Abstract
Background: Published formulae, frequently used to predict the volume of transfused red cells required to achieve a desired rise in haemoglobin (Hb) or haematocrit (Hct), do not appear to have been validated in clinical practice.
Aims: To examine the relation between transfusion volume and the resulting rise in Hb and Hct in critically ill children.
Methods: Phase 1: Sample of 50% of children admitted during 1997; 237 of these 495 patients received at least one packed red cell transfusion; 82 children were transfused without confounding factors that could influence the Hb/Hct response to transfusion and were analysed further. Actual rise in Hb concentration or haematocrit was compared to that expected from use of existing formulae. A new formula was developed. Phase 2: In 50 children receiving a packed red cell transfusion during 2001, actual rise in Hb concentration was compared to expected rise in Hb with use of the new formula.
Results: Phase 1: Existing formulae performed poorly; median ratio of actual/predicted rise in Hb or Hct ranged from 0.61 to 0.85. Using the regression coefficients new formulae were developed for both Hb and Hct. These formulae were applicable across all age and diagnostic groups. Phase 2: Median ratio of actual/predicted rise in Hb improved to 0.95 with use of the new formula.
Conclusions: Existing formulae underestimate the volume of packed red cells required to achieve a target Hb or Hct. Adoption of the new formulae could reduce the number of transfusion episodes in PICU, cutting costs and reducing risk.
Full Text
The Full Text of this article is available as a PDF (251.3 KB).
Figure 1.
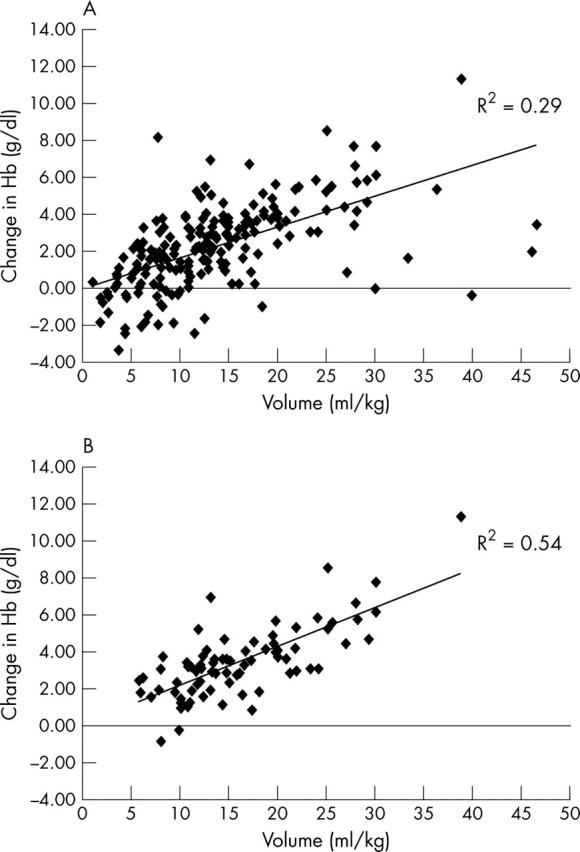
(A) Individual data for transfusion volume relative to weight (ml/kg) against the change in haemoglobin (Hb) concentration following transfusion (n = 237). (B) Individual data in those children without confounding factors that could influence the Hb response to transfusion (n = 82).
Figure 2.
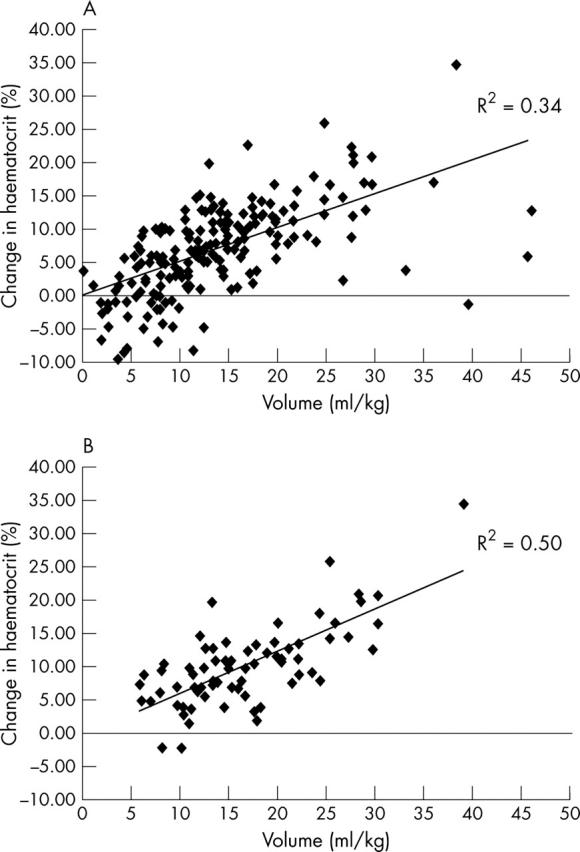
(A) Individual data for transfusion volume relative to weight (ml/kg) against the change in haematocrit (Hct) following transfusion (n = 237). (B) Individual data in those children without confounding factors that could influence the Hct response to transfusion (n = 82).
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Aladangady N., Aitchison T. C., Beckett C., Holland B. M., Kyle B. M., Wardrop C. A. J. Is it possible to predict the blood volume of a sick preterm infant? Arch Dis Child Fetal Neonatal Ed. 2004 Jul;89(4):F344–F347. doi: 10.1136/adc.2003.039008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bolton-Maggs P. H. B., Murphy M. F. Blood transfusion. Arch Dis Child. 2004 Jan;89(1):4–7. [PMC free article] [PubMed] [Google Scholar]
- Bratton Susan L., Annich Gail M. Packed red blood cell transfusions for critically ill pediatric patients: when and for what conditions? J Pediatr. 2003 Feb;142(2):95–97. doi: 10.1067/mpd.2003.77. [DOI] [PubMed] [Google Scholar]
- Freedman J. The significance of complement on the red cell surface. Transfus Med Rev. 1987 Apr;1(1):58–70. doi: 10.1016/s0887-7963(87)70006-6. [DOI] [PubMed] [Google Scholar]
- Hamasaki N., Yamamoto M. Red blood cell function and blood storage. Vox Sang. 2000;79(4):191–197. doi: 10.1159/000056729. [DOI] [PubMed] [Google Scholar]
- Hébert P. C., Wells G., Blajchman M. A., Marshall J., Martin C., Pagliarello G., Tweeddale M., Schweitzer I., Yetisir E. A multicenter, randomized, controlled clinical trial of transfusion requirements in critical care. Transfusion Requirements in Critical Care Investigators, Canadian Critical Care Trials Group. N Engl J Med. 1999 Feb 11;340(6):409–417. doi: 10.1056/NEJM199902113400601. [DOI] [PubMed] [Google Scholar]
- Jefferies L. C., Sachais B. S., Young D. S. Blood transfusion costs by diagnosis-related groups in 60 university hospitals in 1995. Transfusion. 2001 Apr;41(4):522–529. doi: 10.1046/j.1537-2995.2001.41040522.x. [DOI] [PubMed] [Google Scholar]
- Laverdière Caroline, Gauvin France, Hébert Paul C., Infante-Rivard Claire, Hume Heather, Toledano Baruch J., Guertin Marie-Claude, Lacroix Jacques, Canadian Critical Care Trials Group Survey on transfusion practices of pediatric intensivists. Pediatr Crit Care Med. 2002 Oct;3(4):335–340. doi: 10.1097/00130478-200210000-00001. [DOI] [PubMed] [Google Scholar]
- Linderkamp O., Holthausen H., Seifert J., Butenandt I., Riegel K. P. Accuracy of blood volume estimations in critically ill children using 125I-labelled albumin and 51Cr-labelled red cells. Eur J Pediatr. 1977 Jun 1;125(2):143–151. doi: 10.1007/BF00489987. [DOI] [PubMed] [Google Scholar]
- Samuels L. D. Measuring the circulating blood: how much does a child have? A description and explanation of radioactivity procedures. Clin Pediatr (Phila) 1972 Aug;11(8):479–481. doi: 10.1177/000992287201100815. [DOI] [PubMed] [Google Scholar]
- Valeri C. R. Viability and function of preserved red cells. N Engl J Med. 1971 Jan 14;284(2):81–88. doi: 10.1056/NEJM197101142840205. [DOI] [PubMed] [Google Scholar]
- Walker R. H. Mathematical calculations in transfusion medicine. Clin Lab Med. 1996 Dec;16(4):895–906. [PubMed] [Google Scholar]


