Abstract
Objective: To assess the effect of routine measurement of postductal oxygen saturation as an adjunct to routine clinical examination in the asymptomatic newborn.
Design and setting: Prospective study in a district general hospital.
Patients: All 6166 infants inborn between 1 April 1999 and 31 March 2001.
Intervention: Oxygen saturation was measured over two minutes, after the age of 2 hours and before discharge, in one foot of all babies not admitted directly to the neonatal unit. Babies with fractional (as opposed to functional) oxygen saturation (SaO2) below 95% were examined by the midwife. If this examination was abnormal or if normal but further measurements were below 95%, an echocardiogram was performed. All babies with cardiac malformations diagnosed by 1 year of age were identified from databases maintained at the regional cardiology referral unit and the regional congenital malformation survey.
Results: Measurements were made in 98% of eligible babies. A fractional SaO2 less than 95% was found in 5% but persisted in only 1%. Structural cardiac malformations were found in 50 (8.1/1000), 26 of whom had isolated ventricular septal defects. Of the remaining 24 with other cardiac malformations, attention was first drawn to six by low SaO2, and four more, first noticed for other reasons, also had low SaO2. Low SaO2 also first drew attention to 13 other babies ill for other reasons.
Conclusion: Newborn babies with important cardiac malformations are often asymptomatic initially and the yield from clinical examination is poor. Measuring postductal saturation routinely in newborn babies before discharge is easy and can alert staff to ill babies.
Full Text
The Full Text of this article is available as a PDF (239.7 KB).
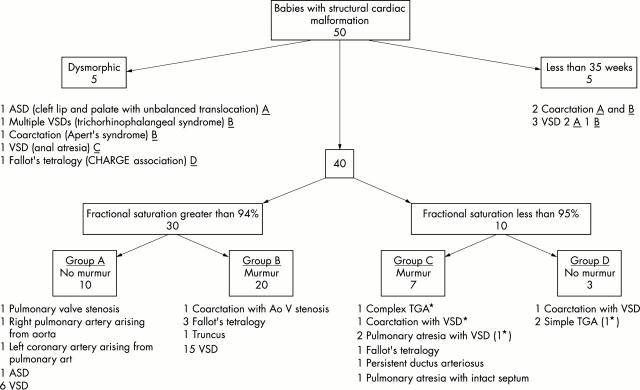
Figure 1 .

Flow chart showing how the babies with low saturation and those with congenital cardiac malformation were processed. CVS exam means clinical examination of the cardiovascular system, and exam means clinical examination including CVS examination. *An additional 10 babies with congenital cardiac malformation were also identified among babies who were either preterm (less than 35 weeks gestation) or dysmorphic.
Figure 2 .
Flow chart showing the signs exhibited in the first days of life in the 50 cases of congenital cardiac malformation. The letters A, B, C, D next to those cases listed in the dysmorphic and preterm groups indicate which other group (low saturation with no murmur etc) they would have been in had attention not already been drawn to them by their dysmorphism or preterm status. Babies are classed as having a murmur if a murmur was detected before discharge home or in the first week of life in babies discharged after 7 days of age. ASD, Atrial septal defect; VSD, ventricular septal defect; TGA, transposition of the great arteries. * denotes antenatal diagnosis.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Abu-Harb M., Hey E., Wren C. Death in infancy from unrecognised congenital heart disease. Arch Dis Child. 1994 Jul;71(1):3–7. doi: 10.1136/adc.71.1.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abu-Harb M., Wyllie J., Hey E., Richmond S., Wren C. Presentation of obstructive left heart malformations in infancy. Arch Dis Child Fetal Neonatal Ed. 1994 Nov;71(3):F179–F183. doi: 10.1136/fn.71.3.f179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ainsworth S., Wyllie J. P., Wren C. Prevalence and clinical significance of cardiac murmurs in neonates. Arch Dis Child Fetal Neonatal Ed. 1999 Jan;80(1):F43–F45. doi: 10.1136/fn.80.1.f43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonnet D., Coltri A., Butera G., Fermont L., Le Bidois J., Kachaner J., Sidi D. Detection of transposition of the great arteries in fetuses reduces neonatal morbidity and mortality. Circulation. 1999 Feb 23;99(7):916–918. doi: 10.1161/01.cir.99.7.916. [DOI] [PubMed] [Google Scholar]
- Katzman G. H. The newborn's SpO2: a routine vital sign whose time has come? Pediatrics. 1995 Jan;95(1):161–162. [PubMed] [Google Scholar]
- Poets C. F., Southall D. P. Noninvasive monitoring of oxygenation in infants and children: practical considerations and areas of concern. Pediatrics. 1994 May;93(5):737–746. [PubMed] [Google Scholar]
- Pollitt R. J., Green A., McCabe C. J., Booth A., Cooper N. J., Leonard J. V., Nicholl J., Nicholson P., Tunaley J. R., Virdi N. K. Neonatal screening for inborn errors of metabolism: cost, yield and outcome. Health Technol Assess. 1997;1(7):i-iv, 1-202. [PubMed] [Google Scholar]
- Wren C., Richmond S., Donaldson L. Presentation of congenital heart disease in infancy: implications for routine examination. Arch Dis Child Fetal Neonatal Ed. 1999 Jan;80(1):F49–F53. doi: 10.1136/fn.80.1.f49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wren C., Richmond S., Donaldson L. Temporal variability in birth prevalence of cardiovascular malformations. Heart. 2000 Apr;83(4):414–419. doi: 10.1136/heart.83.4.414. [DOI] [PMC free article] [PubMed] [Google Scholar]