Abstract
Aims: To describe and quantify impairment in an outpatient population of children with chronic pain of unknown origin (UCP).
Methods: A total of 149 children who presented with pain of at least three months' duration and without a satisfactory explanation at presentation were studied. Number of somatic complaints (Children's Somatisation Inventory, CSI), pain intensity (VAS, 0–10 cm), functional disability (Child Health Questionnaire (CHQ-CF) and clinical history), and general health perceptions (CHQ) were determined.
Results: Mean age of the children was 11.8 years; 73% were girls. Overall, 72% suffered impairment in sports activities, 51% reported absence from school, 40% experienced limitations in social functioning, and 34% had problems with sleeping. Mean number of somatic symptoms differed significantly between boys (8.4) and girls (10.7). The CHQ-CF scores for physical functioning, role/social functioning, and general health perceptions were 76.4, 70.7, and 57.5, respectively, indicating substantial impairment on all domains. The mean pain intensity was 4.7 for current and 7.1 for worst pain. Children solely evaluated by a general practitioner prior to referral reported less, though still substantial, impairment. Low general health perceptions, impaired role/social functioning, high pain intensity, and having headache or musculoskeletal pain were independent predictors of having significant impairment.
Conclusions: Referred children with UCP show substantial impairment on multiple domains in daily life.
Full Text
The Full Text of this article is available as a PDF (92.3 KB).
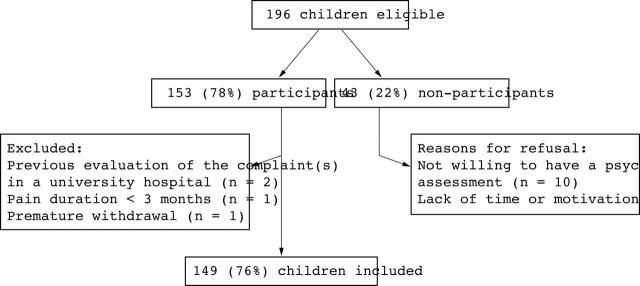
Figure 1.
Flowchart inclusion procedure.
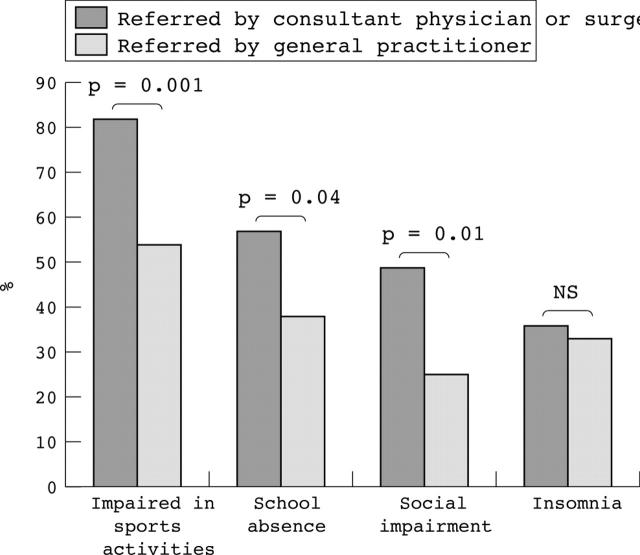
Figure 2.
Impairments in daily life. The x-axis represents four domains of possible impairment: impairment in sports activities, absence from school, social impairment, and insomnia. The y-axis represents the proportion of children affected, subdivided by referral status: referred by the general practitioner (GP group) or referred by a consultant physician or surgeon (C group).
Figure 3.
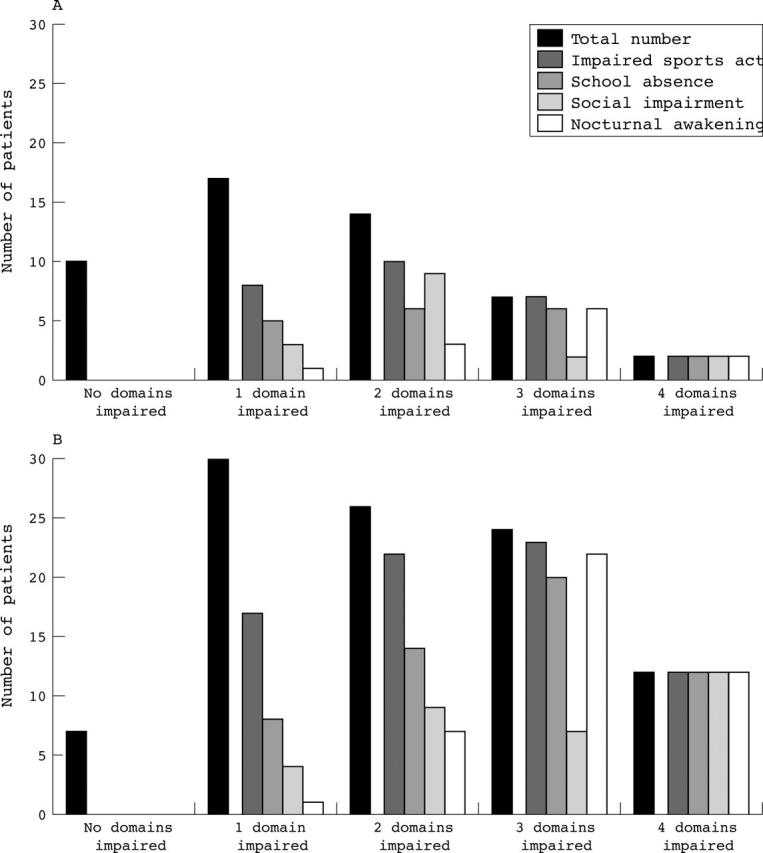
Number of impaired domains. The x-axis represents the number of impaired domains, subdivided by the relative contribution of the four domains counted: impairment in sports activities, absence from school, social impairment, and nocturnal awakening. The y-axis represents the number of children affected. (A) Data for children referred by a general practitioner (GP group, n = 50). (B) Data for children referred by a consultant physician or surgeon (C group, n = 99).
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Abu-Arefeh I., Russell G. Prevalence of headache and migraine in schoolchildren. BMJ. 1994 Sep 24;309(6957):765–769. doi: 10.1136/bmj.309.6957.765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abu-Saad H. H., Pool H., Tulkens B. Further validity testing of the Abu-Saad Paediatric Pain Assessment Tool. J Adv Nurs. 1994 Jun;19(6):1063–1071. doi: 10.1111/j.1365-2648.1994.tb01189.x. [DOI] [PubMed] [Google Scholar]
- Anderson H. R., Bailey P. A., Cooper J. S., Palmer J. C., West S. Morbidity and school absence caused by asthma and wheezing illness. Arch Dis Child. 1983 Oct;58(10):777–784. doi: 10.1136/adc.58.10.777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Apley J. The child with recurrent abdominal pain. Pediatr Clin North Am. 1967 Feb;14(1):63–72. doi: 10.1016/s0031-3955(16)31943-5. [DOI] [PubMed] [Google Scholar]
- Aronson K. R., Barrett L. F., Quigley K. S. Feeling your body or feeling badly: evidence for the limited validity of the Somatosensory Amplification Scale as an index of somatic sensitivity. J Psychosom Res. 2001 Jul;51(1):387–394. doi: 10.1016/s0022-3999(01)00216-1. [DOI] [PubMed] [Google Scholar]
- Campo John V., Comer Diane M., Jansen-Mcwilliams Linda, Gardner William, Kelleher Kelly J. Recurrent pain, emotional distress, and health service use in childhood. J Pediatr. 2002 Jul;141(1):76–83. doi: 10.1067/mpd.2002.125491. [DOI] [PubMed] [Google Scholar]
- Chalder T., Power M. J., Wessely S. Chronic fatigue in the community: 'a question of attribution'. Psychol Med. 1996 Jul;26(4):791–800. doi: 10.1017/s0033291700037818. [DOI] [PubMed] [Google Scholar]
- Delamothe T., Smith R. PubMed Central: creating an Aladdin's cave of ideas. BMJ. 2001 Jan 6;322(7277):1–2. doi: 10.1136/bmj.322.7277.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flatø B., Aasland A., Vandvik I. H., Førre O. Outcome and predictive factors in children with chronic idiopathic musculoskeletal pain. Clin Exp Rheumatol. 1997 Sep-Oct;15(5):569–577. [PubMed] [Google Scholar]
- Garralda M. E., Bowman F. M., Mandalia S. Children with psychiatric disorders who are frequent attenders to primary care. Eur Child Adolesc Psychiatry. 1999 Mar;8(1):34–44. doi: 10.1007/s007870050081. [DOI] [PubMed] [Google Scholar]
- Gladstein J., Holden E. W. Chronic daily headache in children and adolescents: a 2-year prospective study. Headache. 1996 Jun;36(6):349–351. doi: 10.1046/j.1526-4610.1996.3606349.x. [DOI] [PubMed] [Google Scholar]
- Holden E. W., Gladstein J., Trulsen M., Wall B. Chronic daily headache in children and adolescents. Headache. 1994 Oct;34(9):508–514. doi: 10.1111/j.1526-4610.1994.hed3409508.x. [DOI] [PubMed] [Google Scholar]
- Hotopf M., Carr S., Mayou R., Wadsworth M., Wessely S. Why do children have chronic abdominal pain, and what happens to them when they grow up? Population based cohort study. BMJ. 1998 Apr 18;316(7139):1196–1200. doi: 10.1136/bmj.316.7139.1196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hyams J. S., Burke G., Davis P. M., Rzepski B., Andrulonis P. A. Abdominal pain and irritable bowel syndrome in adolescents: a community-based study. J Pediatr. 1996 Aug;129(2):220–226. doi: 10.1016/s0022-3476(96)70246-9. [DOI] [PubMed] [Google Scholar]
- Hyams J. S., Treem W. R., Justinich C. J., Davis P., Shoup M., Burke G. Characterization of symptoms in children with recurrent abdominal pain: resemblance to irritable bowel syndrome. J Pediatr Gastroenterol Nutr. 1995 Feb;20(2):209–214. doi: 10.1097/00005176-199502000-00012. [DOI] [PubMed] [Google Scholar]
- Ipsiroglu Osman S., Fatemi Ali, Werner Irene, Paditz Ekkehart, Schwarz Bernhard. Self-reported organic and nonorganic sleep problems in schoolchildren aged 11 to 15 years in Vienna. J Adolesc Health. 2002 Nov;31(5):436–442. doi: 10.1016/s1054-139x(02)00423-8. [DOI] [PubMed] [Google Scholar]
- Kashikar-Zuck S., Goldschneider K. R., Powers S. W., Vaught M. H., Hershey A. D. Depression and functional disability in chronic pediatric pain. Clin J Pain. 2001 Dec;17(4):341–349. doi: 10.1097/00002508-200112000-00009. [DOI] [PubMed] [Google Scholar]
- Klerman L. V. School absence--a health perspective. Pediatr Clin North Am. 1988 Dec;35(6):1253–1269. doi: 10.1016/s0031-3955(16)36582-8. [DOI] [PubMed] [Google Scholar]
- Macfarlane G. J., Morris S., Hunt I. M., Benjamin S., McBeth J., Papageorgiou A. C., Silman A. J. Chronic widespread pain in the community: the influence of psychological symptoms and mental disorder on healthcare seeking behavior. J Rheumatol. 1999 Feb;26(2):413–419. [PubMed] [Google Scholar]
- Malleson P. N., Connell H., Bennett S. M., Eccleston C. Chronic musculoskeletal and other idiopathic pain syndromes. Arch Dis Child. 2001 Mar;84(3):189–192. doi: 10.1136/adc.84.3.189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGhee Julie L., Burks Frank N., Sheckels Julie L., Jarvis James N. Identifying children with chronic arthritis based on chief complaints: absence of predictive value for musculoskeletal pain as an indicator of rheumatic disease in children. Pediatrics. 2002 Aug;110(2 Pt 1):354–359. doi: 10.1542/peds.110.2.354. [DOI] [PubMed] [Google Scholar]
- Perquin C. W., Hazebroek-Kampschreur A. A., Hunfeld J. A., Bohnen A. M., van Suijlekom-Smit L. W., Passchier J., van der Wouden J. C. Pain in children and adolescents: a common experience. Pain. 2000 Jul;87(1):51–58. doi: 10.1016/S0304-3959(00)00269-4. [DOI] [PubMed] [Google Scholar]
- Perquin C. W., Hunfeld J. A., Hazebroek-Kampschreur A. A., van Suijlekom-Smit L. W., Passchier J., Koes B. W., van der Wouden J. C. Insights in the use of health care services in chronic benign pain in childhood and adolescence. Pain. 2001 Nov;94(2):205–213. doi: 10.1016/S0304-3959(01)00355-4. [DOI] [PubMed] [Google Scholar]
- Raat Hein, Bonsel Gouke J., Essink-Bot Marie Louise, Landgraf Jeanne M., Gemke Reinoud J. B. J. Reliability and validity of comprehensive health status measures in children: The Child Health Questionnaire in relation to the Health Utilities Index. J Clin Epidemiol. 2002 Jan;55(1):67–76. doi: 10.1016/s0895-4356(01)00411-5. [DOI] [PubMed] [Google Scholar]
- Reid G. J., Gilbert C. A., McGrath P. J. The Pain Coping Questionnaire: preliminary validation. Pain. 1998 May;76(1-2):83–96. doi: 10.1016/s0304-3959(98)00029-3. [DOI] [PubMed] [Google Scholar]
- Ruperto N., Ravelli A., Pistorio A., Malattia C., Cavuto S., Gado-West L., Tortorelli A., Landgraf J. M., Singh G., Martini A. Cross-cultural adaptation and psychometric evaluation of the Childhood Health Assessment Questionnaire (CHAQ) and the Child Health Questionnaire (CHQ) in 32 countries. Review of the general methodology. Clin Exp Rheumatol. 2001 Jul-Aug;19(4 Suppl 23):S1–S9. [PubMed] [Google Scholar]
- Smith M. S., Martin-Herz S. P., Womack W. M., McMahon R. J. Recurrent headache in adolescents: nonreferred versus clinic population. Headache. 1999 Oct;39(9):616–624. doi: 10.1046/j.1526-4610.1999.3909616.x. [DOI] [PubMed] [Google Scholar]
- Taimela S., Kujala U. M., Salminen J. J., Viljanen T. The prevalence of low back pain among children and adolescents. A nationwide, cohort-based questionnaire survey in Finland. Spine (Phila Pa 1976) 1997 May 15;22(10):1132–1136. doi: 10.1097/00007632-199705150-00013. [DOI] [PubMed] [Google Scholar]
- Varni J. W., Thompson K. L., Hanson V. The Varni/Thompson Pediatric Pain Questionnaire. I. Chronic musculoskeletal pain in juvenile rheumatoid arthritis. Pain. 1987 Jan;28(1):27–38. doi: 10.1016/0304-3959(87)91056-6. [DOI] [PubMed] [Google Scholar]
- Walker L. S., Garber J., Greene J. W. Somatization symptoms in pediatric abdominal pain patients: relation to chronicity of abdominal pain and parent somatization. J Abnorm Child Psychol. 1991 Aug;19(4):379–394. doi: 10.1007/BF00919084. [DOI] [PubMed] [Google Scholar]
- Waters E. B., Salmon L. A., Wake M., Wright M., Hesketh K. D. The health and well-being of adolescents: a school-based population study of the self-report Child Health Questionnaire. J Adolesc Health. 2001 Aug;29(2):140–149. doi: 10.1016/s1054-139x(01)00211-7. [DOI] [PubMed] [Google Scholar]
- Wessely S., Nimnuan C., Sharpe M. Functional somatic syndromes: one or many? Lancet. 1999 Sep 11;354(9182):936–939. doi: 10.1016/S0140-6736(98)08320-2. [DOI] [PubMed] [Google Scholar]
- Wulffraat N., van der Net J. J., Ruperto N., Kamphuis S., Prakken B. J., Ten Cate R., Van Soesbergen R. M., Van Rossum M. A., Raat H., Landgraf J. M. The Dutch version of the Childhood Health Assessment Questionnaire (CHAQ) and the Child Health Questionnaire (CHQ). Clin Exp Rheumatol. 2001 Jul-Aug;19(4 Suppl 23):S111–S115. [PubMed] [Google Scholar]