Abstract
Background: Noise exposure in neonatal units has long been suspected of being a cause of hearing loss associated with such units. The noise intensity to which the neonate is exposed varies with the type of ventilatory support used. Also, the post-nasal space is an enclosed cavity that is close to the inner ear and an area of turbulent and hence potentially noisy airflow.
Aim: To determine noise intensities within the ear and post-nasal space in neonates on different modes of ventilatory support using probe microphones, measures previously not undertaken.
Methods: A portable instrument with a probe microphone was used for the measurements. Three groups of infants were included: (a) those receiving no respiratory support (NS); (b) those receiving conventional ventilation (CV); (c) those receiving continuous positive airways pressure (CPAP) support.
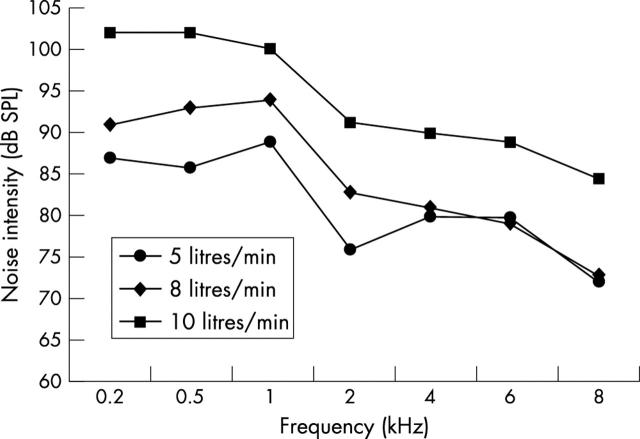
Results: The mean in-the-ear noise intensities (at 1 kHz) were 41.7 dB SPL (NS), 39.5 dB SPL (CV), and 55.1 dB SPL (CPAP). The noise intensities in the post-nasal space in those receiving CPAP support were higher than in the other groups, reached mean levels of up to 102 dB SPL at some frequencies, and increased with increasing flow rates.
Conclusions: The most important finding is the high noise intensities in the post-nasal space of those receiving CPAP support. Given the proximity of the post-nasal space to the inner ear, enough noise could be transmitted, especially in infants receiving the higher flow rates, to cause cochlear damage and hence hearing loss. It would therefore be wise, wherever possible, to avoid using the higher flow rates.
Full Text
The Full Text of this article is available as a PDF (103.0 KB).
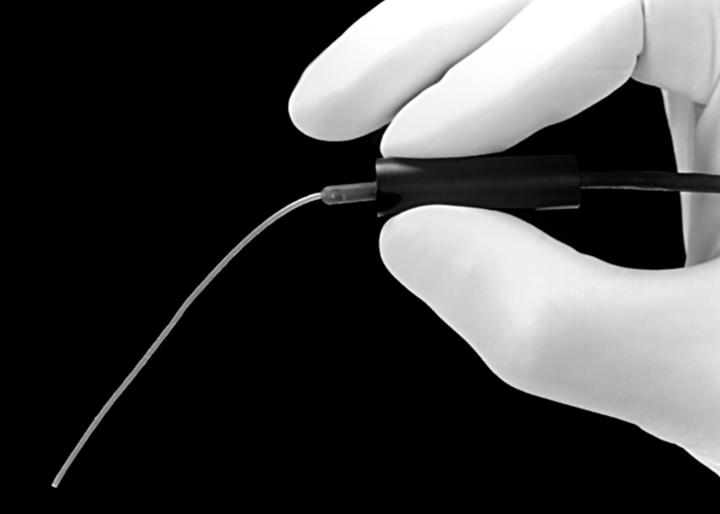
Figure 1 .
Probe microphone/tube used to measure noise intensity.
Figure 2 .
Graphical representation of increase in post-nasal noise intensity for selected flow rates.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Benini F., Magnavita V., Lago P., Arslan E., Pisan P. Evaluation of noise in the neonatal intensive care unit. Am J Perinatol. 1996 Jan;13(1):37–41. doi: 10.1055/s-2007-994200. [DOI] [PubMed] [Google Scholar]
- Bess F. H., Peek B. F., Chapman J. J. Further observations on noise levels in infant incubators. Pediatrics. 1979 Jan;63(1):100–106. [PubMed] [Google Scholar]
- Borg E. Perinatal asphyxia, hypoxia, ischemia and hearing loss. An overview. Scand Audiol. 1997;26(2):77–91. doi: 10.3109/01050399709074979. [DOI] [PubMed] [Google Scholar]
- Committee on Environmental Hazards. Noise pollution: neonatal aspects. Pediatrics. 1974 Oct;54(4):476–479. [PubMed] [Google Scholar]
- Das V. K. Adverse perinatal factors in the causation of sensorineural hearing impairment in young children. Int J Pediatr Otorhinolaryngol. 1991 Apr;21(2):121–125. doi: 10.1016/0165-5876(91)90142-x. [DOI] [PubMed] [Google Scholar]
- Davis A., Wood S. The epidemiology of childhood hearing impairment: factor relevant to planning of services. Br J Audiol. 1992 Apr;26(2):77–90. doi: 10.3109/03005369209077875. [DOI] [PubMed] [Google Scholar]
- Dayal V. S., Kokshanian A., Mitchell D. P. Combined effects of noise and kanamycin. Ann Otol Rhinol Laryngol. 1971 Dec;80(6):897–902. doi: 10.1177/000348947108000616. [DOI] [PubMed] [Google Scholar]
- Douek E., Dodson H. C., Bannister L. H., Ashcroft P., Humphries K. N. Effects of incubator noise on the cochlea of the newborn. Lancet. 1976 Nov 20;2(7995):1110–1113. doi: 10.1016/s0140-6736(76)91088-6. [DOI] [PubMed] [Google Scholar]
- Falk S. A., Cook R. O., Haseman J. K., Sanders G. M. Noise-induced inner ear damage in newborn and adult guinea pigs. Laryngoscope. 1974 Mar;84(3):444–453. doi: 10.1288/00005537-197403000-00008. [DOI] [PubMed] [Google Scholar]
- Falk S. A., Farmer J. C., Jr Incubator noise and possible deafness. Arch Otolaryngol. 1973 May;97(5):385–387. doi: 10.1001/archotol.1973.00780010397006. [DOI] [PubMed] [Google Scholar]
- Falk S. A., Woods N. F. Hospital noise--levels and potential health hazards. N Engl J Med. 1973 Oct 11;289(15):774–781. doi: 10.1056/NEJM197310112891504. [DOI] [PubMed] [Google Scholar]
- Field T. Alleviating stress in newborn infants in the intensive care unit. Clin Perinatol. 1990 Mar;17(1):1–9. [PubMed] [Google Scholar]
- Geber W. F., Anderson T. A., Van Dyne B. Physiologic responses of the albino rat to chronic noise stress. Arch Environ Health. 1966 Jun;12(6):751–754. doi: 10.1080/00039896.1966.10664476. [DOI] [PubMed] [Google Scholar]
- Gädeke R., Döring B., Keller F., Vogel A. The noise level in a childrens hospital and the wake-up threshold in infants. Acta Paediatr Scand. 1969 Mar;58(2):164–170. doi: 10.1111/j.1651-2227.1969.tb04701.x. [DOI] [PubMed] [Google Scholar]
- Kruger B., Ruben R. J. The acoustic properties of the infant ear. A preliminary report. Acta Otolaryngol. 1987 May-Jun;103(5-6):578–585. [PubMed] [Google Scholar]
- Lenoir M., Pujol R. Sensitive period to acoustic trauma in the rat pup cochlea. Histological findings. Acta Otolaryngol. 1980 Mar-Apr;89(3-4):317–322. doi: 10.3109/00016488009127143. [DOI] [PubMed] [Google Scholar]
- Saunders J. C., Chen C. S. Sensitive periods of susceptibility to auditory trauma in mammals. Environ Health Perspect. 1982 Apr;44:63–66. doi: 10.1289/ehp.824463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zahr L. K., de Traversay J. Premature infant responses to noise reduction by earmuffs: effects on behavioral and physiologic measures. J Perinatol. 1995 Nov-Dec;15(6):448–455. [PubMed] [Google Scholar]