Full Text
The Full Text of this article is available as a PDF (169.2 KB).
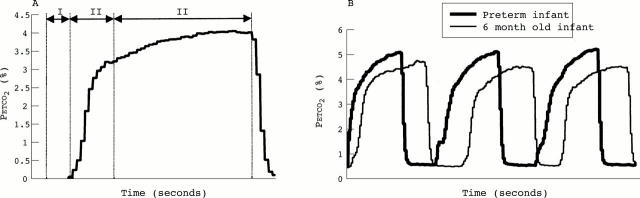
Figure 1 .
(A) The CO2 waveform has three phases. PETCO2 remains zero as gas from the anatomic dead space leaves the airway (phase I); it then rises sharply as alveolar gas mixes with dead space gas (phase II); as purely alveolar gas is exhaled, the curve levels (phase III). (B) The CO2 waveform from a small preterm infant (bold line) without an alveolar plateau (phase III), compared with that in a 6 month old infant (thin line) where the phase III is present.
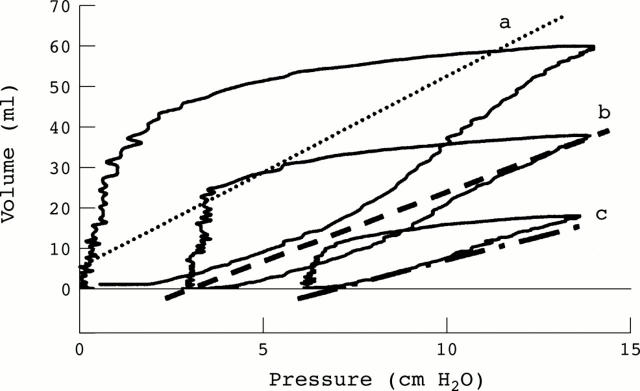
Figure 2 .
Three different pressure-volume curves of an infant (3.2 kg) with normal lungs during mechanical ventilation are shown. Positive end expiratory pressure has been changed from 0 (curve a) to 3 (curve b) and to 6 cm H2O (curve c). Cdyn, Re, and functional residual capacity were: curve a, 4.4 ml/cm H2O, 0.031 cm H2O/ml/s, and 60 ml; curve b, 3.0 ml/cm H2O, 0.025 cm H2O/ml/s, and 81 ml; curve c, 2.0 ml/cm H2O, 0.021 cm H2O/ml/s, and 92 ml.
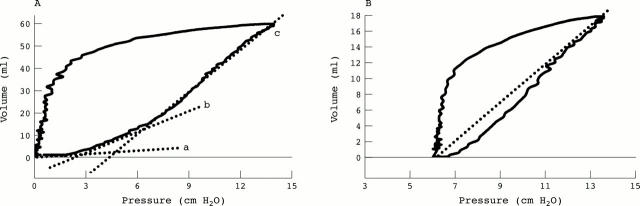
Figure 3 .
The pressure-volume curve of the same infant as in fig 2. When the lung is ventilated at 0 positive end expiratory pressure (PEEP) (A), a lower inflection point can be seen (crossing of line a and b). With increasing inspiratory pressure, the lungs are inflated and the pressure-volume relation becomes linear (line c). If PEEP is set to 6 (B), most of the inspiratory limb of the pressure-volume curve is linear.
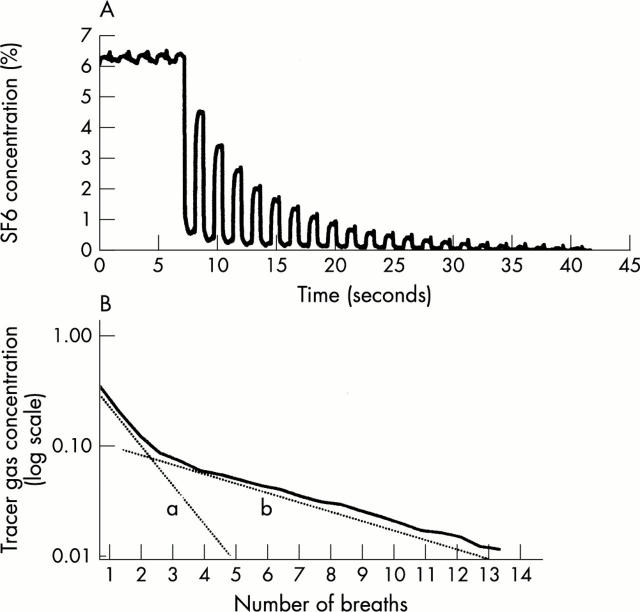
Figure 4 .
(A) An SF6 washout using an ultrasonic flow meter. (B) An SF6 washout of an infant with severe ventilation inhomogeneity. The SF6 concentration (log scale) is plotted against the number of breaths. There is an initial fast lung compartment (line a) followed by a slow emptying one (line b).
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Arnold J. H., Stenz R. I., Thompson J. E., Arnold L. W. Noninvasive determination of cardiac output using single breath CO2 analysis. Crit Care Med. 1996 Oct;24(10):1701–1705. doi: 10.1097/00003246-199610000-00017. [DOI] [PubMed] [Google Scholar]
- Freezer N. J., Sly P. D. Predictive value of measurements of respiratory mechanics in preterm infants with HMD. Pediatr Pulmonol. 1993 Aug;16(2):116–123. doi: 10.1002/ppul.1950160207. [DOI] [PubMed] [Google Scholar]
- Goldsmith L. S., Greenspan J. S., Rubenstein S. D., Wolfson M. R., Shaffer T. H. Immediate improvement in lung volume after exogenous surfactant: alveolar recruitment versus increased distention. J Pediatr. 1991 Sep;119(3):424–428. doi: 10.1016/s0022-3476(05)82057-8. [DOI] [PubMed] [Google Scholar]
- Habib R. H., Lutchen K. R. Moment analysis of a multibreath nitrogen washout based on an alveolar gas dilution number. Am Rev Respir Dis. 1991 Sep;144(3 Pt 1):513–519. doi: 10.1164/ajrccm/144.3_Pt_1.513. [DOI] [PubMed] [Google Scholar]
- Kraemer R., Meister B. Fast real-time moment-ratio analysis of multibreath nitrogen washout in children. J Appl Physiol (1985) 1985 Oct;59(4):1137–1144. doi: 10.1152/jappl.1985.59.4.1137. [DOI] [PubMed] [Google Scholar]
- Lanteri C. J., Kano S., Nicolai T., Sly P. D. Measurement of dynamic respiratory mechanics in neonatal and pediatric intensive care: the multiple linear regression technique. Pediatr Pulmonol. 1995 Jan;19(1):29–45. doi: 10.1002/ppul.1950190106. [DOI] [PubMed] [Google Scholar]
- Larsson A., Jonmarker C., Werner O. Ventilation inhomogeneity during controlled ventilation. Which index should be used? J Appl Physiol (1985) 1988 Nov;65(5):2030–2039. doi: 10.1152/jappl.1988.65.5.2030. [DOI] [PubMed] [Google Scholar]
- Mariani G., Cifuentes J., Carlo W. A. Randomized trial of permissive hypercapnia in preterm infants. Pediatrics. 1999 Nov;104(5 Pt 1):1082–1088. doi: 10.1542/peds.104.5.1082. [DOI] [PubMed] [Google Scholar]
- Pfenninger J., Aebi C., Bachmann D., Wagner B. P. Lung mechanics and gas exchange in ventilated preterm infants during treatment of hyaline membrane disease with multiple doses of artificial surfactant (Exosurf) Pediatr Pulmonol. 1992 Sep;14(1):10–15. doi: 10.1002/ppul.1950140104. [DOI] [PubMed] [Google Scholar]
- Ream R. S., Schreiner M. S., Neff J. D., McRae K. M., Jawad A. F., Scherer P. W., Neufeld G. R. Volumetric capnography in children. Influence of growth on the alveolar plateau slope. Anesthesiology. 1995 Jan;82(1):64–73. doi: 10.1097/00000542-199501000-00010. [DOI] [PubMed] [Google Scholar]
- Schibler A., Henning R. Measurement of functional residual capacity in rabbits and children using an ultrasonic flow meter. Pediatr Res. 2001 Apr;49(4):581–588. doi: 10.1203/00006450-200104000-00022. [DOI] [PubMed] [Google Scholar]
- Schibler A., Schneider M., Frey U., Kraemer R. Moment ratio analysis of multiple breath nitrogen washout in infants with lung disease. Eur Respir J. 2000 Jun;15(6):1094–1101. doi: 10.1034/j.1399-3003.2000.01518.x. [DOI] [PubMed] [Google Scholar]
- Schulze A., Schaller P., Töpfer A., Kirpalani H. Measurement of functional residual capacity by sulfur hexafluoride in small-volume lungs during spontaneous breathing and mechanical ventilation. Pediatr Res. 1994 Apr;35(4 Pt 1):494–499. [PubMed] [Google Scholar]
- Sivan Y., Deakers T. W., Newth C. J. An automated bedside method for measuring functional residual capacity by N2 washout in mechanically ventilated children. Pediatr Res. 1990 Nov;28(5):446–450. doi: 10.1203/00006450-199011000-00005. [DOI] [PubMed] [Google Scholar]
- Sivan Y., Deakers T. W., Newth C. J. Functional residual capacity in ventilated infants and children. Pediatr Res. 1990 Nov;28(5):451–454. doi: 10.1203/00006450-199011000-00006. [DOI] [PubMed] [Google Scholar]
- Sivan Y., Eldadah M. K., Cheah T. E., Newth C. J. Estimation of arterial carbon dioxide by end-tidal and transcutaneous PCO2 measurements in ventilated children. Pediatr Pulmonol. 1992 Mar;12(3):153–157. doi: 10.1002/ppul.1950120305. [DOI] [PubMed] [Google Scholar]
- Tepper R. S., Asdell S. Comparison of helium dilution and nitrogen washout measurements of functional residual capacity in infants and very young children. Pediatr Pulmonol. 1992 Aug;13(4):250–254. doi: 10.1002/ppul.1950130414. [DOI] [PubMed] [Google Scholar]
- Vilstrup C. T., Björklund L. J., Larsson A., Lachmann B., Werner O. Functional residual capacity and ventilation homogeneity in mechanically ventilated small neonates. J Appl Physiol (1985) 1992 Jul;73(1):276–283. doi: 10.1152/jappl.1992.73.1.276. [DOI] [PubMed] [Google Scholar]