Abstract
Background: Better language outcomes are reported for preschool children with hearing impairment (HI) diagnosed very early, irrespective of severity. However, population studies of older children are required to substantiate longer term benefits of early detection.
Aims: To study impact of age of diagnosis and severity of HI in a population cohort of 7–8 year old children.
Methods: Eighty eight 7–8 year old children born in Victoria, who were (a) fitted with hearing aids for congenital HI by 4.5 years and (b) did not have intellectual or major physical disability were studied. Main outcome measures were Clinical Evaluation of Language Fundamentals (CELF) and Peabody Picture Vocabulary Test (PPVT). Predictors were pure tone average (0.5, 1, 2 kHz) in better ear at diagnosis and age at diagnosis. Marginal (adjusted) means were estimated with general linear models.
Results: Response rate was 67% (n = 89; 53 boys). Mean age at diagnosis was 21.6 months (SD 14.4); 21% had mild, 34% moderate, 21% severe, and 24% profound HI; mean non-verbal IQ was 104.6 (SD 16.7). Mean total CELF score was 76.7 (SD 21.4) and mean PPVT score 78.1 (SD 18.1). Age of diagnosis, adjusted for severity and IQ, did not contribute to language scores. In contrast, adjusted mean CELF and PPVT language scores fell sequentially with increasing severity of HI.
Conclusions: More severe HI, but not later diagnosis, was strongly related to poorer language outcomes at 7–8 years. Further systematic study is needed to understand why children with hearing impairment have good or poor outcomes.
Full Text
The Full Text of this article is available as a PDF (95.6 KB).
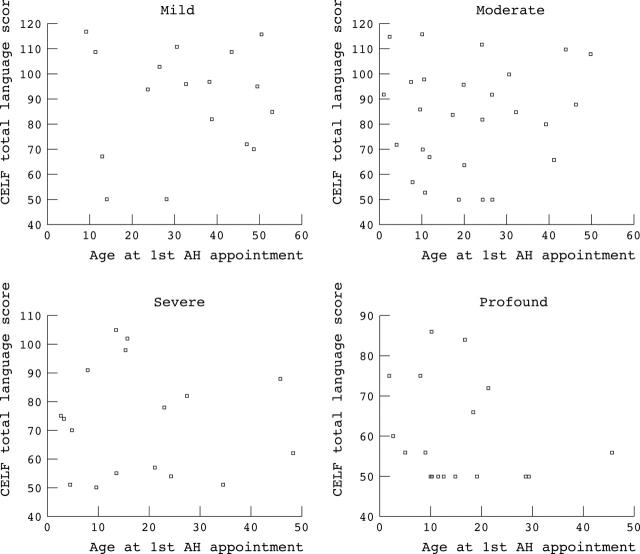
Figure 1.
Participant flowchart.
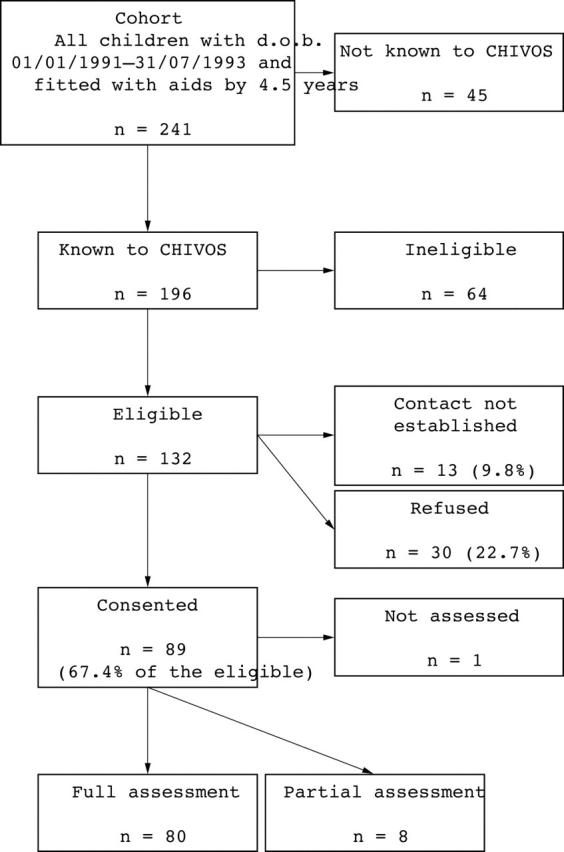
Figure 2.
Scatterplots showing CELF score against age at diagnosis, stratified by severity of hearing impairment.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Blamey Peter, Sarant Julia. Speech perception and language criteria for paediatric cochlear implant candidature. Audiol Neurootol. 2002 Mar-Apr;7(2):114–121. doi: 10.1159/000057659. [DOI] [PubMed] [Google Scholar]
- Grandori F., Lutman M. E. European Consensus Statement on Neonatal Hearing Screening. Finalised at the European Consensus Development Conference on Neonatal Hearing Screening, 15-16 May 1998, Milan. Int J Pediatr Otorhinolaryngol. 1998 Aug 1;44(3):309–310. [PubMed] [Google Scholar]
- Hammes Dianne M., Novak Michael A., Rotz Lee Ann, Willis Mary, Edmondson Danielle M., Thomas Jean F. Early identification and cochlear implantation: critical factors for spoken language development. Ann Otol Rhinol Laryngol Suppl. 2002 May;189:74–78. doi: 10.1177/00034894021110s516. [DOI] [PubMed] [Google Scholar]
- Markides A. Age at fitting of hearing aids and speech intelligibility. Br J Audiol. 1986 May;20(2):165–167. doi: 10.3109/03005368609079011. [DOI] [PubMed] [Google Scholar]
- Ramkalawan T. W., Davis A. C. The effects of hearing loss and age of intervention on some language metrics in young hearing-impaired children. Br J Audiol. 1992 Apr;26(2):97–107. doi: 10.3109/03005369209077877. [DOI] [PubMed] [Google Scholar]
- Robertson C., Aldridge S., Jarman F., Saunders K., Poulakis Z., Oberklaid F. Late diagnosis of congenital sensorineural hearing impairment: why are detection methods failing? Arch Dis Child. 1995 Jan;72(1):11–15. doi: 10.1136/adc.72.1.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinshaw H. M. Early intervention for hearing impairment: differences in the timing of communicative and linguistic development. Br J Audiol. 1995 Dec;29(6):315–334. doi: 10.3109/03005369509076750. [DOI] [PubMed] [Google Scholar]
- Russ Shirley A., Poulakis Zeffie, Barker Melinda, Wake Melissa, Rickards Field, Saunders Kerryn, Oberklaid Frank. Epidemiology of congenital hearing loss in Victoria, Australia. Int J Audiol. 2003 Oct;42(7):385–390. doi: 10.3109/14992020309080047. [DOI] [PubMed] [Google Scholar]
- Thompson D. C., McPhillips H., Davis R. L., Lieu T. L., Homer C. J., Helfand M. Universal newborn hearing screening: summary of evidence. JAMA. 2001 Oct 24;286(16):2000–2010. doi: 10.1001/jama.286.16.2000. [DOI] [PubMed] [Google Scholar]
- Ward S. An investigation into the effectiveness of an early intervention method for delayed language development in young children. Int J Lang Commun Disord. 1999 Jul-Sep;34(3):243–264. doi: 10.1080/136828299247405. [DOI] [PubMed] [Google Scholar]
- Yoshinaga-Itano C., Sedey A. L., Coulter D. K., Mehl A. L. Language of early- and later-identified children with hearing loss. Pediatrics. 1998 Nov;102(5):1161–1171. doi: 10.1542/peds.102.5.1161. [DOI] [PubMed] [Google Scholar]