Abstract
Objective: To determine if differences in respiratory muscle strength could explain any posture related effects on oxygenation in convalescent neonates.
Methods: Infants were examined in three postures: supine, supine with head up tilt of 45°, and prone. A subsequent study was performed to determine the influence of head position in the supine posture. In each posture/head position, oxygen saturation (SaO2) was determined and respiratory muscle strength assessed by measurement of the maximum inspiratory pressure (PIMAX).
Patients: Twenty infants, median gestational age 34.5 weeks (range 25–43), and 10 infants, median gestational age 33 weeks (range 30–36), were entered into the first and second study respectively.
Results: Oxygenation was higher in the prone and supine with 45° head up tilt postures than in the supine posture (p<0.001), whereas PIMAX was higher in the supine and supine with head up tilt of 45° postures than in the prone posture (p<0.001). Head position did not influence the effect of posture on PIMAX or oxygenation.
Conclusion: Superior oxygenation in the prone posture in convalescent infants was not explained by greater respiratory muscle strength, as this was superior in the supine posture.
Full Text
The Full Text of this article is available as a PDF (92.2 KB).
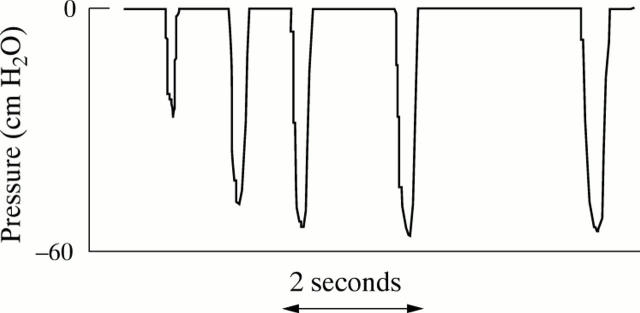
Figure 1 .
Representative trace of airway pressure during measurement of maximum inspiratory pressure (PIMAX). Airway occlusions were performed at end expiration on at least three separate occasions. Each occlusion was maintained until the infant had made at least five inspiratory efforts. From the series of occlusions, PIMAX was identified as the largest negative pressure generated.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Adams J. A., Zabaleta I. A., Sackner M. A. Comparison of supine and prone noninvasive measurements of breathing patterns in fullterm newborns. Pediatr Pulmonol. 1994 Jul;18(1):8–12. doi: 10.1002/ppul.1950180105. [DOI] [PubMed] [Google Scholar]
- Aiton N. R., Fox G. F., Alexander J., Ingram D. M., Milner A. D. The influence of sleeping position on functional residual capacity and effective pulmonary blood flow in healthy neonates. Pediatr Pulmonol. 1996 Dec;22(6):342–347. doi: 10.1002/(SICI)1099-0496(199612)22:6<342::AID-PPUL2>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- Anzueto A., Peters J. I., Tobin M. J., de los Santos R., Seidenfeld J. J., Moore G., Cox W. J., Coalson J. J. Effects of prolonged controlled mechanical ventilation on diaphragmatic function in healthy adult baboons. Crit Care Med. 1997 Jul;25(7):1187–1190. doi: 10.1097/00003246-199707000-00021. [DOI] [PubMed] [Google Scholar]
- Baird T. M., Paton J. B., Fisher D. E. Improved oxygenation with prone positioning in neonates: stability of increased transcutaneous PO2. J Perinatol. 1991 Dec;11(4):315–318. [PubMed] [Google Scholar]
- Black L. F., Hyatt R. E. Maximal static respiratory pressures in generalized neuromuscular disease. Am Rev Respir Dis. 1971 May;103(5):641–650. doi: 10.1164/arrd.1971.103.5.641. [DOI] [PubMed] [Google Scholar]
- Byrd R. B., Hyatt R. E. Maximal respiratory pressures in chronic obstructive lung disease. Am Rev Respir Dis. 1968 Nov;98(5):848–856. doi: 10.1164/arrd.1968.98.5.848. [DOI] [PubMed] [Google Scholar]
- Caruso P., Friedrich C., Denari S. D., Ruiz S. A., Deheinzelin D. The unidirectional valve is the best method to determine maximal inspiratory pressure during weaning. Chest. 1999 Apr;115(4):1096–1101. doi: 10.1378/chest.115.4.1096. [DOI] [PubMed] [Google Scholar]
- Cohn D., Benditt J. O., Eveloff S., McCool F. D. Diaphragm thickening during inspiration. J Appl Physiol (1985) 1997 Jul;83(1):291–296. doi: 10.1152/jappl.1997.83.1.291. [DOI] [PubMed] [Google Scholar]
- Dellagrammaticas H. D., Kapetanakis J., Papadimitriou M., Kourakis G. Effect of body tilting on physiological functions in stable very low birthweight neonates. Arch Dis Child. 1991 Apr;66(4 Spec No):429–432. doi: 10.1136/adc.66.4_spec_no.429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dimitriou G., Greenoug A., Dyke H., Rafferty G. F. Maximal airway pressures during crying in healthy preterm and term neonates. Early Hum Dev. 2000 Feb;57(2):149–156. doi: 10.1016/s0378-3782(99)00075-4. [DOI] [PubMed] [Google Scholar]
- Jenni O. G., von Siebenthal K., Wolf M., Keel M., Duc G., Bucher H. U. Effect of nursing in the head elevated tilt position (15 degrees) on the incidence of bradycardic and hypoxemic episodes in preterm infants. Pediatrics. 1997 Oct;100(4):622–625. doi: 10.1542/peds.100.4.622. [DOI] [PubMed] [Google Scholar]
- Kurlak L. O., Ruggins N. R., Stephenson T. J. Effect of nursing position on incidence, type, and duration of clinically significant apnoea in preterm infants. Arch Dis Child Fetal Neonatal Ed. 1994 Jul;71(1):F16–F19. doi: 10.1136/fn.71.1.f16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levene S., McKenzie S. A. Transcutaneous oxygen saturation in sleeping infants: prone and supine. Arch Dis Child. 1990 May;65(5):524–526. doi: 10.1136/adc.65.5.524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lioy J., Manginello F. P. A comparison of prone and supine positioning in the immediate postextubation period of neonates. J Pediatr. 1988 Jun;112(6):982–984. doi: 10.1016/s0022-3476(88)80230-0. [DOI] [PubMed] [Google Scholar]
- Margulies S. S., Farkas G. A., Rodarte J. R. Effects of body position and lung volume on in situ operating length of canine diaphragm. J Appl Physiol (1985) 1990 Nov;69(5):1702–1708. doi: 10.1152/jappl.1990.69.5.1702. [DOI] [PubMed] [Google Scholar]
- Martin R. J., DiFiore J. M., Korenke C. B., Randal H., Miller M. J., Brooks L. J. Vulnerability of respiratory control in healthy preterm infants placed supine. J Pediatr. 1995 Oct;127(4):609–614. doi: 10.1016/s0022-3476(95)70125-7. [DOI] [PubMed] [Google Scholar]
- Martin R. J., Herrell N., Rubin D., Fanaroff A. Effect of supine and prone positions on arterial oxygen tension in the preterm infant. Pediatrics. 1979 Apr;63(4):528–531. [PubMed] [Google Scholar]
- McCool F. D., Tzelepis G. E., Leith D. E., Hoppin F. G., Jr Oxygen cost of breathing during fatiguing inspiratory resistive loads. J Appl Physiol (1985) 1989 May;66(5):2045–2055. doi: 10.1152/jappl.1989.66.5.2045. [DOI] [PubMed] [Google Scholar]
- McEvoy C., Mendoza M. E., Bowling S., Hewlett V., Sardesai S., Durand M. Prone positioning decreases episodes of hypoxemia in extremely low birth weight infants (1000 grams or less) with chronic lung disease. J Pediatr. 1997 Feb;130(2):305–309. doi: 10.1016/s0022-3476(97)70360-3. [DOI] [PubMed] [Google Scholar]
- Mendoza J. C., Roberts J. L., Cook L. N. Postural effects on pulmonary function and heart rate of preterm infants with lung disease. J Pediatr. 1991 Mar;118(3):445–448. doi: 10.1016/s0022-3476(05)82166-3. [DOI] [PubMed] [Google Scholar]
- Newell S. J., Booth I. W., Morgan M. E., Durbin G. M., McNeish A. S. Gastro-oesophageal reflux in preterm infants. Arch Dis Child. 1989 Jun;64(6):780–786. doi: 10.1136/adc.64.6.780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polkey M. I., Hamnegård C. H., Hughes P. D., Rafferty G. F., Green M., Moxham J. Influence of acute lung volume change on contractile properties of human diaphragm. J Appl Physiol (1985) 1998 Oct;85(4):1322–1328. doi: 10.1152/jappl.1998.85.4.1322. [DOI] [PubMed] [Google Scholar]
- Rehan V. K., Nakashima J. M., Gutman A., Rubin L. P., McCool F. D. Effects of the supine and prone position on diaphragm thickness in healthy term infants. Arch Dis Child. 2000 Sep;83(3):234–238. doi: 10.1136/adc.83.3.234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shen X. M., Zhoa W., Huang D. S., Lin F. G., Wu S. M. Effect of positioning on pulmonary function of newborns: comparison of supine and prone position. Pediatr Pulmonol. 1996 Mar;21(3):167–170. doi: 10.1002/(SICI)1099-0496(199603)21:3<167::AID-PPUL3>3.0.CO;2-N. [DOI] [PubMed] [Google Scholar]
- Tam P., Lin L. H. Fifteen-hour continuous esophageal pH monitoring: influence of position on gastroesophageal reflux among asymptomatic babies. Zhonghua Min Guo Xiao Er Ke Yi Xue Hui Za Zhi. 1993 Jan-Feb;34(1):14–21. [PubMed] [Google Scholar]
- Thoresen M., Cowan F., Whitelaw A. Effect of tilting on oxygenation in newborn infants. Arch Dis Child. 1988 Mar;63(3):315–317. doi: 10.1136/adc.63.3.315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vandenplas Y., Sacre-Smits L. Seventeen-hour continuous esophageal pH monitoring in the newborn: evaluation of the influence of position in asymptomatic and symptomatic babies. J Pediatr Gastroenterol Nutr. 1985 Jun;4(3):356–361. doi: 10.1097/00005176-198506000-00006. [DOI] [PubMed] [Google Scholar]
- Wagaman M. J., Shutack J. G., Moomjian A. S., Schwartz J. G., Shaffer T. H., Fox W. W. Improved oxygenation and lung compliance with prone positioning of neonates. J Pediatr. 1979 May;94(5):787–791. doi: 10.1016/s0022-3476(79)80157-2. [DOI] [PubMed] [Google Scholar]
- Wolfson M. R., Greenspan J. S., Deoras K. S., Allen J. L., Shaffer T. H. Effect of position on the mechanical interaction between the rib cage and abdomen in preterm infants. J Appl Physiol (1985) 1992 Mar;72(3):1032–1038. doi: 10.1152/jappl.1992.72.3.1032. [DOI] [PubMed] [Google Scholar]