Abstract
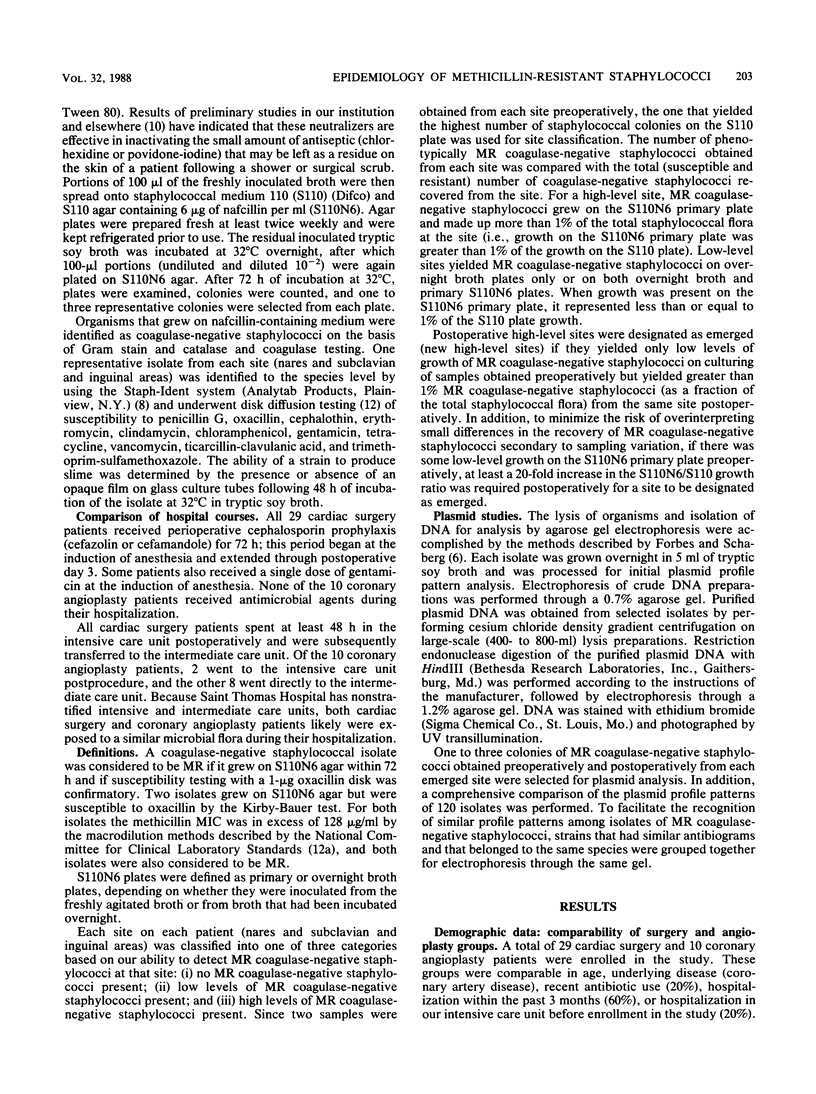
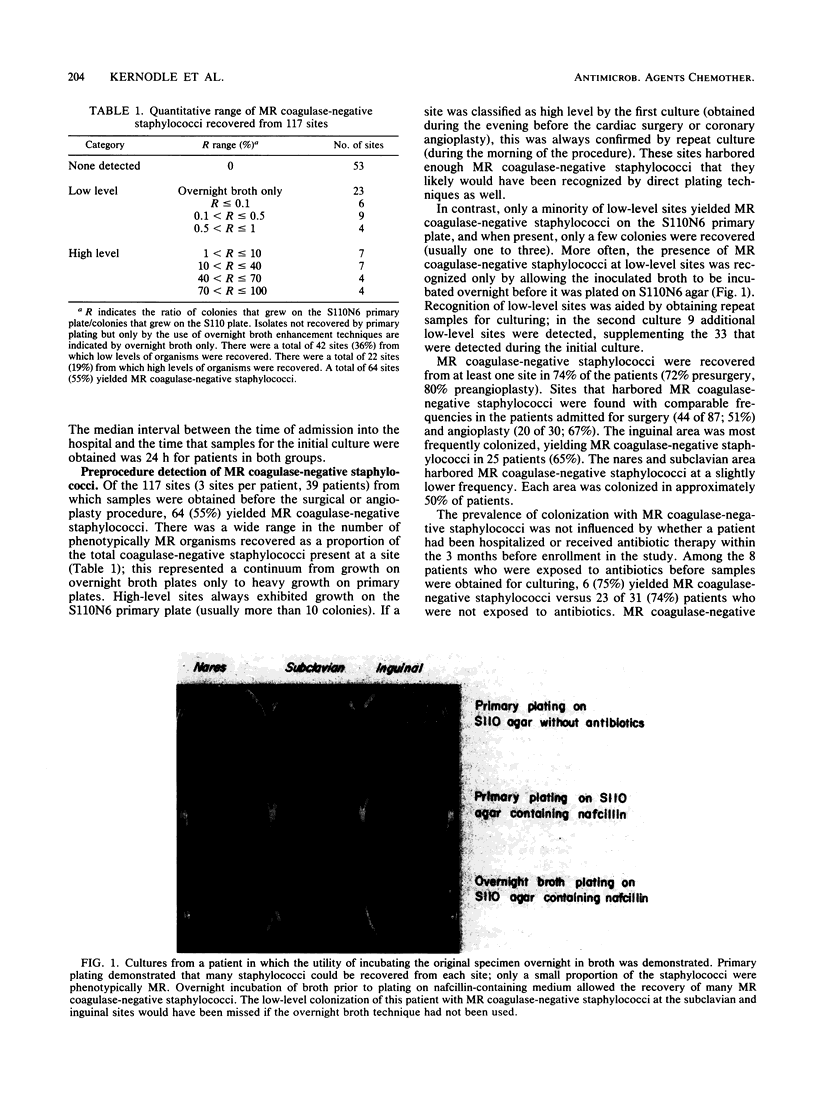
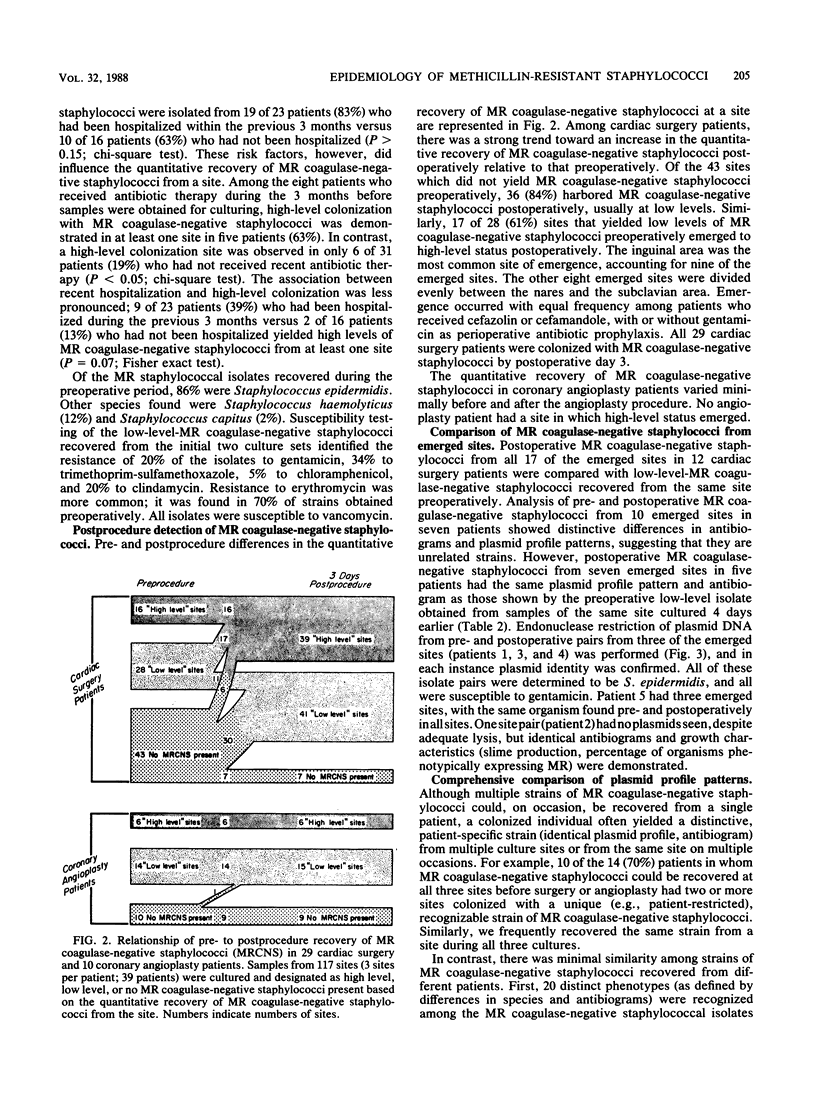
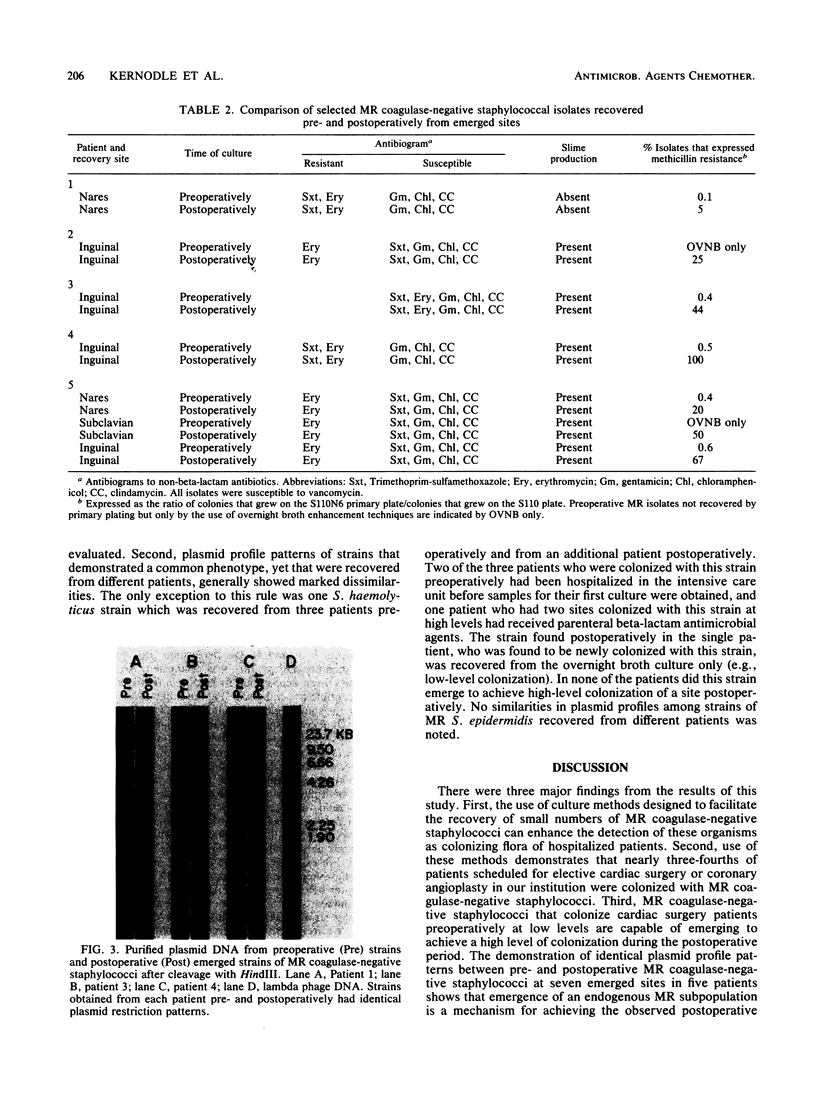
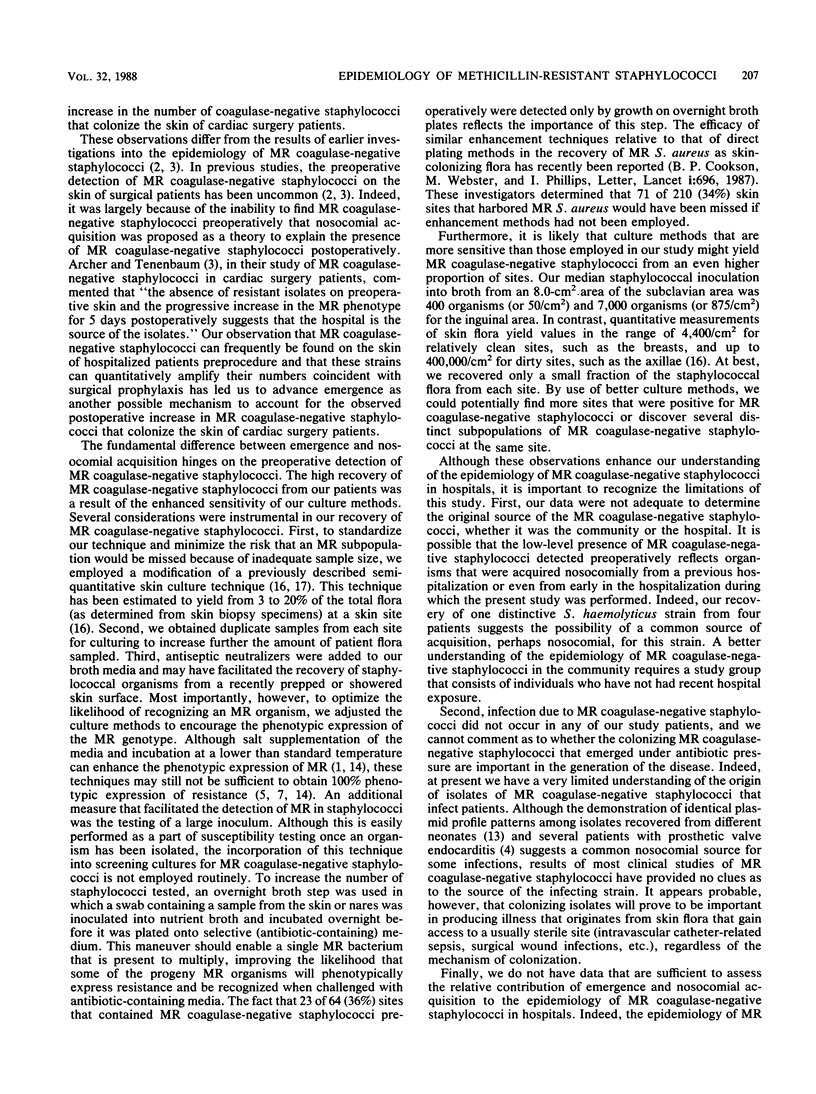
By use of techniques that have been developed to detect small numbers of methicillin-resistant staphylococci, we cultured samples from the nares and subclavian and inguinal areas of 29 patients before and after cardiac surgery and 10 patients before and after coronary angioplasty. Methicillin-resistant coagulase-negative staphylococci were recovered before the surgical or angioplasty procedure from 74% of patients. The quantitative recovery of methicillin-resistant isolates before cardiac surgery or coronary angioplasty was compared with the number of methicillin-resistant staphylococci detected at the same site 3 days after the procedure. In cardiac surgery patients (who received antibiotic prophylaxis), 17 of the 28 sites (61%) in which low-level colonization with methicillin-resistant strains was detected preoperatively contained high levels of methicillin-resistant staphylococci postoperatively. In contrast, coronary angioplasty patients (who did not receive antibiotic prophylaxis) did not have any of the 14 sites containing low levels of methicillin-resistant strains before angioplasty emerge to harbor high levels of methicillin-resistant staphylococci after angioplasty. Methicillin-resistant coagulase-negative staphylococci from each site in which high levels of methicillin-resistant staphylococci emerged postoperatively were paired with preoperative isolates from the same site. Identical antibiograms and plasmid profile patterns were demonstrated for seven of the pre- and postoperative isolate pairs, suggesting that the high levels of methicillin-resistant coagulase-negative staphylococci detected on the skin or in the nares after cardiac surgery were derived from methicillin-resistant organisms present at the site preoperatively in much smaller numbers.
Full text
PDF

Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Annear D. I. The effect of temperature on resistance of Staphylococcus aureus to methicillin and some other antibioics. Med J Aust. 1968 Mar 16;1(11):444–446. [PubMed] [Google Scholar]
- Archer G. L., Armstrong B. C. Alteration of staphylococcal flora in cardiac surgery patients receiving antibiotic prophylaxis. J Infect Dis. 1983 Apr;147(4):642–649. doi: 10.1093/infdis/147.4.642. [DOI] [PubMed] [Google Scholar]
- Archer G. L., Tenenbaum M. J. Antibiotic-resistant Staphylococcus epidermidis in patients undergoing cardiac surgery. Antimicrob Agents Chemother. 1980 Feb;17(2):269–272. doi: 10.1128/aac.17.2.269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Archer G. L., Vishniavsky N., Stiver H. G. Plasmid pattern analysis of Staphylococcal epidermidis isolates from patients with prosthetic valve endocarditis. Infect Immun. 1982 Feb;35(2):627–632. doi: 10.1128/iai.35.2.627-632.1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- BARBER M. NATURALLY OCCURING METHICILLIN-RESISTANT STAPHYLOCOCCI. J Gen Microbiol. 1964 May;35:183–190. doi: 10.1099/00221287-35-2-183. [DOI] [PubMed] [Google Scholar]
- Forbes B. A., Schaberg D. R. Transfer of resistance plasmids from Staphylococcus epidermidis to Staphylococcus aureus: evidence for conjugative exchange of resistance. J Bacteriol. 1983 Feb;153(2):627–634. doi: 10.1128/jb.153.2.627-634.1983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartman B. J., Tomasz A. Expression of methicillin resistance in heterogeneous strains of Staphylococcus aureus. Antimicrob Agents Chemother. 1986 Jan;29(1):85–92. doi: 10.1128/aac.29.1.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kloos W. E., Wolfshohl J. F. Identification of Staphylococcus species with the API STAPH-IDENT system. J Clin Microbiol. 1982 Sep;16(3):509–516. doi: 10.1128/jcm.16.3.509-516.1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lilly H. A., Lowbury E. J., Wilkins M. D. Limits to progressive reduction of resident skin bacteria by disinfection. J Clin Pathol. 1979 Apr;32(4):382–385. doi: 10.1136/jcp.32.4.382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon I. H. The use of inactivators in the evaluation of disinfectants. J Hyg (Lond) 1974 Oct;73(2):189–195. doi: 10.1017/s0022172400024013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montes L. F., Wilborn W. H. Anatomical location of normal skin flora. Arch Dermatol. 1970 Feb;101(2):145–159. [PubMed] [Google Scholar]
- Parisi J. T., Hecht D. W. Plasmid profiles in epidemiologic studies of infections by Staphylococcus epidermidis. J Infect Dis. 1980 May;141(5):637–643. doi: 10.1093/infdis/141.5.637. [DOI] [PubMed] [Google Scholar]
- Sabath L. D. Chemical and physical factors influencing methicillin resistance of Staphylococcus aureus and Staphylococcus epidermidis. J Antimicrob Chemother. 1977 Nov;3 (Suppl 100):47–51. doi: 10.1093/jac/3.suppl_c.47. [DOI] [PubMed] [Google Scholar]
- Saravolatz L. D., Markowitz N., Arking L., Pohlod D., Fisher E. Methicillin-resistant Staphylococcus aureus. Epidemiologic observations during a community-acquired outbreak. Ann Intern Med. 1982 Jan;96(1):11–16. doi: 10.7326/0003-4819-96-1-11. [DOI] [PubMed] [Google Scholar]
- Selwyn S., Ellis H. Skin bacteria and skin disinfection reconsidered. Br Med J. 1972 Jan 15;1(5793):136–140. doi: 10.1136/bmj.1.5793.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williamson P., Kligman A. M. A new method for the quantitative investigation of cutaneous bacteria. J Invest Dermatol. 1965 Dec;45(6):498–503. doi: 10.1038/jid.1965.164. [DOI] [PubMed] [Google Scholar]