affects healthy children, is multifocal, and has high morbidity and mortality, in keeping with the high severity of illness scores on admission. It is imperative to look for sites of dissemination and to drain and debride foci. Routine echocardiography had low yield in the absence of pre-existing cardiac lesions, persisting fever, or persisting bacteraemia.
Full Text
The Full Text of this article is available as a PDF (86.9 KB).
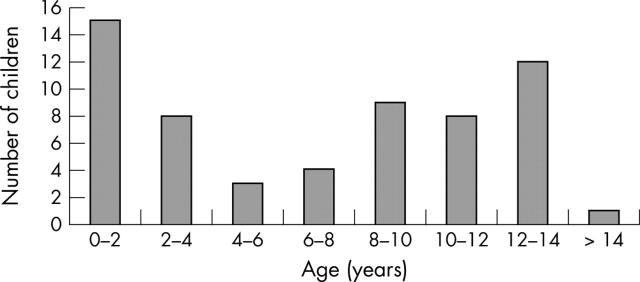
Figure 1.
Age distribution of children with S aureus sepsis presenting to a PICU in New Zealand.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Abbott W., Scragg R., Marbrook J. Differences in disease frequency between Europeans and Polynesians: directions for future research into genetic risk factors. N Z Med J. 1999 Jul 9;112(1091):243–245. [PubMed] [Google Scholar]
- Archer G. L., Climo M. W. Staphylococcus aureus bacteremia--consider the source. N Engl J Med. 2001 Jan 4;344(1):55–56. doi: 10.1056/NEJM200101043440110. [DOI] [PubMed] [Google Scholar]
- Baker M., McNicholas A., Garrett N., Jones N., Stewart J., Koberstein V., Lennon D. Household crowding a major risk factor for epidemic meningococcal disease in Auckland children. Pediatr Infect Dis J. 2000 Oct;19(10):983–990. doi: 10.1097/00006454-200010000-00009. [DOI] [PubMed] [Google Scholar]
- Bone R. C., Sibbald W. J., Sprung C. L. The ACCP-SCCM consensus conference on sepsis and organ failure. Chest. 1992 Jun;101(6):1481–1483. doi: 10.1378/chest.101.6.1481. [DOI] [PubMed] [Google Scholar]
- Chang I-Jing, Yang Chia-Yi, Sung Feng-Yi, Ng Kai-Yam. A red-brown plaque on the nape. Solitary mastocytoma. Arch Dermatol. 2004 Oct;140(10):1275–1280. doi: 10.1001/archderm.140.10.1275-e. [DOI] [PubMed] [Google Scholar]
- Finger Florian, Rossaak Melissa, Umstaetter Richard, Reulbach Udo, Pitto Rocco. Skin infections of the limbs of Polynesian children. N Z Med J. 2004 Apr 23;117(1192):U847–U847. [PubMed] [Google Scholar]
- Friedland I. R., du Plessis J., Cilliers A. Cardiac complications in children with Staphylococcus aureus bacteremia. J Pediatr. 1995 Nov;127(5):746–748. doi: 10.1016/s0022-3476(95)70166-4. [DOI] [PubMed] [Google Scholar]
- Grant C. C., Pati A., Tan D., Vogel S., Aickin R., Scragg R. Ethnic comparisons of disease severity in children hospitalized with pneumonia in New Zealand. J Paediatr Child Health. 2001 Feb;37(1):32–37. doi: 10.1046/j.1440-1754.2001.00583.x. [DOI] [PubMed] [Google Scholar]
- Grant C. C., Scragg R., Tan D., Pati A., Aickin R., Yee R. L. Hospitalization for pneumonia in children in Auckland, New Zealand. J Paediatr Child Health. 1998 Aug;34(4):355–359. doi: 10.1046/j.1440-1754.1998.00237.x. [DOI] [PubMed] [Google Scholar]
- Hieber J. P., Nelson A. J., McCracken G. H., Jr Acute disseminated staphylococcal disease in childhood. Am J Dis Child. 1977 Feb;131(2):181–185. doi: 10.1001/archpedi.1977.02120150063012. [DOI] [PubMed] [Google Scholar]
- Hill P. C., Wong C. G., Voss L. M., Taylor S. L., Pottumarthy S., Drinkovic D., Morris A. J. Prospective study of 125 cases of Staphylococcus aureus bacteremia in children in New Zealand. Pediatr Infect Dis J. 2001 Sep;20(9):868–873. doi: 10.1097/00006454-200109000-00009. [DOI] [PubMed] [Google Scholar]
- Jefferies C., Lennon D., Stewart J., Martin D. Meningococcal disease in Auckland, July 1992 - June 1994. N Z Med J. 1999 Apr 9;112(1085):115–117. [PubMed] [Google Scholar]
- Jensen A. G. Importance of focus identification in the treatment of Staphylococcus aureus bacteraemia. J Hosp Infect. 2002 Sep;52(1):29–36. doi: 10.1053/jhin.2002.1270. [DOI] [PubMed] [Google Scholar]
- Jensen Allan G., Wachmann Carsten H., Espersen Frank, Scheibel Jens, Skinhøj Peter, Frimodt-Møller Niels. Treatment and outcome of Staphylococcus aureus bacteremia: a prospective study of 278 cases. Arch Intern Med. 2002 Jan 14;162(1):25–32. doi: 10.1001/archinte.162.1.25. [DOI] [PubMed] [Google Scholar]
- Kettelhut B. V., Metcalfe D. D. Pediatric mastocytosis. Ann Allergy. 1994 Sep;73(3):197–207. [PubMed] [Google Scholar]
- Ladhani S., Konana O. S., Mwarumba S., English M. C. Bacteraemia due to Staphylococcus aureus. Arch Dis Child. 2004 Jun;89(6):568–571. doi: 10.1136/adc.2003.026781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li J. S., Sexton D. J., Mick N., Nettles R., Fowler V. G., Jr, Ryan T., Bashore T., Corey G. R. Proposed modifications to the Duke criteria for the diagnosis of infective endocarditis. Clin Infect Dis. 2000 Apr 3;30(4):633–638. doi: 10.1086/313753. [DOI] [PubMed] [Google Scholar]
- Munro C. S., Farr P. M. Solitary mastocytoma causing recurrent blistering in infancy. Arch Dis Child. 1992 Aug;67(8):1038–1039. doi: 10.1136/adc.67.8.1038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mylonakis E., Calderwood S. B. Infective endocarditis in adults. N Engl J Med. 2001 Nov 1;345(18):1318–1330. doi: 10.1056/NEJMra010082. [DOI] [PubMed] [Google Scholar]
- Pearson G. A., Stickley J., Shann F. Calibration of the paediatric index of mortality in UK paediatric intensive care units. Arch Dis Child. 2001 Feb;84(2):125–128. doi: 10.1136/adc.84.2.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raja Lope R. J., Goldstein A. R., Gray J. W. Delayed disseminated Staphylococcus aureus infection following chickenpox. J Paediatr Child Health. 2004 May-Jun;40(5-6):320–321. doi: 10.1111/j.1440-1754.2004.00373.x. [DOI] [PubMed] [Google Scholar]
- Shann F. Are we doing a good job: PRISM, PIM and all that. Intensive Care Med. 2002 Jan 12;28(2):105–107. doi: 10.1007/s00134-001-1186-1. [DOI] [PubMed] [Google Scholar]
- Shulman S. T., Ayoub E. M. Severe staphylococcal sepsis in adolescents. Pediatrics. 1976 Jul;58(1):59–66. [PubMed] [Google Scholar]
- Slater Anthony, Shann Frank, Pearson Gale, Paediatric Index of Mortality (PIM) Study Group PIM2: a revised version of the Paediatric Index of Mortality. Intensive Care Med. 2003 Jan 23;29(2):278–285. doi: 10.1007/s00134-002-1601-2. [DOI] [PubMed] [Google Scholar]