Abstract
Objective: To describe the magnetic resonance imaging (MRI) characteristics of punctate brain lesions in neonates (number, appearance, distribution, and association with other brain abnormalities) and to relate them to neurodevelopmental outcome.
Methods: A retrospective analysis was performed of 110 MRI brain scans from 92 infants admitted in 1998 to the neonatal intensive care unit. Results of routine neurodevelopmental follow up (1998–2001) in those infants with punctate brain lesions were analysed.
Results: Punctate lesions were observed in 15/50 preterm and 2/42 term infants. In the preterm group, the number of lesions was < 3 in 20%, 3–10 in 27%, and > 10 in 53%. In 14/15 the lesions were linearly organised and located in the centrum semiovale. Other brain abnormalities were absent or minor—that is, "isolated" punctate lesions—in 8/15 and major in 7/15. In the term group, punctate lesions were organised in clusters and no other brain abnormalities were observed. Isolated punctate lesions were observed in 10/17 infants, and a normal neurodevelopmental outcome was seen in 9/10 (mean follow up 29.5 months). One infant showed a slight delay in language development. In the infants with associated brain lesions (7/17, mean follow up 27.5 months), outcome was normal in only two subjects.
Conclusions: Punctate lesions are predominantly seen in preterm infants, are usually linearly organised, and border the lateral ventricles. Isolated punctate lesions may imply a good prognosis, because most of these subjects have a normal neurodevelopmental outcome so far.
Full Text
The Full Text of this article is available as a PDF (175.8 KB).
Figure 1 .
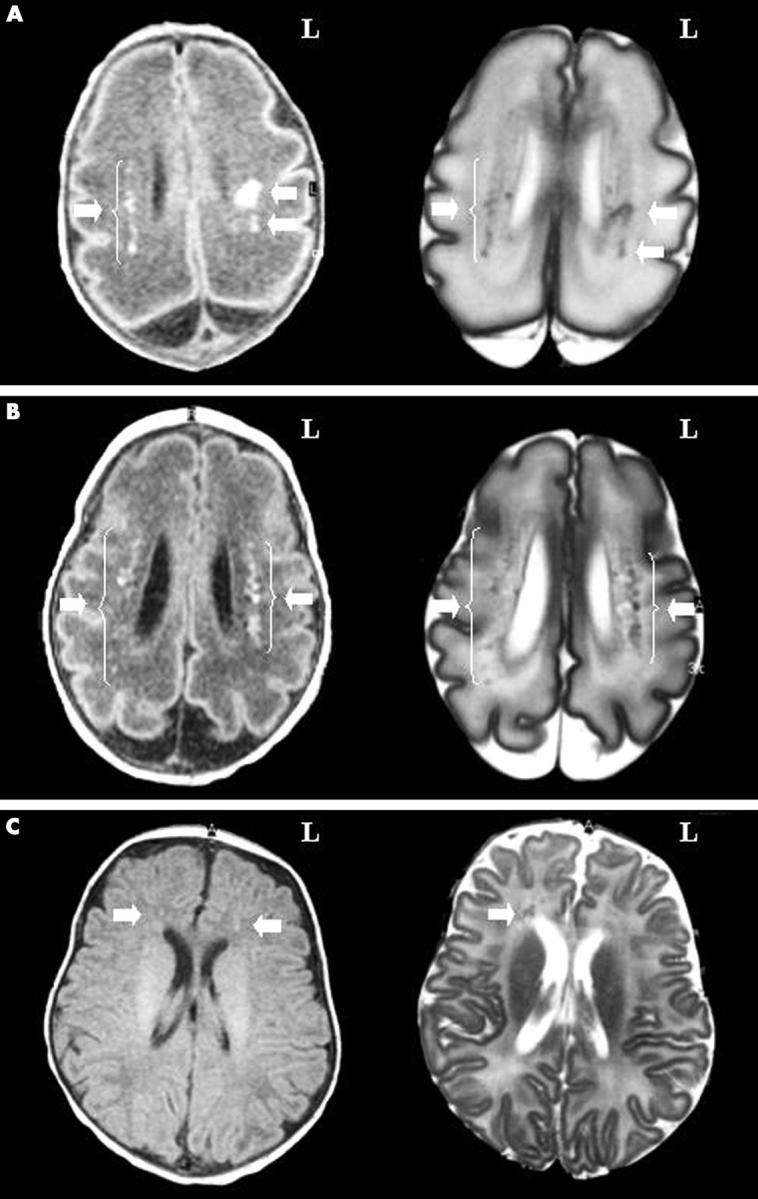
Magnetic resonance characterisation of punctate lesions. (A) Isolated punctate lesions in an infant of 28 weeks gestation, scanned at 7 days of age (corresponding to case 1 in table 1). Left panel: T1 weighted axial image through the body of the lateral ventricles. Bilateral high intensity spots (arrows) correspond to punctate lesions, predominantly seen in the mid and posterior regions of the brain. In the right hemisphere, lesions (about 10) are linearly organised in the periventricular white matter. In the left hemisphere, lesions are organised in a mixed-type pattern (clustered and linear). No other brain abnormalities are observed. L, Left. Right panel: corresponding T2 weighted axial image of same infant. Bilateral low intensity spots (arrows) correspond to punctate lesions. (B) Punctate lesions in an infant of 29 weeks gestation with cystic periventricular leucomalacia (PVL), scanned at 26 days of age (corresponding to case 11 in table 1). Left panel: T1 weighted axial image through the body of the lateral ventricles. Bilateral high intensity spots (arrows) correspond to punctate lesions, predominantly seen in the mid and posterior regions of the brain. In the two hemispheres, the lesions are linearly organised and border a medially located discrete band of low signal intensity lesions in the periventricular white matter. Right panel: corresponding T2 weighted axial image of same infant. Bilateral low intensity spots (arrows) correspond to punctate lesions. The punctate lesions are clearly neighbouring a medial region of cystic PVL (high intensity lesions, corresponding to cystic degeneration). (C) Isolated punctate lesions in an infant of 40 weeks gestation, scanned at 51 days of age (corresponding to case 16 in table 1). Left panel: T1 weighted axial image through the body of the lateral ventricles. Bilateral high intensity spots (arrows) correspond to punctate lesions, exclusively seen in the anterior region of the brain. No anatomical or myelination abnormalities are observed. Right panel: corresponding T2 weighted axial image of same infant. Low intensity spots (arrow) correspond to punctate lesions. In the right hemisphere, a cluster of six lesions is observed, whereas only one spot is clearly distinguished on the T1 weighted image.
Figure 2 .
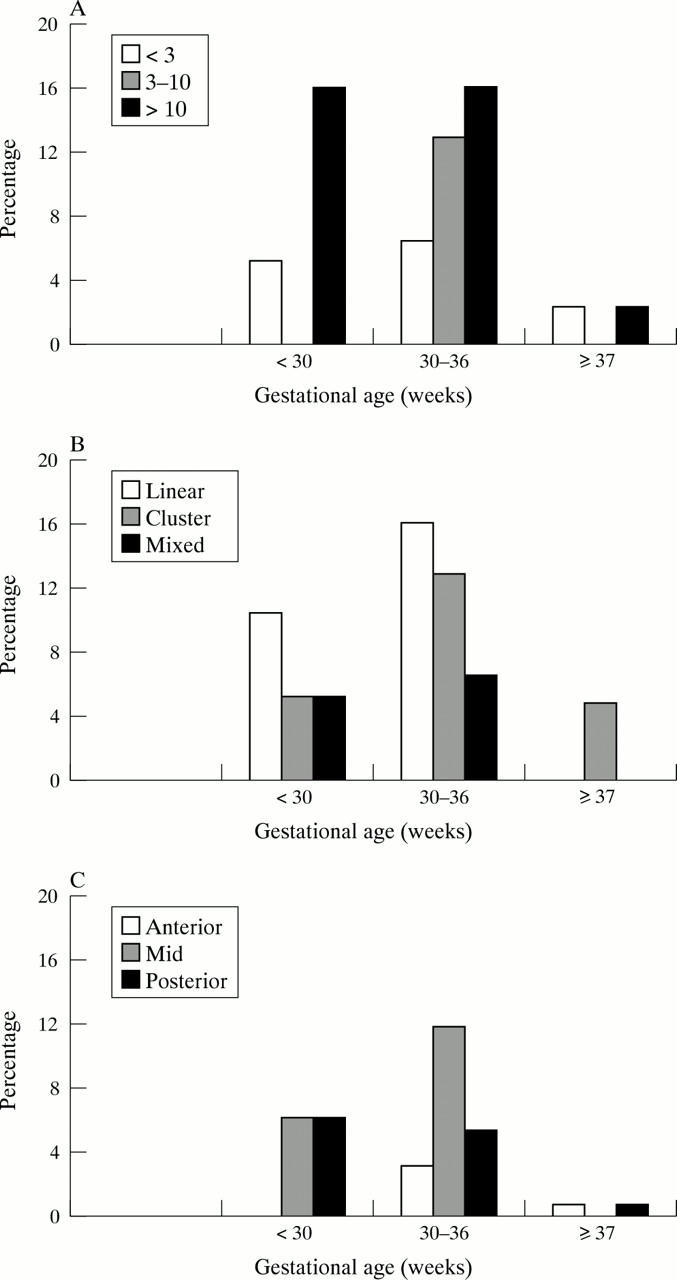
Overview of punctate lesions. Results are grouped according to the gestational age of all subjects analysed (n = 92): < 30 weeks (n = 19), between 30 and 36 weeks (n = 31), and ≥ 37 weeks (n = 42). (A) Number of punctate lesions. The percentage of cases with < 3, 3–10, or > 10 lesions is plotted for the different groups. (B) Appearance of punctate lesions. The percentage of cases with linear, clustered, or mixed appearance is plotted for the different groups. (C) Topography of punctate lesions. The percentage of cases in the anterior, mid, or posterior region of the brain is plotted for the different groups. As lesions were observed in the anterior, mid, and posterior region of the brain, we multiplied the total number of cases by three to calculate the percentage.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Aida N., Nishimura G., Hachiya Y., Matsui K., Takeuchi M., Itani Y. MR imaging of perinatal brain damage: comparison of clinical outcome with initial and follow-up MR findings. AJNR Am J Neuroradiol. 1998 Nov-Dec;19(10):1909–1921. [PMC free article] [PubMed] [Google Scholar]
- Armstrong D., Norman M. G. Periventricular leucomalacia in neonates. Complications and sequelae. Arch Dis Child. 1974 May;49(5):367–375. doi: 10.1136/adc.49.5.367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baenziger O., Martin E., Steinlin M., Good M., Largo R., Burger R., Fanconi S., Duc G., Buchli R., Rumpel H. Early pattern recognition in severe perinatal asphyxia: a prospective MRI study. Neuroradiology. 1993;35(6):437–442. doi: 10.1007/BF00602824. [DOI] [PubMed] [Google Scholar]
- Battin M. R., Maalouf E. F., Counsell S. J., Herlihy A. H., Rutherford M. A., Azzopardi D., Edwards A. D. Magnetic resonance imaging of the brain in very preterm infants: visualization of the germinal matrix, early myelination, and cortical folding. Pediatrics. 1998 Jun;101(6):957–962. doi: 10.1542/peds.101.6.957. [DOI] [PubMed] [Google Scholar]
- Byrne P., Welch R., Johnson M. A., Darrah J., Piper M. Serial magnetic resonance imaging in neonatal hypoxic-ischemic encephalopathy. J Pediatr. 1990 Nov;117(5):694–700. doi: 10.1016/s0022-3476(05)83323-2. [DOI] [PubMed] [Google Scholar]
- Childs A. M., Cornette L., Ramenghi L. A., Tanner S. F., Arthur R. J., Martinez D., Levene M. I. Magnetic resonance and cranial ultrasound characteristics of periventricular white matter abnormalities in newborn infants. Clin Radiol. 2001 Aug;56(8):647–655. doi: 10.1053/crad.2001.0754. [DOI] [PubMed] [Google Scholar]
- Childs A. M., Ramenghi L. A., Evans D. J., Ridgeway J., Saysell M., Martinez D., Arthur R., Tanner S., Levene M. I. MR features of developing periventricular white matter in preterm infants: evidence of glial cell migration. AJNR Am J Neuroradiol. 1998 May;19(5):971–976. [PMC free article] [PubMed] [Google Scholar]
- Chugani H. T., Phelps M. E., Mazziotta J. C. Positron emission tomography study of human brain functional development. Ann Neurol. 1987 Oct;22(4):487–497. doi: 10.1002/ana.410220408. [DOI] [PubMed] [Google Scholar]
- Cowan F. M., Pennock J. M., Hanrahan J. D., Manji K. P., Edwards A. D. Early detection of cerebral infarction and hypoxic ischemic encephalopathy in neonates using diffusion-weighted magnetic resonance imaging. Neuropediatrics. 1994 Aug;25(4):172–175. doi: 10.1055/s-2008-1073018. [DOI] [PubMed] [Google Scholar]
- De Vries L. S., Connell J. A., Dubowitz L. M., Oozeer R. C., Dubowitz V., Pennock J. M. Neurological, electrophysiological and MRI abnormalities in infants with extensive cystic leukomalacia. Neuropediatrics. 1987 May;18(2):61–66. doi: 10.1055/s-2008-1052453. [DOI] [PubMed] [Google Scholar]
- Gomori J. M., Grossman R. I., Goldberg H. I., Zimmerman R. A., Bilaniuk L. T. Intracranial hematomas: imaging by high-field MR. Radiology. 1985 Oct;157(1):87–93. doi: 10.1148/radiology.157.1.4034983. [DOI] [PubMed] [Google Scholar]
- Huppi P. S., Inder T. E. Magnetic resonance techniques in the evaluation of the perinatal brain: recent advances and future directions. Semin Neonatol. 2001 Apr;6(2):195–210. doi: 10.1053/siny.2001.0039. [DOI] [PubMed] [Google Scholar]
- Keeney S. E., Adcock E. W., McArdle C. B. Prospective observations of 100 high-risk neonates by high-field (1.5 Tesla) magnetic resonance imaging of the central nervous system. II. Lesions associated with hypoxic-ischemic encephalopathy. Pediatrics. 1991 Apr;87(4):431–438. [PubMed] [Google Scholar]
- Martin E., Barkovich A. J. Magnetic resonance imaging in perinatal asphyxia. Arch Dis Child Fetal Neonatal Ed. 1995 Jan;72(1):F62–F70. doi: 10.1136/fn.72.1.f62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mercuri E., Rutherford M., Cowan F., Pennock J., Counsell S., Papadimitriou M., Azzopardi D., Bydder G., Dubowitz L. Early prognostic indicators of outcome in infants with neonatal cerebral infarction: a clinical, electroencephalogram, and magnetic resonance imaging study. Pediatrics. 1999 Jan;103(1):39–46. doi: 10.1542/peds.103.1.39. [DOI] [PubMed] [Google Scholar]
- Millet V., Bartoli J. M., Lacroze V., Raybaud C., Unal D., Girard N. Predictive significance of magnetic resonance imaging at 4 months of adjusted age in infants after a perinatal neurologic insult. Biol Neonate. 1998;73(4):207–219. doi: 10.1159/000013979. [DOI] [PubMed] [Google Scholar]
- Neil J. J., Shiran S. I., McKinstry R. C., Schefft G. L., Snyder A. Z., Almli C. R., Akbudak E., Aronovitz J. A., Miller J. P., Lee B. C. Normal brain in human newborns: apparent diffusion coefficient and diffusion anisotropy measured by using diffusion tensor MR imaging. Radiology. 1998 Oct;209(1):57–66. doi: 10.1148/radiology.209.1.9769812. [DOI] [PubMed] [Google Scholar]
- Robertson R. L., Ben-Sira L., Barnes P. D., Mulkern R. V., Robson C. D., Maier S. E., Rivkin M. J., du Plessis A. MR line-scan diffusion-weighted imaging of term neonates with perinatal brain ischemia. AJNR Am J Neuroradiol. 1999 Oct;20(9):1658–1670. [PMC free article] [PubMed] [Google Scholar]
- Rutherford M. A., Pennock J. M., Counsell S. J., Mercuri E., Cowan F. M., Dubowitz L. M., Edwards A. D. Abnormal magnetic resonance signal in the internal capsule predicts poor neurodevelopmental outcome in infants with hypoxic-ischemic encephalopathy. Pediatrics. 1998 Aug;102(2 Pt 1):323–328. doi: 10.1542/peds.102.2.323. [DOI] [PubMed] [Google Scholar]
- Rutherford M., Pennock J., Schwieso J., Cowan F., Dubowitz L. Hypoxic-ischaemic encephalopathy: early and late magnetic resonance imaging findings in relation to outcome. Arch Dis Child Fetal Neonatal Ed. 1996 Nov;75(3):F145–F151. doi: 10.1136/fn.75.3.f145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmidt R., Fazekas F., Kapeller P., Schmidt H., Hartung H. P. MRI white matter hyperintensities: three-year follow-up of the Austrian Stroke Prevention Study. Neurology. 1999 Jul 13;53(1):132–139. doi: 10.1212/wnl.53.1.132. [DOI] [PubMed] [Google Scholar]
- Sze G., De Armond S. J., Brant-Zawadzki M., Davis R. L., Norman D., Newton T. H. Foci of MRI signal (pseudo lesions) anterior to the frontal horns: histologic correlations of a normal finding. AJR Am J Roentgenol. 1986 Aug;147(2):331–337. doi: 10.2214/ajr.147.2.331. [DOI] [PubMed] [Google Scholar]
- Tanner S. F., Ramenghi L. A., Ridgway J. P., Berry E., Saysell M. A., Martinez D., Arthur R. J., Smith M. A., Levene M. I. Quantitative comparison of intrabrain diffusion in adults and preterm and term neonates and infants. AJR Am J Roentgenol. 2000 Jun;174(6):1643–1649. doi: 10.2214/ajr.174.6.1741643. [DOI] [PubMed] [Google Scholar]
- de Vries L. S., Eken P., Dubowitz L. M. The spectrum of leukomalacia using cranial ultrasound. Behav Brain Res. 1992 Jul 31;49(1):1–6. doi: 10.1016/s0166-4328(05)80189-5. [DOI] [PubMed] [Google Scholar]
- de Vries L. S., Rademaker K. J., Groenendaal F., Eken P., van Haastert I. C., Vandertop W. P., Gooskens R., Meiners L. C. Correlation between neonatal cranial ultrasound, MRI in infancy and neurodevelopmental outcome in infants with a large intraventricular haemorrhage with or without unilateral parenchymal involvement. Neuropediatrics. 1998 Aug;29(4):180–188. doi: 10.1055/s-2007-973558. [DOI] [PubMed] [Google Scholar]
- van Wezel-Meijler G., van der Knaap M. S., Sie L. T., Oosting J., van Amerongen A. H., Cranendonk A., Lafeber H. N. Magnetic resonance imaging of the brain in premature infants during the neonatal period. Normal phenomena and reflection of mild ultrasound abnormalities. Neuropediatrics. 1998 Apr;29(2):89–96. doi: 10.1055/s-2007-973541. [DOI] [PubMed] [Google Scholar]


