Abstract
Objectives: To examine the effect of low birth weight (LBW) and fetal anaemia (FA) on haemoglobin (Hb) patterns in infancy. To study the additional contribution of other risk factors known at birth. To examine the effect of iron supplementation during infancy on Hb levels.
Methods: A stratified cohort of infants in Malawi (83 with LBW (< 2500 g), 111 with FA (cord Hb < 125 g/l), 31 with both LBW and FA, and 176 controls) was followed during infancy. Hb levels were measured at about 2, 4, 6, 9, and 12 months of age. Repeated measures models were used to describe the changes in Hb levels over time.
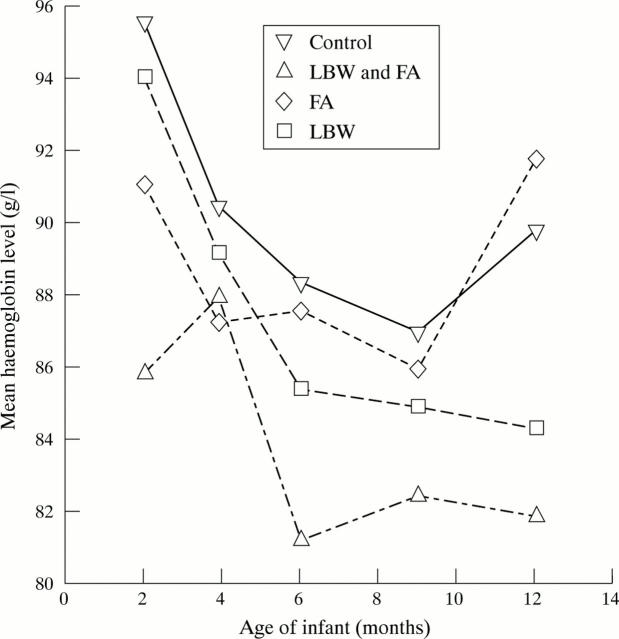
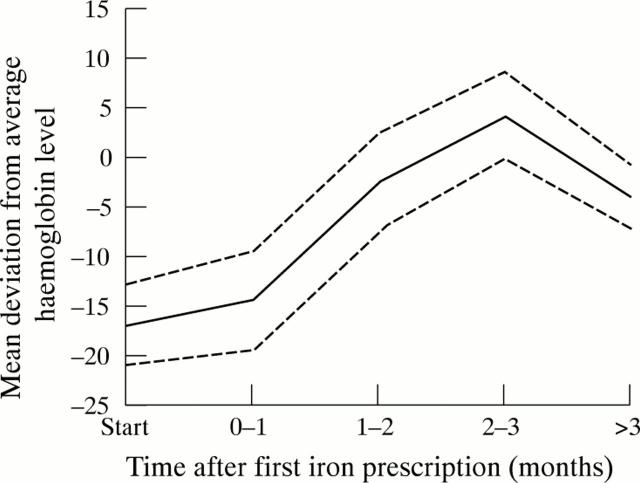
Results: The mean Hb concentration in the control group was 95.5 g/l (95% confidence interval (CI) 92.5 to 98.5) at 2 months, 86.9 g/l (95% CI 84.4 to 89.4) at 9 months, and 898 g/l (95% CI 874 to 92.2) at 12 months. Differences between LBW infants and controls increased over time (difference at 12 months: 5.5 g/l (95% CI 1.3 to 9.7)). Infants with FA had borderline significantly lower Hb at 2 months (p = 0.07), but at 6 months their levels were similar to those of controls. The LBW infants and those with FA had the lowest Hb levels (difference from controls at 12 months 7.9 g/l). Parity, placental and maternal malaria at delivery, and sex significantly affected Hb levels after adjustment for LBW and FA. After iron supplementation, Hb significantly increased.
Conclusions: Antimalarial control and iron supplementation throughout pregnancy should be increased to reduce the incidence of infant anaemia and improve child development and survival.
Full Text
The Full Text of this article is available as a PDF (121.9 KB).
Figure 1 .
Changes in haemoglobin levels during follow up for the four different stratification groups. LBW, Low birth weight; FA, fetal anaemia.
Figure 2 .
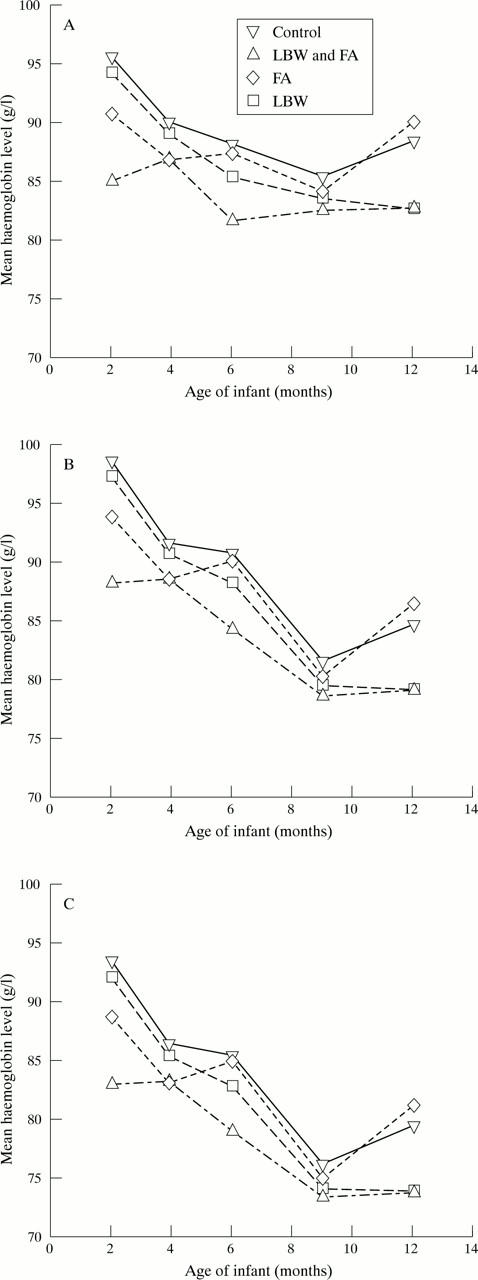
Mean haemoglobin levels during follow up, estimated from the multiple regression model, for infants with different characteristics at birth. (A) Girls without additional risk factors; (B) girls with malaria at delivery; (C) boys with placental and delivery malaria. LBW, Low birth weight; FA, fetal anaemia.
Figure 3 .
Difference in mean haemoglobin levels with 95% confidence interval as a function of time since first prescription, for infants who received one or more prescriptions of iron compared with infants of the same age and stratification group who did not receive iron.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Alonzo González M., Menéndez C., Font F., Kahigwa E., Kimario J., Mshinda H., Tanner M., Bosch-Capblanch X., Alonso P. L. Cost-effectiveness of iron supplementation and malaria chemoprophylaxis in the prevention of anaemia and malaria among Tanzanian infants. Bull World Health Organ. 2000;78(1):97–107. [PMC free article] [PubMed] [Google Scholar]
- Brabin B. Fetal anaemia in malarious areas: its causes and significance. Ann Trop Paediatr. 1992;12(3):303–310. doi: 10.1080/02724936.1992.11747589. [DOI] [PubMed] [Google Scholar]
- Burman D. Haemoglobin levels in normal infants aged 3 to 24 months, and the effect of iron. Arch Dis Child. 1972 Apr;47(252):261–271. doi: 10.1136/adc.47.252.261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chawla V., Haufton B. Pattern of childhood mortality at Harare Central Hospital, Zimbabwe. East Afr Med J. 1988 Apr;65(4):238–245. [PubMed] [Google Scholar]
- Commey J. O., Dekyem P. Childhood deaths from anaemia in Accra, Ghana. West Afr J Med. 1995 Apr-Jun;14(2):101–104. [PubMed] [Google Scholar]
- Cornet M., Le Hesran J. Y., Fievet N., Cot M., Personne P., Gounoue R., Beyeme M., Deloron P. Prevalence of and risk factors for anemia in young children in southern Cameroon. Am J Trop Med Hyg. 1998 May;58(5):606–611. doi: 10.4269/ajtmh.1998.58.606. [DOI] [PubMed] [Google Scholar]
- Dallman P. R., Siimes M. A., Stekel A. Iron deficiency in infancy and childhood. Am J Clin Nutr. 1980 Jan;33(1):86–118. doi: 10.1093/ajcn/33.1.86. [DOI] [PubMed] [Google Scholar]
- DeMaeyer E., Adiels-Tegman M. The prevalence of anaemia in the world. World Health Stat Q. 1985;38(3):302–316. [PubMed] [Google Scholar]
- Emond A. M., Hawkins N., Pennock C., Golding J. Haemoglobin and ferritin concentrations in infants at 8 months of age. Arch Dis Child. 1996 Jan;74(1):36–39. doi: 10.1136/adc.74.1.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hodges M., Williams R. A. Registered infant and under-five deaths in Freetown, Sierra Leone from 1987-1991 and a comparison with 1969-1979. West Afr J Med. 1998 Apr-Jun;17(2):95–98. [PubMed] [Google Scholar]
- Kitua A. Y., Smith T. A., Alonso P. L., Urassa H., Masanja H., Kimario J., Tanner M. The role of low level Plasmodium falciparum parasitaemia in anaemia among infants living in an area of intense and perennial transmission. Trop Med Int Health. 1997 Apr;2(4):325–333. doi: 10.1111/j.1365-3156.1997.tb00147.x. [DOI] [PubMed] [Google Scholar]
- Lackritz E. M., Campbell C. C., Ruebush T. K., 2nd, Hightower A. W., Wakube W., Steketee R. W., Were J. B. Effect of blood transfusion on survival among children in a Kenyan hospital. Lancet. 1992 Aug 29;340(8818):524–528. doi: 10.1016/0140-6736(92)91719-o. [DOI] [PubMed] [Google Scholar]
- Lozoff B. Methodologic issues in studying behavioral effects of infant iron-deficiency anemia. Am J Clin Nutr. 1989 Sep;50(3 Suppl):641–654. doi: 10.1093/ajcn/50.3.641. [DOI] [PubMed] [Google Scholar]
- Lundström U., Siimes M. A., Dallman P. R. At what age does iron supplementation become necessary in low-birth-weight infants? J Pediatr. 1977 Dec;91(6):878–883. doi: 10.1016/s0022-3476(77)80881-0. [DOI] [PubMed] [Google Scholar]
- Menendez C., Kahigwa E., Hirt R., Vounatsou P., Aponte J. J., Font F., Acosta C. J., Schellenberg D. M., Galindo C. M., Kimario J. Randomised placebo-controlled trial of iron supplementation and malaria chemoprophylaxis for prevention of severe anaemia and malaria in Tanzanian infants. Lancet. 1997 Sep 20;350(9081):844–850. doi: 10.1016/S0140-6736(97)04229-3. [DOI] [PubMed] [Google Scholar]
- Michaelsen K. F., Milman N., Samuelson G. A longitudinal study of iron status in healthy Danish infants: effects of early iron status, growth velocity and dietary factors. Acta Paediatr. 1995 Sep;84(9):1035–1044. doi: 10.1111/j.1651-2227.1995.tb138212.x. [DOI] [PubMed] [Google Scholar]
- Reed S. C., Wirima J. J., Steketee R. W. Risk factors for anemia in young children in rural Malawi. Am J Trop Med Hyg. 1994 Aug;51(2):170–174. doi: 10.4269/ajtmh.1994.51.170. [DOI] [PubMed] [Google Scholar]
- Stockman J. A., 3rd, Oski F. A. Physiological anaemia of infancy and the anaemia of prematurity. Clin Haematol. 1978 Feb;7(1):3–18. [PubMed] [Google Scholar]
- Verhoeff F. H., Brabin B. J., Hart C. A., Chimsuku L., Kazembe P., Broadhead R. L. Increased prevalence of malaria in HIV-infected pregnant women and its implications for malaria control. Trop Med Int Health. 1999 Jan;4(1):5–12. doi: 10.1046/j.1365-3156.1999.00349.x. [DOI] [PubMed] [Google Scholar]
- Verhoeff F. H., Milligan P., Brabin B. J., Mlanga S., Nakoma V. Gestational age assessment by nurses in a developing country using the Ballard method, external criteria only. Ann Trop Paediatr. 1997 Dec;17(4):333–342. doi: 10.1080/02724936.1997.11747907. [DOI] [PubMed] [Google Scholar]
- Williams R. L., Creasy R. K., Cunningham G. C., Hawes W. E., Norris F. D., Tashiro M. Fetal growth and perinatal viability in California. Obstet Gynecol. 1982 May;59(5):624–632. [PubMed] [Google Scholar]
- Wirima J. J. A nation-wide malaria knowledge, attitudes and practices survey in Malawi: introduction. Trop Med Parasitol. 1994 Mar;45(1):52–53. [PubMed] [Google Scholar]