Abstract
AIM—To assess ultrasonographically the flow pattern and the time of postnatal closure of ductus venosus related to the other fetal shunts. METHODS—Fifty healthy, term neonates were studied from day 1 up to day 18 using a VingMed CFM 800A ultrasound scanner. RESULTS—Ductus arteriosus was closed in 94% of the infants before day 3. Ductus venosus, however, was closed in only 12% at the same time, in 76% before day 7, and in all infants before day 18. A closed ductus venosus or ductus arteriosus did not show signs of reopening. Pulsed and colour Doppler flow could be detected across the foramen ovale in all infants during the sequential investigation. At day 1, when the pulmonary vascular resistance was still high, a reversed Doppler flow velocity signal was seen in ductus venosus in 10 infants (20%) and a bidirectional flow in ductus arteriosus in 26 (52%). Closure of the ductus venosus was not significantly correlated with closure of the ductus arteriosus nor related to sex nor weight loss. CONCLUSIONS—The time of closure of the ductus venosus evaluated by ultrasonography is much later than that of the ductus arteriosus. The flow pattern in ductus venosus reflects the portocaval pressure gradient and the pressure on the right side of the heart and in the pulmonary arteries. Both the flow pattern in the ductus venosus as well as that in the ductus arteriosus may be an indication of compromised neonatal haemodynamics. Keywords: ductus venosus; ductus arteriosus; foramen ovale; Doppler echocardiography
Full Text
The Full Text of this article is available as a PDF (137.6 KB).
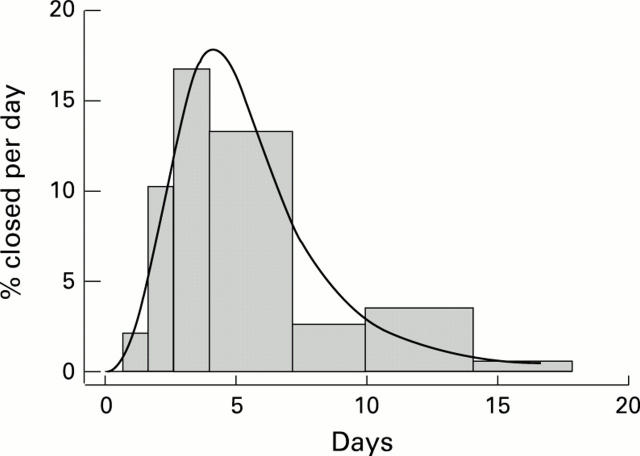
Figure 1 .
Distribution of closing times for ductus venosus. The height of each bar gives the percentage closure per day during the corresponding time interval. The curve represents the log logistic distribution fitted to the observations.
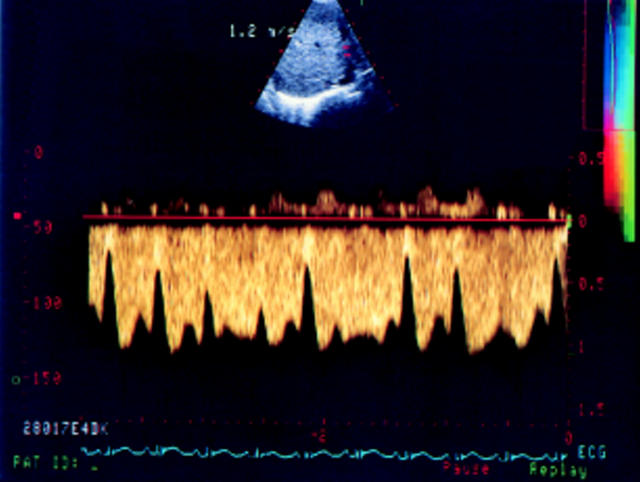
Figure 2 .
Doppler signals in ductus venosus from the portal sinus to the inferior caval vein at the inlet of the right atrium.
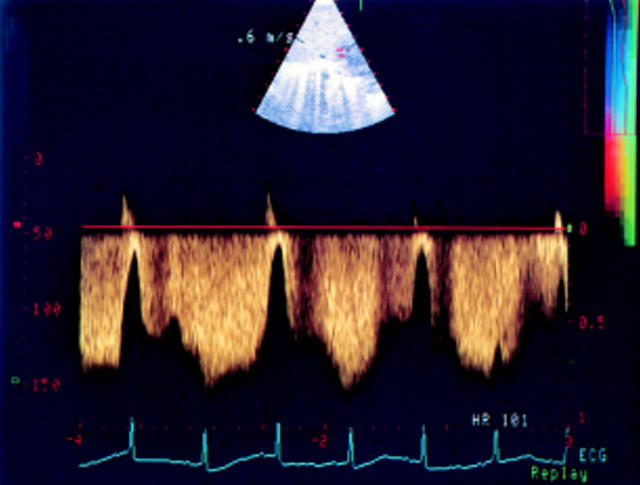
Figure 3 .
Cephalic biphasic waveform signals in the ductus venosus. The low velocity pattern shows a peak during ventricular systole and diastole, and a nadir during atrial systole.
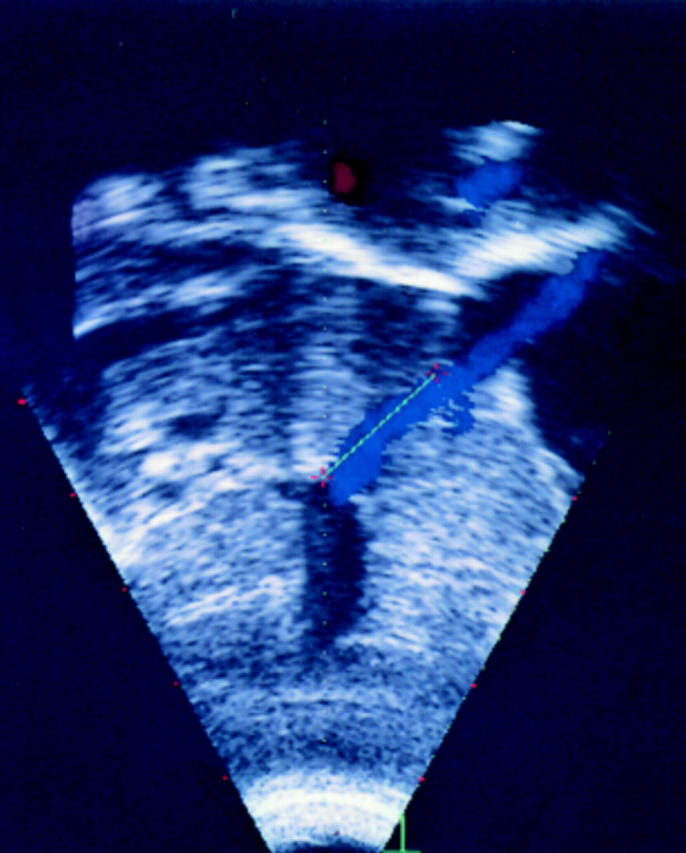
Figure 4 .
During the first day of life, a short reversed velocity flow signal during atrial systole in ductus venosus was observed in 10 infants.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Agata Y., Hiraishi S., Misawa H., Hirota H., Nowatari M., Hiura K., Fujino N., Oguchi K., Horiguchi Y. Regional blood flow distribution and left ventricular output during early neonatal life: a quantitative ultrasonographic assessment. Pediatr Res. 1994 Dec;36(6):805–810. doi: 10.1203/00006450-199412000-00022. [DOI] [PubMed] [Google Scholar]
- Alenick D. S., Holzman I. R., Ritter S. B. The neonatal transitional circulation: a combined noninvasive assessment. Echocardiography. 1992 Jan;9(1):29–37. doi: 10.1111/j.1540-8175.1992.tb00436.x. [DOI] [PubMed] [Google Scholar]
- Behrman R. E., Lees M. H., Peterson E. N., De Lannoy C. W., Seeds A. E. Distribution of the circulation in the normal and asphyxiated fetal primate. Am J Obstet Gynecol. 1970 Nov 15;108(6):956–969. doi: 10.1016/0002-9378(70)90341-8. [DOI] [PubMed] [Google Scholar]
- Berger M., Haimowitz A., Van Tosh A., Berdoff R. L., Goldberg E. Quantitative assessment of pulmonary hypertension in patients with tricuspid regurgitation using continuous wave Doppler ultrasound. J Am Coll Cardiol. 1985 Aug;6(2):359–365. doi: 10.1016/s0735-1097(85)80172-8. [DOI] [PubMed] [Google Scholar]
- Chan K. L., Currie P. J., Seward J. B., Hagler D. J., Mair D. D., Tajik A. J. Comparison of three Doppler ultrasound methods in the prediction of pulmonary artery pressure. J Am Coll Cardiol. 1987 Mar;9(3):549–554. doi: 10.1016/s0735-1097(87)80047-5. [DOI] [PubMed] [Google Scholar]
- Currie P. J., Seward J. B., Chan K. L., Fyfe D. A., Hagler D. J., Mair D. D., Reeder G. S., Nishimura R. A., Tajik A. J. Continuous wave Doppler determination of right ventricular pressure: a simultaneous Doppler-catheterization study in 127 patients. J Am Coll Cardiol. 1985 Oct;6(4):750–756. doi: 10.1016/s0735-1097(85)80477-0. [DOI] [PubMed] [Google Scholar]
- Evans N. J., Archer L. N. Postnatal circulatory adaptation in healthy term and preterm neonates. Arch Dis Child. 1990 Jan;65(1 Spec No):24–26. doi: 10.1136/adc.65.1_spec_no.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gentile R., Stevenson G., Dooley T., Franklin D., Kawabori I., Pearlman A. Pulsed Doppler echocardiographic determination of time of ductal closure in normal newborn infants. J Pediatr. 1981 Mar;98(3):443–448. doi: 10.1016/s0022-3476(81)80719-6. [DOI] [PubMed] [Google Scholar]
- HIRVONEN L., PELTONEN T., RUOKOLA M. Angiocardiography of the newborn with contrast injected into the umbilical vein. Ann Paediatr Fenn. 1961;7:124–130. [PubMed] [Google Scholar]
- Hecher K., Snijders R., Campbell S., Nicolaides K. Fetal venous, intracardiac, and arterial blood flow measurements in intrauterine growth retardation: relationship with fetal blood gases. Am J Obstet Gynecol. 1995 Jul;173(1):10–15. doi: 10.1016/0002-9378(95)90161-2. [DOI] [PubMed] [Google Scholar]
- Hiraishi S., Agata Y., Saito K., Oguchi K., Misawa H., Fujino N., Horiguchi Y., Yashiro K. Interatrial shunt flow profiles in newborn infants: a colour flow and pulsed Doppler echocardiographic study. Br Heart J. 1991 Jan;65(1):41–45. doi: 10.1136/hrt.65.1.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hiraishi S., Misawa H., Oguchi K., Kadoi N., Saito K., Fujino N., Hojo M., Horiguchi Y., Yashiro K. Two-dimensional Doppler echocardiographic assessment of closure of the ductus arteriosus in normal newborn infants. J Pediatr. 1987 Nov;111(5):755–760. doi: 10.1016/s0022-3476(87)80263-9. [DOI] [PubMed] [Google Scholar]
- Kiserud T., Eik-Nes S. H., Blaas H. G., Hellevik L. R. Foramen ovale: an ultrasonographic study of its relation to the inferior vena cava, ductus venosus and hepatic veins. Ultrasound Obstet Gynecol. 1992 Nov 1;2(6):389–396. doi: 10.1046/j.1469-0705.1992.02060389.x. [DOI] [PubMed] [Google Scholar]
- Kiserud T., Eik-Nes S. H., Blaas H. G., Hellevik L. R., Simensen B. Ductus venosus blood velocity and the umbilical circulation in the seriously growth-retarded fetus. Ultrasound Obstet Gynecol. 1994 Mar 1;4(2):109–114. doi: 10.1046/j.1469-0705.1994.04020109.x. [DOI] [PubMed] [Google Scholar]
- Kiserud T., Eik-Nes S. H., Blaas H. G., Hellevik L. R. Ultrasonographic velocimetry of the fetal ductus venosus. Lancet. 1991 Dec 7;338(8780):1412–1414. doi: 10.1016/0140-6736(91)92720-m. [DOI] [PubMed] [Google Scholar]
- Lind J. Eleventh Edgar Mannheimer Lecture. Human fetal and neonatal circulation. Some structural and functional aspects. Eur J Cardiol. 1977 May;5(3):265–281. [PubMed] [Google Scholar]
- Loberant N., Barak M., Gaitini D., Herskovits M., Ben-Elisha M., Roguin N. Closure of the ductus venosus in neonates: findings on real-time gray-scale, color-flow Doppler, and duplex Doppler sonography. AJR Am J Roentgenol. 1992 Nov;159(5):1083–1085. doi: 10.2214/ajr.159.5.1414780. [DOI] [PubMed] [Google Scholar]
- Musewe N. N., Poppe D., Smallhorn J. F., Hellman J., Whyte H., Smith B., Freedom R. M. Doppler echocardiographic measurement of pulmonary artery pressure from ductal Doppler velocities in the newborn. J Am Coll Cardiol. 1990 Feb;15(2):446–456. doi: 10.1016/s0735-1097(10)80076-2. [DOI] [PubMed] [Google Scholar]
- Oepkes D., Vandenbussche F. P., Van Bel F., Kanhai H. H. Fetal ductus venosus blood flow velocities before and after transfusion in red-cell alloimmunized pregnancies. Obstet Gynecol. 1993 Aug;82(2):237–241. [PubMed] [Google Scholar]
- Rudolph A. M. Distribution and regulation of blood flow in the fetal and neonatal lamb. Circ Res. 1985 Dec;57(6):811–821. doi: 10.1161/01.res.57.6.811. [DOI] [PubMed] [Google Scholar]
- Walther F. J., Benders M. J., Leighton J. O. Early changes in the neonatal circulatory transition. J Pediatr. 1993 Oct;123(4):625–632. doi: 10.1016/s0022-3476(05)80966-7. [DOI] [PubMed] [Google Scholar]