Abstract
Objective: To investigate the hypothesis that preterm infants who are more susceptible to lung damage have decreased neutrophil apoptosis, and to explore its relation to interleukin 10 (IL10) concentration.
Design: Prospective cohort design.
Patients: One hundred tracheal fluid specimens from 50 week-1 ventilated infants were examined for IL10 (by enzyme linked immunosorbent assay) and neutrophil apoptosis (by light microscopy).
Results: Neutrophil apoptosis was absent or less than 0.22% (median 0%) in the 11 infants with chronic lung disease (CLD) (24–31 weeks gestation) during the first 4 days of life. This was significantly lower than that of the 20 preterm infants without CLD (27–31 weeks gestation; median 0.47%, range 0–1.25%) and 19 term infants (median 0.5%, range 0–2.25%). There was an increase in apoptosis in infants with CLD (median 0.44%, p = 0.046) during days 5–7. Few infants without CLD were intubated beyond 4 days. Median apoptosis on days 5–7 was 0.26% and 2.78% for non-CLD preterm and term infants, but differences were not significant. IL10 concentration in tracheal fluid of infants with CLD was less than 5 pg/ml. None of the infants with IL10 greater than 5 pg/ml developed CLD. The range of IL10 concentrations in tracheal fluid from infants without CLD was wide (0–938 pg/ml). There was no apparent correlation between IL10 levels and percentage neutrophil apoptosis in infants without CLD.
Conclusion: Preterm infants with low levels of IL10 and neutrophil apoptosis may be predisposed to disordered lung repair. Further studies into the method of disposal of senescent neutrophils within preterm lungs are required.
Full Text
The Full Text of this article is available as a PDF (131.2 KB).
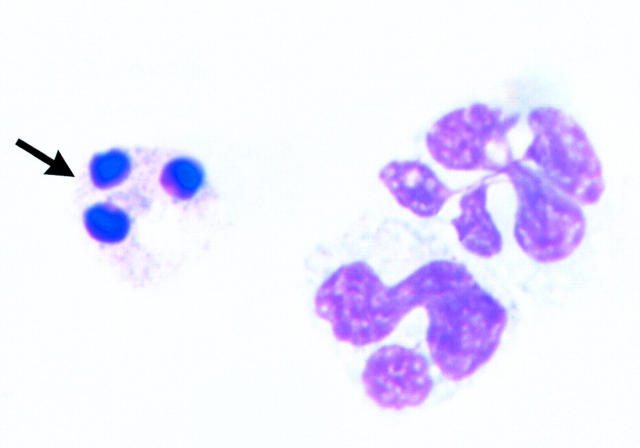
Figure 1 .
Neutrophil showing the characteristic changes of apoptosis (arrow) with densely condensed and rounded nuclear material.
Figure 2 .
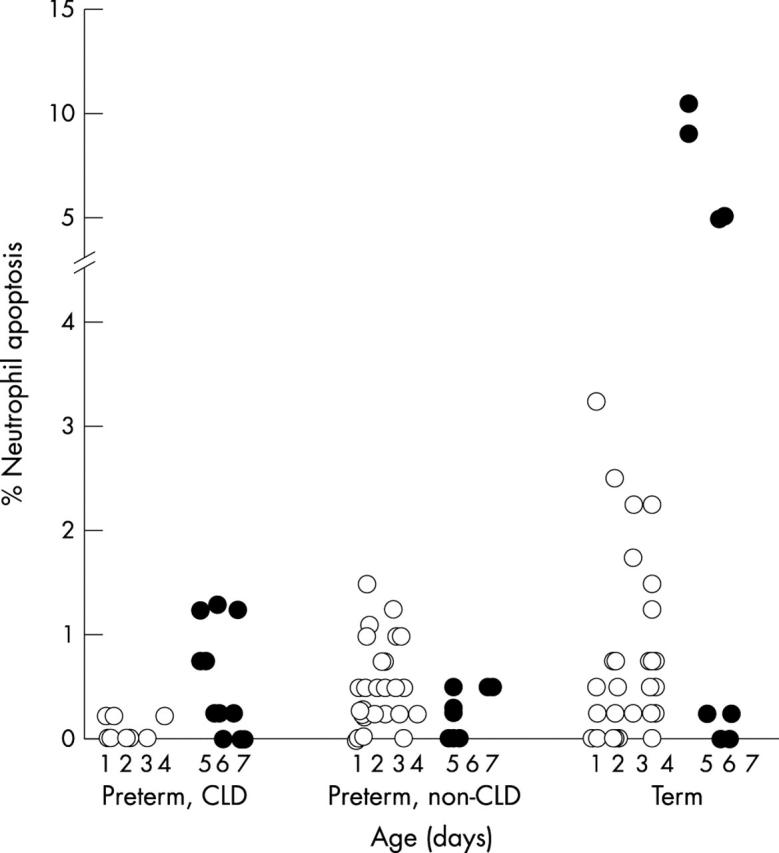
Percentage of neutrophils that are apoptotic in tracheal fluids of ventilated infants during the first week of life. Three groups of infants are shown: preterm infants with chronic lung disease (CLD), preterm infants without CLD, and term infants. Fewer tracheal fluid specimens were obtained beyond the first 4 days of life in non-CLD preterm and term infants (closed circles).
Figure 3 .
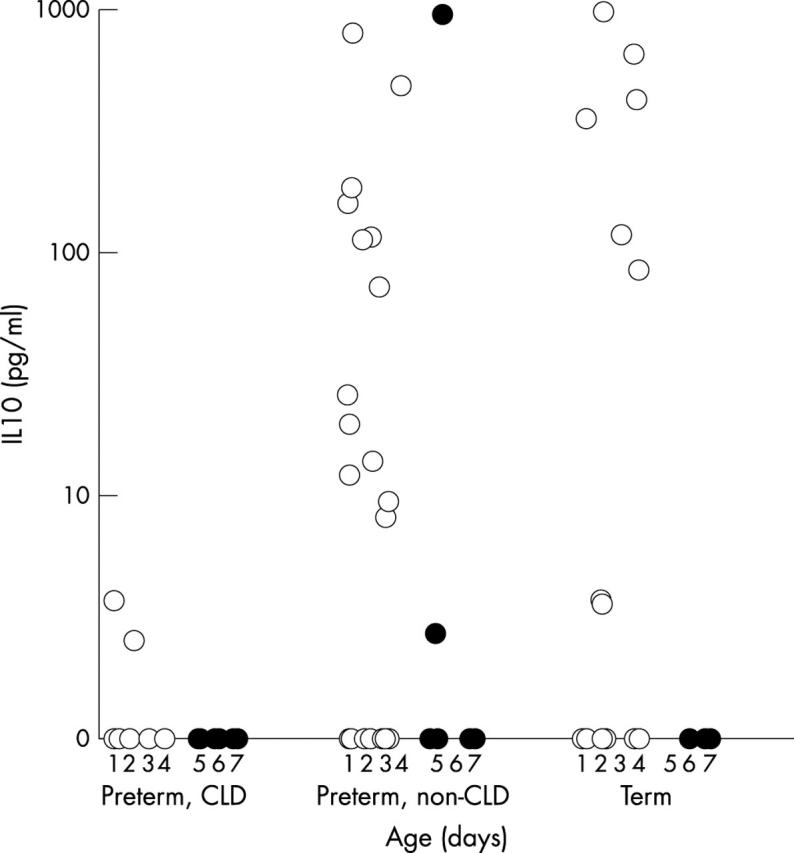
Interleukin 10 (IL10) in tracheal fluids of ventilated infants during the first week of life. IL10 concentrations are shown in log10 scale. Three groups of infants are shown: preterm infants with CLD, preterm without CLD, and term infants. Fewer tracheal fluid specimens were obtained beyond the first 4 days of life in non-CLD preterm and term infants (closed circles).
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Aoshiba K., Nagai A., Konno K. Erythromycin shortens neutrophil survival by accelerating apoptosis. Antimicrob Agents Chemother. 1995 Apr;39(4):872–877. doi: 10.1128/aac.39.4.872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arnon S., Grigg J., Silverman M. Pulmonary inflammatory cells in ventilated preterm infants: effect of surfactant treatment. Arch Dis Child. 1993 Jul;69(1 Spec No):44–48. doi: 10.1136/adc.69.1_spec_no.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biffl W. L., Moore E. E., Moore F. A., Barnett C. C., Jr, Carl V. S., Peterson V. N. Interleukin-6 delays neutrophil apoptosis. Arch Surg. 1996 Jan;131(1):24–30. doi: 10.1001/archsurg.1996.01430130026005. [DOI] [PubMed] [Google Scholar]
- Borish L., Aarons A., Rumbyrt J., Cvietusa P., Negri J., Wenzel S. Interleukin-10 regulation in normal subjects and patients with asthma. J Allergy Clin Immunol. 1996 Jun;97(6):1288–1296. doi: 10.1016/s0091-6749(96)70197-5. [DOI] [PubMed] [Google Scholar]
- Cassatella M. A., Meda L., Bonora S., Ceska M., Constantin G. Interleukin 10 (IL-10) inhibits the release of proinflammatory cytokines from human polymorphonuclear leukocytes. Evidence for an autocrine role of tumor necrosis factor and IL-1 beta in mediating the production of IL-8 triggered by lipopolysaccharide. J Exp Med. 1993 Dec 1;178(6):2207–2211. doi: 10.1084/jem.178.6.2207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chmiel J. F., Konstan M. W., Knesebeck J. E., Hilliard J. B., Bonfield T. L., Dawson D. V., Berger M. IL-10 attenuates excessive inflammation in chronic Pseudomonas infection in mice. Am J Respir Crit Care Med. 1999 Dec;160(6):2040–2047. doi: 10.1164/ajrccm.160.6.9901043. [DOI] [PubMed] [Google Scholar]
- Cox G., Crossley J., Xing Z. Macrophage engulfment of apoptotic neutrophils contributes to the resolution of acute pulmonary inflammation in vivo. Am J Respir Cell Mol Biol. 1995 Feb;12(2):232–237. doi: 10.1165/ajrcmb.12.2.7865221. [DOI] [PubMed] [Google Scholar]
- Cox G. Glucocorticoid treatment inhibits apoptosis in human neutrophils. Separation of survival and activation outcomes. J Immunol. 1995 May 1;154(9):4719–4725. [PubMed] [Google Scholar]
- Deneke S. M., Fanburg B. L. Normobaric oxygen toxicity of the lung. N Engl J Med. 1980 Jul 10;303(2):76–86. doi: 10.1056/NEJM198007103030204. [DOI] [PubMed] [Google Scholar]
- Donnelly S. C., Strieter R. M., Reid P. T., Kunkel S. L., Burdick M. D., Armstrong I., Mackenzie A., Haslett C. The association between mortality rates and decreased concentrations of interleukin-10 and interleukin-1 receptor antagonist in the lung fluids of patients with the adult respiratory distress syndrome. Ann Intern Med. 1996 Aug 1;125(3):191–196. doi: 10.7326/0003-4819-125-3-199608010-00005. [DOI] [PubMed] [Google Scholar]
- Dransfield I., Stocks S. C., Haslett C. Regulation of cell adhesion molecule expression and function associated with neutrophil apoptosis. Blood. 1995 Jun 1;85(11):3264–3273. [PubMed] [Google Scholar]
- Grigg J. M., Savill J. S., Sarraf C., Haslett C., Silverman M. Neutrophil apoptosis and clearance from neonatal lungs. Lancet. 1991 Sep 21;338(8769):720–722. doi: 10.1016/0140-6736(91)91443-x. [DOI] [PubMed] [Google Scholar]
- Groneck P., Götze-Speer B., Oppermann M., Eiffert H., Speer C. P. Association of pulmonary inflammation and increased microvascular permeability during the development of bronchopulmonary dysplasia: a sequential analysis of inflammatory mediators in respiratory fluids of high-risk preterm neonates. Pediatrics. 1994 May;93(5):712–718. [PubMed] [Google Scholar]
- Henderson-Smart D. J., Davis P. G. Prophylactic methylxanthine for extubation in preterm infants. Cochrane Database Syst Rev. 2000;(2):CD000139–CD000139. doi: 10.1002/14651858.CD000139. [DOI] [PubMed] [Google Scholar]
- Hussain N., Wu F., Zhu L., Thrall R. S., Kresch M. J. Neutrophil apoptosis during the development and resolution of oleic acid-induced acute lung injury in the rat. Am J Respir Cell Mol Biol. 1998 Dec;19(6):867–874. doi: 10.1165/ajrcmb.19.6.3118. [DOI] [PubMed] [Google Scholar]
- Ishii Y., Hashimoto K., Nomura A., Sakamoto T., Uchida Y., Ohtsuka M., Hasegawa S., Sagai M. Elimination of neutrophils by apoptosis during the resolution of acute pulmonary inflammation in rats. Lung. 1998;176(2):89–98. doi: 10.1007/pl00007597. [DOI] [PubMed] [Google Scholar]
- Jones C. A., Cayabyab R. G., Kwong K. Y., Stotts C., Wong B., Hamdan H., Minoo P., deLemos R. A. Undetectable interleukin (IL)-10 and persistent IL-8 expression early in hyaline membrane disease: a possible developmental basis for the predisposition to chronic lung inflammation in preterm newborns. Pediatr Res. 1996 Jun;39(6):966–975. doi: 10.1203/00006450-199606000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jónsson B., Li Y. H., Noack G., Brauner A., Tullus K. Downregulatory cytokines in tracheobronchial aspirate fluid from infants with chronic lung disease of prematurity. Acta Paediatr. 2000 Nov;89(11):1375–1380. doi: 10.1080/080352500300002606. [DOI] [PubMed] [Google Scholar]
- Jónsson B., Tullus K., Brauner A., Lu Y., Noack G. Early increase of TNF alpha and IL-6 in tracheobronchial aspirate fluid indicator of subsequent chronic lung disease in preterm infants. Arch Dis Child Fetal Neonatal Ed. 1997 Nov;77(3):F198–F201. doi: 10.1136/fn.77.3.f198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kunkel S. L., Standiford T., Kasahara K., Strieter R. M. Interleukin-8 (IL-8): the major neutrophil chemotactic factor in the lung. Exp Lung Res. 1991 Jan-Feb;17(1):17–23. doi: 10.3109/01902149109063278. [DOI] [PubMed] [Google Scholar]
- Liu Y., Cousin J. M., Hughes J., Van Damme J., Seckl J. R., Haslett C., Dransfield I., Savill J., Rossi A. G. Glucocorticoids promote nonphlogistic phagocytosis of apoptotic leukocytes. J Immunol. 1999 Mar 15;162(6):3639–3646. [PubMed] [Google Scholar]
- McColm J. R., Stenson B. J., Biermasz N., McIntosh N. Measurement of interleukin 10 in bronchoalveolar lavage from preterm ventilated infants. Arch Dis Child Fetal Neonatal Ed. 2000 Mar;82(2):F156–F159. doi: 10.1136/fn.82.2.F156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munshi U. K., Niu J. O., Siddiq M. M., Parton L. A. Elevation of interleukin-8 and interleukin-6 precedes the influx of neutrophils in tracheal aspirates from preterm infants who develop bronchopulmonary dysplasia. Pediatr Pulmonol. 1997 Nov;24(5):331–336. doi: 10.1002/(sici)1099-0496(199711)24:5<331::aid-ppul5>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- Ogden B. E., Murphy S. A., Saunders G. C., Pathak D., Johnson J. D. Neonatal lung neutrophils and elastase/proteinase inhibitor imbalance. Am Rev Respir Dis. 1984 Nov;130(5):817–821. doi: 10.1164/arrd.1984.130.5.817. [DOI] [PubMed] [Google Scholar]
- Robertson B. The evolution of neonatal respiratory distress syndrome into chronic lung disease. Eur Respir J Suppl. 1989 Mar;3:33s–37s. [PubMed] [Google Scholar]
- Saraste A. Morphologic criteria and detection of apoptosis. Herz. 1999 May;24(3):189–195. doi: 10.1007/BF03044961. [DOI] [PubMed] [Google Scholar]
- Savill J. S., Wyllie A. H., Henson J. E., Walport M. J., Henson P. M., Haslett C. Macrophage phagocytosis of aging neutrophils in inflammation. Programmed cell death in the neutrophil leads to its recognition by macrophages. J Clin Invest. 1989 Mar;83(3):865–875. doi: 10.1172/JCI113970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shennan A. T., Dunn M. S., Ohlsson A., Lennox K., Hoskins E. M. Abnormal pulmonary outcomes in premature infants: prediction from oxygen requirement in the neonatal period. Pediatrics. 1988 Oct;82(4):527–532. [PubMed] [Google Scholar]
- Smith J. A. Neutrophils, host defense, and inflammation: a double-edged sword. J Leukoc Biol. 1994 Dec;56(6):672–686. doi: 10.1002/jlb.56.6.672. [DOI] [PubMed] [Google Scholar]
- Stern M., Savill J., Haslett C. Human monocyte-derived macrophage phagocytosis of senescent eosinophils undergoing apoptosis. Mediation by alpha v beta 3/CD36/thrombospondin recognition mechanism and lack of phlogistic response. Am J Pathol. 1996 Sep;149(3):911–921. [PMC free article] [PubMed] [Google Scholar]
- Wang P., Wu P., Anthes J. C., Siegel M. I., Egan R. W., Billah M. M. Interleukin-10 inhibits interleukin-8 production in human neutrophils. Blood. 1994 May 1;83(9):2678–2683. [PubMed] [Google Scholar]
- Whyte M. K., Meagher L. C., MacDermot J., Haslett C. Impairment of function in aging neutrophils is associated with apoptosis. J Immunol. 1993 Jun 1;150(11):5124–5134. [PubMed] [Google Scholar]
- Yasui K., Hu B., Nakazawa T., Agematsu K., Komiyama A. Theophylline accelerates human granulocyte apoptosis not via phosphodiesterase inhibition. J Clin Invest. 1997 Oct 1;100(7):1677–1684. doi: 10.1172/JCI119692. [DOI] [PMC free article] [PubMed] [Google Scholar]