Abstract
Objectives: To determine the incidence and study the causes and outcome of congenital brachial palsy (CBP).
Design: Active surveillance of newborn infants using the British Paediatric Surveillance Unit notification system and follow up study of outcome at 6 months of age.
Setting: The United Kingdom and Republic of Ireland.
Participants: Newborn infants presenting with a flaccid paresis of the arm (usually one, rarely both) born between April 1998 and March 1999.
Main outcome measures: Extent of the lesion at birth and degree of recovery at 6 months of age.
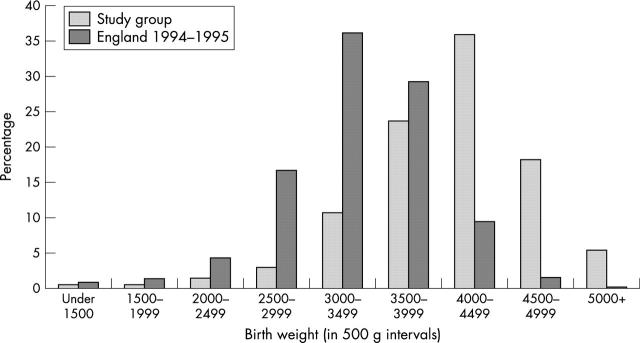
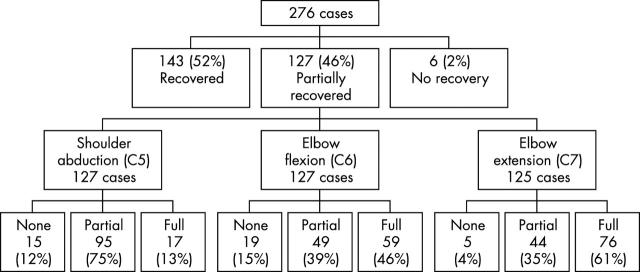
Findings: There were 323 confirmed cases giving an incidence of 0.42 per 1000 live births (1 in 2300). Significant associated risk factors in comparison with the normal population were shoulder dystocia (60% v 0.3%), high birth weight with 53% infants weighing more than the 90th centile, and assisted delivery (relative risk (RR) 3.4, 95% confidence interval (CI) 2.9 to 3.9, p = 0.0001). There was a considerably lower risk of CBP in infants delivered by caesarean section (RR 7, 95% CI 2 to 56, p = 0.002). At about 6 months of age, about half of the infants had recovered fully, but the remainder showed incomplete recovery including 2% with no recovery. The relative risk of partial or no recovery in infants with extensive lesions soon after birth compared with those with less extensive lesions was 11.28 (95% CI 2.38 to 63.66, p = 0.000005).
Conclusions: The incidence of CBP in the United Kingdom and Republic of Ireland is strikingly similar to that previously reported nearly 40 years ago. Most cases are due to trauma at delivery, which is not necessarily excessive or inappropriate. Given the uncertainty about the appropriate management of these infants, serious consideration should be given to a formal clinical trial of microsurgical nerve repair.
Full Text
The Full Text of this article is available as a PDF (157.8 KB).
Figure 1 .
Birth weight distribution.
Figure 2 .
Summary of outcomes.
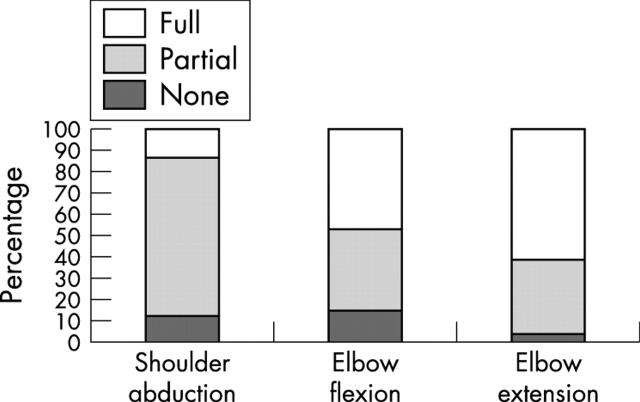
Figure 3 .
Pattern of recovery.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Adler J. B., Patterson R. L., Jr Erb's palsy. Long-term results of treatment in eighty-eight cases. J Bone Joint Surg Am. 1967 Sep;49(6):1052–1064. [PubMed] [Google Scholar]
- Bennet G. C., Harrold A. J. Prognosis and early management of birth injuries to the brachial plexus. Br Med J. 1976 Jun 19;1(6024):1520–1521. doi: 10.1136/bmj.1.6024.1520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birch R. Surgery for brachial plexus injuries. J Bone Joint Surg Br. 1993 May;75(3):346–348. doi: 10.1302/0301-620X.75B3.8496196. [DOI] [PubMed] [Google Scholar]
- Gairdner D., Pearson J. A growth chart for premature and other infants. Arch Dis Child. 1971 Dec;46(250):783–787. doi: 10.1136/adc.46.250.783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geutjens G., Gilbert A., Helsen K. Obstetric brachial plexus palsy associated with breech delivery. A different pattern of injury. J Bone Joint Surg Br. 1996 Mar;78(2):303–306. [PubMed] [Google Scholar]
- Gherman R. B., Ouzounian J. G., Goodwin T. M. Brachial plexus palsy: an in utero injury? Am J Obstet Gynecol. 1999 May;180(5):1303–1307. doi: 10.1016/s0002-9378(99)70633-2. [DOI] [PubMed] [Google Scholar]
- Gherman R. B., Ouzounian J. G., Miller D. A., Kwok L., Goodwin T. M. Spontaneous vaginal delivery: a risk factor for Erb's palsy? Am J Obstet Gynecol. 1998 Mar;178(3):423–427. doi: 10.1016/s0002-9378(98)70413-2. [DOI] [PubMed] [Google Scholar]
- Gonik B., Hollyer V. L., Allen R. Shoulder dystocia recognition: differences in neonatal risks for injury. Am J Perinatol. 1991 Jan;8(1):31–34. doi: 10.1055/s-2007-999334. [DOI] [PubMed] [Google Scholar]
- Gordon M., Rich H., Deutschberger J., Green M. The immediate and long-term outcome of obstetric birth trauma. I. Brachial plexus paralysis. Am J Obstet Gynecol. 1973 Sep 1;117(1):51–56. doi: 10.1016/0002-9378(73)90727-8. [DOI] [PubMed] [Google Scholar]
- Greenwald A. G., Schute P. C., Shiveley J. L. Brachial plexus birth palsy: a 10-year report on the incidence and prognosis. J Pediatr Orthop. 1984 Nov;4(6):689–692. doi: 10.1097/01241398-198411000-00006. [DOI] [PubMed] [Google Scholar]
- Jennett R. J., Tarby T. J. Brachial plexus palsy: an old problem revisited again. II. Cases in point. Am J Obstet Gynecol. 1997 Jun;176(6):1354–1357. doi: 10.1016/s0002-9378(97)70357-0. [DOI] [PubMed] [Google Scholar]
- Jennett R. J., Tarby T. J., Kreinick C. J. Brachial plexus palsy: an old problem revisited. Am J Obstet Gynecol. 1992 Jun;166(6 Pt 1):1673–1677. doi: 10.1016/0002-9378(92)91555-o. [DOI] [PubMed] [Google Scholar]
- Kay S. P. Obstetrical brachial palsy. Br J Plast Surg. 1998 Jan;51(1):43–50. doi: 10.1054/bjps.1997.0166. [DOI] [PubMed] [Google Scholar]
- Medlock M. D., Hanigan W. C. Neurologic birth trauma. Intracranial, spinal cord, and brachial plexus injury. Clin Perinatol. 1997 Dec;24(4):845–857. [PubMed] [Google Scholar]
- Michelow B. J., Clarke H. M., Curtis C. G., Zuker R. M., Seifu Y., Andrews D. F. The natural history of obstetrical brachial plexus palsy. Plast Reconstr Surg. 1994 Apr;93(4):675–681. [PubMed] [Google Scholar]
- Sadleir L. G., Connolly M. B. Acquired brachial-plexus neuropathy in the neonate: a rare presentation of late-onset group-B streptococcal osteomyelitis. Dev Med Child Neurol. 1998 Jul;40(7):496–499. doi: 10.1111/j.1469-8749.1998.tb15401.x. [DOI] [PubMed] [Google Scholar]
- Sjöberg I., Erichs K., Bjerre I. Cause and effect of obstetric (neonatal) brachial plexus palsy. Acta Paediatr Scand. 1988 May;77(3):357–364. doi: 10.1111/j.1651-2227.1988.tb10660.x. [DOI] [PubMed] [Google Scholar]
- Sjöberg I., Erichs K., Bjerre I. Cause and effect of obstetric (neonatal) brachial plexus palsy. Acta Paediatr Scand. 1988 May;77(3):357–364. doi: 10.1111/j.1651-2227.1988.tb10660.x. [DOI] [PubMed] [Google Scholar]
- Stewart R. E., Grossman D. M., Shulkin B. L., Shapiro B. Iodine-131 metaiodobenzylguanidine uptake in infantile myofibromatosis. Clin Nucl Med. 1989 May;14(5):344–346. doi: 10.1097/00003072-198905000-00007. [DOI] [PubMed] [Google Scholar]
- Wigglesworth J. S. Lesions in the neonatal brain. Arch Dis Child. 1985 Dec;60(12):1202–1203. doi: 10.1136/adc.60.12.1202-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- al-Qattan M. M., el-Sayed A. A., al-Kharfy T. M., al-Jurayyan N. A. Obstetrical brachial plexus injury in newborn babies delivered by caesarean section. J Hand Surg Br. 1996 Apr;21(2):263–265. doi: 10.1016/s0266-7681(96)80112-4. [DOI] [PubMed] [Google Scholar]