Abstract
Background: Preterm infants with chronic lung disease (CLD) had impaired cognitive development and poorer eye-hand coordination at 10 months of age.
Aims: To study whether this effect of CLD persisted until school age and whether the severity of CLD affected outcome.
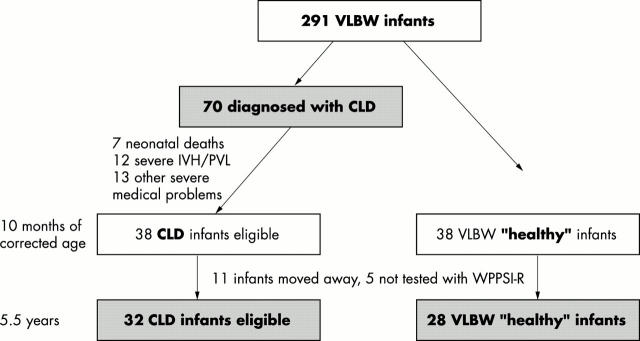
Method: Cognition and visual-motor skills were examined (Wechsler preschool and primary scale of intelligence, and tests from the Nepsy scale) in 60 very preterm children, without intraventricular haemorrhage or periventricular leucomalacia, at 5.5 years of age. Thirty two children suffered from CLD and 28 were controls.
Results: The groups did not differ significantly in cognitive outcome. Children with CLD and controls attained a full scale intelligence quotient (IQ) of 94.4 and 99.1, a verbal IQ of 99.6 and 101.5, and a performance IQ of 90.9 and 96.7 respectively. Similarly, no difference was found in tests of eye-hand control. However, the children with the most severe form of CLD had significantly lower performance (84.8) and full scale(87.6) IQs and worse visual-motor performance than the controls. CLD grade III, together with the need for glasses or lenses, had a significant impact on the explained variance.
Conclusions: At school age, children born very preterm and who experienced severe CLD had deficits in cognition, visual-motor perception, and performance. The findings suggest a need to consider intervention programmes for such infants.
Full Text
The Full Text of this article is available as a PDF (136.9 KB).
Figure 1 .
Selection of study subjects. CLD, Chronic lung disease; VLBW, very low birthweight; PVL, periventricular leucomalacia; IVH, intraventricular haemorrhage.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bancalari E., Abdenour G. E., Feller R., Gannon J. Bronchopulmonary dysplasia: clinical presentation. J Pediatr. 1979 Nov;95(5 Pt 2):819–823. doi: 10.1016/s0022-3476(79)80442-4. [DOI] [PubMed] [Google Scholar]
- Barrington K. J. The adverse neuro-developmental effects of postnatal steroids in the preterm infant: a systematic review of RCTs. BMC Pediatr. 2001 Feb 27;1:1–1. doi: 10.1186/1471-2431-1-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowen J. R., Starte D. R., Arnold J. D., Simmons J. L., Ma P. J., Leslie G. I. Extremely low birthweight infants at 3 years: a developmental profile. J Paediatr Child Health. 1993 Aug;29(4):276–281. doi: 10.1111/j.1440-1754.1993.tb00511.x. [DOI] [PubMed] [Google Scholar]
- Clayton P. E., Trueman J. A. Leptin and puberty. Arch Dis Child. 2000 Jul;83(1):1–4. doi: 10.1136/adc.83.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durand M., McEvoy C., MacDonald K. Spontaneous desaturations in intubated very low birth weight infants with acute and chronic lung disease. Pediatr Pulmonol. 1992 Jul;13(3):136–142. doi: 10.1002/ppul.1950130303. [DOI] [PubMed] [Google Scholar]
- Gallo J. E., Holmström G., Kugelberg U., Hedquist B., Lennerstrand G. Regressed retinopathy of prematurity and its sequelae in children aged 5-10 years. Br J Ophthalmol. 1991 Sep;75(9):527–531. doi: 10.1136/bjo.75.9.527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein R. F., Thompson R. J., Jr, Oehler J. M., Brazy J. E. Influence of acidosis, hypoxemia, and hypotension on neurodevelopmental outcome in very low birth weight infants. Pediatrics. 1995 Feb;95(2):238–243. [PubMed] [Google Scholar]
- Hutton J. L., Pharoah P. O., Cooke R. W., Stevenson R. C. Differential effects of preterm birth and small gestational age on cognitive and motor development. Arch Dis Child Fetal Neonatal Ed. 1997 Mar;76(2):F75–F81. doi: 10.1136/fn.76.2.f75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jobe A. H., Bancalari E. Bronchopulmonary dysplasia. Am J Respir Crit Care Med. 2001 Jun;163(7):1723–1729. doi: 10.1164/ajrccm.163.7.2011060. [DOI] [PubMed] [Google Scholar]
- Keen D. V., Pearse R. G. Birthweight between 14 and 42 weeks' gestation. Arch Dis Child. 1985 May;60(5):440–446. doi: 10.1136/adc.60.5.440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korkman M., Liikanen A., Fellman V. Neuropsychological consequences of very low birth weight and asphyxia at term: follow-up until school-age. J Clin Exp Neuropsychol. 1996 Apr;18(2):220–233. doi: 10.1080/01688639608408277. [DOI] [PubMed] [Google Scholar]
- Krägeloh-Mann I., Toft P., Lunding J., Andresen J., Pryds O., Lou H. C. Brain lesions in preterms: origin, consequences and compensation. Acta Paediatr. 1999 Aug;88(8):897–908. doi: 10.1080/08035259950168856. [DOI] [PubMed] [Google Scholar]
- O'Shea T. M., Goldstein D. J., deRegnier R. A., Sheaffer C. I., Roberts D. D., Dillard R. G. Outcome at 4 to 5 years of age in children recovered from neonatal chronic lung disease. Dev Med Child Neurol. 1996 Sep;38(9):830–839. doi: 10.1111/j.1469-8749.1996.tb15118.x. [DOI] [PubMed] [Google Scholar]
- Olsén P., Päkkö E., Vainionpä L., Pyhtinen J., Järvelin M. R. Magnetic resonance imaging of periventricular leukomalacia and its clinical correlation in children. Ann Neurol. 1997 Jun;41(6):754–761. doi: 10.1002/ana.410410611. [DOI] [PubMed] [Google Scholar]
- Sekar K. C., Duke J. C. Sleep apnea and hypoxemia in recently weaned premature infants with and without bronchopulmonary dysplasia. Pediatr Pulmonol. 1991;10(2):112–116. doi: 10.1002/ppul.1950100213. [DOI] [PubMed] [Google Scholar]
- Singer L., Martin R. J., Hawkins S. W., Benson-Szekely L. J., Yamashita T. S., Carlo W. A. Oxygen desaturation complicates feeding in infants with bronchopulmonary dysplasia after discharge. Pediatrics. 1992 Sep;90(3):380–384. [PMC free article] [PubMed] [Google Scholar]
- Singer L., Yamashita T., Lilien L., Collin M., Baley J. A longitudinal study of developmental outcome of infants with bronchopulmonary dysplasia and very low birth weight. Pediatrics. 1997 Dec;100(6):987–993. doi: 10.1542/peds.100.6.987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skidmore M. D., Rivers A., Hack M. Increased risk of cerebral palsy among very low-birthweight infants with chronic lung disease. Dev Med Child Neurol. 1990 Apr;32(4):325–332. doi: 10.1111/j.1469-8749.1990.tb16944.x. [DOI] [PubMed] [Google Scholar]
- Skranes J. S., Vik T., Nilsen G., Smevik O., Andersson H. W., Brubakk A. M. Cerebral magnetic resonance imaging and mental and motor function of very low birth weight children at six years of age. Neuropediatrics. 1997 Jun;28(3):149–154. doi: 10.1055/s-2007-973692. [DOI] [PubMed] [Google Scholar]
- Toce S. S., Farrell P. M., Leavitt L. A., Samuels D. P., Edwards D. K. Clinical and roentgenographic scoring systems for assessing bronchopulmonary dysplasia. Am J Dis Child. 1984 Jun;138(6):581–585. doi: 10.1001/archpedi.1984.02140440065017. [DOI] [PubMed] [Google Scholar]
- Zinman R., Blanchard P. W., Vachon F. Oxygen saturation during sleep in patients with bronchopulmonary dysplasia. Biol Neonate. 1992;61(2):69–75. doi: 10.1159/000243533. [DOI] [PubMed] [Google Scholar]