Abstract
AIMS—To identify the patent ductus arteriosus (PDA) shunt flow pattern using Doppler echocardiography; and to assess whether it could be used to predict the development of clinically significant PDA. METHODS—Premature infants weighing under 1500 g, who required mechanical ventilation, and in whom daily echocardiography could be performed from day 1 until the ductus closed, and on day 7 to confirm closure, were studied. The PDA shunt flow was identified from four Doppler patterns, and the closed pattern of a closed duct was also presented. Clinically significant PDA was diagnosed when there was colour Doppler echocardiographic evidence of left to right ductal shunt associated with at least two of the following clinical signs: heart murmur (systolic or continuous); persistent tachycardia (heart rate>160/min); hyperactive precordial pulsation; bounding pulses; and radiographic evidence of cardiomegaly or pulmonary congestion. RESULTS—Of 68 infants enrolled into this study, clincally significant PDA developed in 31. The most recordable sequence of transition change of shunt flow pattern for clinically significant PDA was: pulmonary hypertension pattern, to growing pattern, to pulsatile pattern, to closing pattern, to closed pattern. And that for non-clinically significant PDA was: pulmonary hypertension pattern, to closing pattern, to closed pattern. The growing and the pulsatile patterns were mostly documented in infants with clinically significant PDA. The first documented growing pattern to predict clinically significant PDA gave a sensitivity of 64.5% and a specificity of 81.1%; the first documented pulsatile pattern gave a sensitivity of 93.5% and a specificity of 100%. CONCLUSION—Doppler echocardiographic assessment of PDA shunt flow pattern during the first 4 days of life is useful for predicting the development of clinically significant PDA in premature infants. At that stage, the closing or closed Doppler pattern indicates that infants are not at risk of developing clinically significant PDA; the growing or pulsatile Doppler pattern indicates a continuing risk of developing clinically significant PDA. Keywords: Echocardiography; patent ductus arteriosus; Doppler flow pattern
Full Text
The Full Text of this article is available as a PDF (119.8 KB).
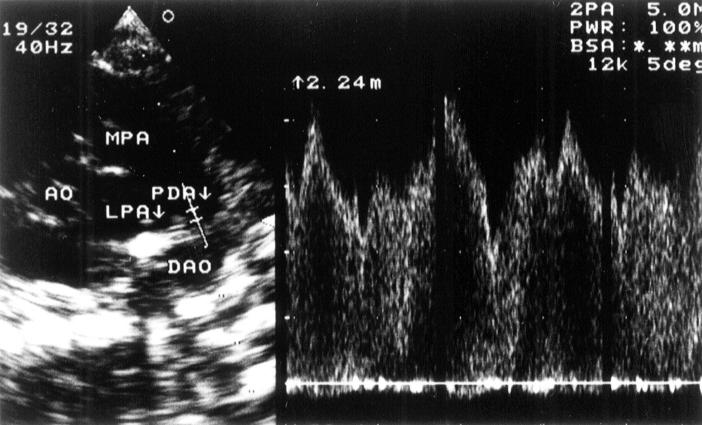
Figure 1 .
Left: high left parasternal view echocardiogram. The main pulmonary artery (MPA), patent ductus arteriosus (PDA), and descending aorta (DAO) can be seen in a contiuous arc. The origin of the left pulmonary artery (LPA) is also evident. Posterior to the DAO are the vertebral bodies. The pulsed Doppler gate is positioned at the pulmonary end of the PDA. Right: resultant Doppler profile of the the PDA shunt flow.
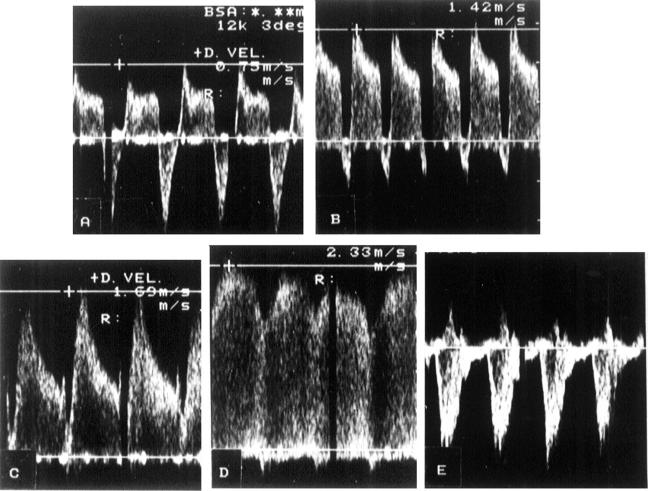
Figure 2 .
Four Doppler flow patterns and the contrasting closed pattern. A: pulmonary hypertension pattern; B: growing pattern; C: pulsatile pattern; D: closing pattern; E: closed pattern.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Brown E. R. Increased risk of bronchopulmonary dysplasia in infants with patent ductus arteriosus. J Pediatr. 1979 Nov;95(5 Pt 2):865–866. doi: 10.1016/s0022-3476(79)80454-0. [DOI] [PubMed] [Google Scholar]
- Clyman R. I. Recommendations for the postnatal use of indomethacin: an analysis of four separate treatment strategies. J Pediatr. 1996 May;128(5 Pt 1):601–607. doi: 10.1016/s0022-3476(96)80123-5. [DOI] [PubMed] [Google Scholar]
- Dudell G. G., Gersony W. M. Patent ductus arteriosus in neonates with severe respiratory disease. J Pediatr. 1984 Jun;104(6):915–920. doi: 10.1016/s0022-3476(84)80499-0. [DOI] [PubMed] [Google Scholar]
- Evans N., Iyer P. Change in blood pressure after treatment of patent ductus arteriosus with indomethacin. Arch Dis Child. 1993 May;68(5 Spec No):584–587. doi: 10.1136/adc.68.5_spec_no.584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans N., Moorcraft J. Effect of patency of the ductus arteriosus on blood pressure in very preterm infants. Arch Dis Child. 1992 Oct;67(10 Spec No):1169–1173. doi: 10.1136/adc.67.10_spec_no.1169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gentile R., Stevenson G., Dooley T., Franklin D., Kawabori I., Pearlman A. Pulsed Doppler echocardiographic determination of time of ductal closure in normal newborn infants. J Pediatr. 1981 Mar;98(3):443–448. doi: 10.1016/s0022-3476(81)80719-6. [DOI] [PubMed] [Google Scholar]
- Houston A. B., Gnanapragasam J. P., Lim M. K., Doig W. B., Coleman E. N. Doppler ultrasound and the silent ductus arteriosus. Br Heart J. 1991 Feb;65(2):97–99. doi: 10.1136/hrt.65.2.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huhta J. C., Cohen M., Gutgesell H. P. Patency of the ductus arteriosus in normal neonates: two-dimensional echocardiography versus Doppler assessment. J Am Coll Cardiol. 1984 Sep;4(3):561–564. doi: 10.1016/s0735-1097(84)80102-3. [DOI] [PubMed] [Google Scholar]
- Huhta J. C., Gutgesell H. P., Latson L. A., Huffines F. D. Two-dimensional echocardiographic assessment of the aorta in infants and children with congenital heart disease. Circulation. 1984 Sep;70(3):417–424. doi: 10.1161/01.cir.70.3.417. [DOI] [PubMed] [Google Scholar]
- Kluckow M., Evans N. Early echocardiographic prediction of symptomatic patent ductus arteriosus in preterm infants undergoing mechanical ventilation. J Pediatr. 1995 Nov;127(5):774–779. doi: 10.1016/s0022-3476(95)70172-9. [DOI] [PubMed] [Google Scholar]
- Käpä P., Seppänen M., Kero P., Saraste M. Pulmonary hemodynamics after synthetic surfactant replacement in neonatal respiratory distress syndrome. J Pediatr. 1993 Jul;123(1):115–119. doi: 10.1016/s0022-3476(05)81553-7. [DOI] [PubMed] [Google Scholar]
- Lipman B., Serwer G. A., Brazy J. E. Abnormal cerebral hemodynamics in preterm infants with patent ductus arteriosus. Pediatrics. 1982 Jun;69(6):778–781. [PubMed] [Google Scholar]
- Martin C. G., Snider A. R., Katz S. M., Peabody J. L., Brady J. P. Abnormal cerebral blood flow patterns in preterm infants with a large patent ductus arteriosus. J Pediatr. 1982 Oct;101(4):587–593. doi: 10.1016/s0022-3476(82)80715-4. [DOI] [PubMed] [Google Scholar]
- Mellander M., Larsson L. E., Ekström-Jodal B., Sabel K. G. Prediction of symptomatic patent ductus arteriosus in preterm infants using Doppler and M-mode echocardiography. Acta Paediatr Scand. 1987 Jul;76(4):553–559. doi: 10.1111/j.1651-2227.1987.tb10520.x. [DOI] [PubMed] [Google Scholar]
- Ramsay J. M., Murphy D. J., Jr, Vick G. W., 3rd, Courtney J. T., Garcia-Prats J. A., Huhta J. C. Response of the patent ductus arteriosus to indomethacin treatment. Am J Dis Child. 1987 Mar;141(3):294–297. doi: 10.1001/archpedi.1987.04460030072028. [DOI] [PubMed] [Google Scholar]
- Reller M. D., Buffkin D. C., Colasurdo M. A., Rice M. J., McDonald R. W. Ductal patency in neonates with respiratory distress syndrome. A randomized surfactant trial. Am J Dis Child. 1991 Sep;145(9):1017–1020. doi: 10.1001/archpedi.1991.02160090069025. [DOI] [PubMed] [Google Scholar]
- Reller M. D., Rice M. J., McDonald R. W. Review of studies evaluating ductal patency in the premature infant. J Pediatr. 1993 Jun;122(6):S59–S62. doi: 10.1016/s0022-3476(09)90044-0. [DOI] [PubMed] [Google Scholar]
- Ryder R. W., Shelton J. D., Guinan M. E. Necrotizing enterocolitis: a prospective multicenter investigation. Am J Epidemiol. 1980 Jul;112(1):113–123. doi: 10.1093/oxfordjournals.aje.a112960. [DOI] [PubMed] [Google Scholar]
- Shimada S., Kasai T., Konishi M., Fujiwara T. Effects of patent ductus arteriosus on left ventricular output and organ blood flows in preterm infants with respiratory distress syndrome treated with surfactant. J Pediatr. 1994 Aug;125(2):270–277. doi: 10.1016/s0022-3476(94)70210-1. [DOI] [PubMed] [Google Scholar]
- Shiraishi H., Yanagisawa M. Bidirectional flow through the ductus arteriosus in normal newborns: evaluation by Doppler color flow imaging. Pediatr Cardiol. 1991 Oct;12(4):201–205. doi: 10.1007/BF02310566. [DOI] [PubMed] [Google Scholar]
- Silverman N. H., Lewis A. B., Heymann M. A., Rudolph A. M. Echocardiographic assessment of ductus arteriosus shunt in premature infants. Circulation. 1974 Oct;50(4):821–825. doi: 10.1161/01.cir.50.4.821. [DOI] [PubMed] [Google Scholar]
- Smallhorn J. F., Gow R., Olley P. M., Freedom R. M., Swyer P. R., Perlman M., Rowe R. D. Combined noninvasive assessment of the patent ductus arteriosus in the preterm infant before and after indomethacin treatment. Am J Cardiol. 1984 Dec 1;54(10):1300–1304. doi: 10.1016/s0002-9149(84)80086-7. [DOI] [PubMed] [Google Scholar]
- Wilson N., Dickinson D. F., Goldberg S. J., Scott O. Pulmonary artery velocity patterns in ductus arteriosus. Br Heart J. 1984 Oct;52(4):462–464. doi: 10.1136/hrt.52.4.462. [DOI] [PMC free article] [PubMed] [Google Scholar]