Abstract
Objective: To study the incidence and outcome of systemic infections with methicillin sensitive (MSSA) and methicillin resistant Staphylococcus aureus (MRSA) infections in Australasian neonatal nurseries.
Methods: Prospective longitudinal study of systemic infections (clinical sepsis plus positive cultures of blood and/or cerebrospinal fluid) in 17 Australasian neonatal nurseries.
Results: The incidence of early onset sepsis with S aureus, mainly MSSA, was 19 cases per 244 718 live births or 0.08 per 1000. From 1992 to 1994, MRSA infections caused only 8% of staphylococcal infections. From 1995 to 1998, there was an outbreak of MRSA infection, in two Melbourne hospitals. The outbreak resolved, after the use of topical mupirocin and improved handwashing. Babies with MRSA sepsis were significantly smaller than babies with MSSA sepsis (mean birth weight 1093 v 1617 g) and more preterm (mean gestation 27.5 v 30.3 weeks). The mortality of MRSA sepsis was 24.6% compared with 9.9% for MSSA infections. The mortality of early onset MSSA sepsis, however, was 39% (seven of 18) compared with 7.3% of late onset MSSA infection presenting more than two days after birth.
Conclusions: S aureus is a rare but important cause of early onset sepsis. Late onset MRSA infections carried a higher mortality than late onset MSSA infections, but babies with early onset MSSA sepsis had a particularly high mortality.
Full Text
The Full Text of this article is available as a PDF (160.7 KB).
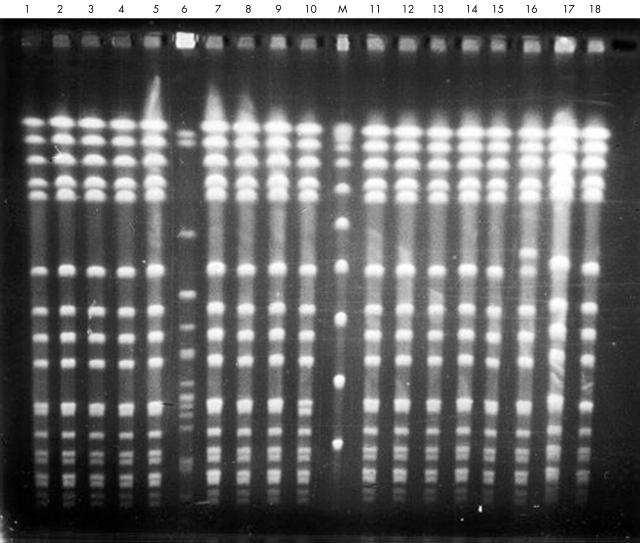
Figure 1.
Local incidence and mortality of systemic infections due to Staphylococcus aureus which are methicillin sensitive (MSSA) or methicillin resistant (MRSA). Hospitals A, B, and C are three different Melbourne hospitals.
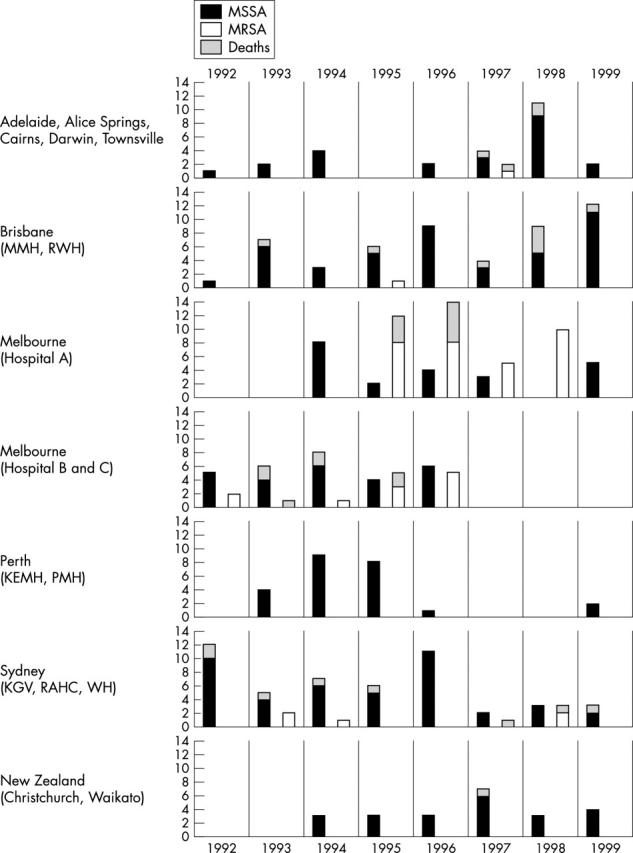
Figure 2.
Pulsed field gel electrophoresis of strains of methicillin resistant Staphylococcus aureus (MRSA). DNA from 18 MRSA isolates digested with SmaI and separated at 6 V/cm for 22 hours with a switch time of 5–25 seconds. Lane marked M, Lambda DNA ladder. Isolates 1–5, 7–15, 17 and 18 showed identical patterns.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Back N. A., Linnemann C. C., Jr, Staneck J. L., Kotagal U. R. Control of methicillin-resistant Staphylococcus aureus in a neonatal intensive-care unit: use of intensive microbiologic surveillance and mupirocin. Infect Control Hosp Epidemiol. 1996 Apr;17(4):227–231. doi: 10.1086/647285. [DOI] [PubMed] [Google Scholar]
- Barakate M. S., Yang Y. X., Foo S. H., Vickery A. M., Sharp C. A., Fowler L. D., Harris J. P., West R. H., Macleod C., Benn R. A. An epidemiological survey of methicillin-resistant Staphylococcus aureus in a tertiary referral hospital. J Hosp Infect. 2000 Jan;44(1):19–26. doi: 10.1053/jhin.1999.0635. [DOI] [PubMed] [Google Scholar]
- Cheong I., Tan S. C., Wong Y. H., Zainudin B. M., Rahman M. Z. Methicillin-resistant Staphylococcus aureus (mrsa) in a Malaysian hospital. Med J Malaysia. 1994 Mar;49(1):24–28. [PubMed] [Google Scholar]
- Davies E. A., Emmerson A. M., Hogg G. M., Patterson M. F., Shields M. D. An outbreak of infection with a methicillin-resistant Staphylococcus aureus in a special care baby unit: value of topical mupirocin and of traditional methods of infection control. J Hosp Infect. 1987 Sep;10(2):120–128. doi: 10.1016/0195-6701(87)90137-x. [DOI] [PubMed] [Google Scholar]
- Givney R., Vickery A., Holliday A., Pegler M., Benn R. Evolution of an endemic methicillin-resistant Staphylococcus aureus population in an Australian hospital from 1967 to 1996. J Clin Microbiol. 1998 Feb;36(2):552–556. doi: 10.1128/jcm.36.2.552-556.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gottlieb T., Mitchell D. The independent evolution of resistance to ciprofloxacin, rifampicin, and fusidic acid in methicillin-resistant Staphylococcus aureus in Australian teaching hospitals (1990-1995). Australian Group for Antimicrobial Resistance (AGAR). J Antimicrob Chemother. 1998 Jul;42(1):67–73. doi: 10.1093/jac/42.1.67. [DOI] [PubMed] [Google Scholar]
- Haddad Q., Sobayo E. I., Basit O. B., Rotimi V. O. Outbreak of methicillin-resistant Staphylococcus aureus in a neonatal intensive care unit. J Hosp Infect. 1993 Mar;23(3):211–222. doi: 10.1016/0195-6701(93)90026-v. [DOI] [PubMed] [Google Scholar]
- Haley R. W., Bregman D. A. The role of understaffing and overcrowding in recurrent outbreaks of staphylococcal infection in a neonatal special-care unit. J Infect Dis. 1982 Jun;145(6):875–885. doi: 10.1093/infdis/145.6.875. [DOI] [PubMed] [Google Scholar]
- Haley R. W., Cushion N. B., Tenover F. C., Bannerman T. L., Dryer D., Ross J., Sánchez P. J., Siegel J. D. Eradication of endemic methicillin-resistant Staphylococcus aureus infections from a neonatal intensive care unit. J Infect Dis. 1995 Mar;171(3):614–624. doi: 10.1093/infdis/171.3.614. [DOI] [PubMed] [Google Scholar]
- Heffernan H., Stehr-Green J., Davies H., Brett M., Bowers S. Methicillin resistant Staphylococcus aureus (MRSA) in New Zealand 1988-90. N Z Med J. 1993 Mar 10;106(951):72–74. [PubMed] [Google Scholar]
- Isaacs D., Barfield C. P., Grimwood K., McPhee A. J., Minutillo C., Tudehope D. I. Systemic bacterial and fungal infections in infants in Australian neonatal units. Australian Study Group for Neonatal Infections. Med J Aust. 1995 Feb 20;162(4):198–201. doi: 10.5694/j.1326-5377.1995.tb126024.x. [DOI] [PubMed] [Google Scholar]
- Ish-Horowicz M. R., McIntyre P., Nade S. Bone and joint infections caused by multiply resistant Staphylococcus aureus in a neonatal intensive care unit. Pediatr Infect Dis J. 1992 Feb;11(2):82–87. doi: 10.1097/00006454-199202000-00005. [DOI] [PubMed] [Google Scholar]
- Jernigan J. A., Titus M. G., Gröschel D. H., Getchell-White S., Farr B. M. Effectiveness of contact isolation during a hospital outbreak of methicillin-resistant Staphylococcus aureus. Am J Epidemiol. 1996 Mar 1;143(5):496–504. doi: 10.1093/oxfordjournals.aje.a008770. [DOI] [PubMed] [Google Scholar]
- Johnson Z., Fitzpatrick P., Hayes C., Sayers G., Pelly H., McDonnell B., Thornton L., Buttimer J. National survey of MRSA: Ireland, 1995. J Hosp Infect. 1997 Mar;35(3):175–184. doi: 10.1016/s0195-6701(97)90205-x. [DOI] [PubMed] [Google Scholar]
- Liu C. C., Hor L. I., Wu Y. H., Huang A. H., Lin C. H., Chuang Y. C. Investigation and elimination of epidemic methicillin-resistant Staphylococcus aureus in a neonatal intensive care unit. Zhonghua Min Guo Xiao Er Ke Yi Xue Hui Za Zhi. 1993 Jul-Aug;34(4):285–293. [PubMed] [Google Scholar]
- Marty L., Flahault A., Suarez B., Caillon J., Hill C., Andremont A. Resistance to methicillin and virulence of Staphylococcus aureus strains in bacteriemic cancer patients. Intensive Care Med. 1993;19(5):285–289. doi: 10.1007/BF01690549. [DOI] [PubMed] [Google Scholar]
- McDonald M. The epidemiology of methicillin-resistant Staphylococcus aureus: surgical relevance 20 years on. Aust N Z J Surg. 1997 Oct;67(10):682–685. doi: 10.1111/j.1445-2197.1997.tb07108.x. [DOI] [PubMed] [Google Scholar]
- Millar M. R., Keyworth N., Lincoln C., King B., Congdon P. 'Methicillin-resistant' Staphylococcus aureus in a regional neonatology unit. J Hosp Infect. 1987 Sep;10(2):187–197. doi: 10.1016/0195-6701(87)90146-0. [DOI] [PubMed] [Google Scholar]
- Mitsuda T., Arai K., Ibe M., Imagawa T., Tomono N., Yokota S. The influence of methicillin-resistant Staphylococcus aureus (MRSA) carriers in a nursery and transmission of MRSA to their households. J Hosp Infect. 1999 May;42(1):45–51. doi: 10.1053/jhin.1998.0551. [DOI] [PubMed] [Google Scholar]
- Morgan M., Salmon R., Evans-Williams D., Hosein I., Looker D. N. Resistance to methicillin in isolates of Staphylococcus aureus from blood and cerebrospinal fluid in Wales, 1993-1997. J Antimicrob Chemother. 1999 Oct;44(4):541–544. doi: 10.1093/jac/44.4.541. [DOI] [PubMed] [Google Scholar]
- Nada T., Ichiyama S., Iinuma Y., Inuzuka K., Washida H., Ohta M., Shimokata K., Kato N., Nakashima N. Types of methicillin-resistant Staphylococcus aureus associated with high mortality in patients with bacteremia. Eur J Clin Microbiol Infect Dis. 1996 Apr;15(4):340–343. doi: 10.1007/BF01695669. [DOI] [PubMed] [Google Scholar]
- Stoll B. J., Gordon T., Korones S. B., Shankaran S., Tyson J. E., Bauer C. R., Fanaroff A. A., Lemons J. A., Donovan E. F., Oh W. Early-onset sepsis in very low birth weight neonates: a report from the National Institute of Child Health and Human Development Neonatal Research Network. J Pediatr. 1996 Jul;129(1):72–80. doi: 10.1016/s0022-3476(96)70192-0. [DOI] [PubMed] [Google Scholar]
- Storch G. A., Rajagopalan L. Methicillin-resistant Staphylococcus aureus bacteremia in children. Pediatr Infect Dis. 1986 Jan-Feb;5(1):59–67. doi: 10.1097/00006454-198601000-00012. [DOI] [PubMed] [Google Scholar]
- Tan K. W., Tay L., Lim S. H. An outbreak of methicillin-resistant Staphylococcus aureus in a neonatal intensive care unit in Singapore: a 20-month study of clinical characteristics and control. Singapore Med J. 1994 Jun;35(3):277–282. [PubMed] [Google Scholar]
- Wong M., Isaacs D., Howman-Giles R., Uren R. Clinical and diagnostic features of osteomyelitis occurring in the first three months of life. Pediatr Infect Dis J. 1995 Dec;14(12):1047–1053. doi: 10.1097/00006454-199512000-00004. [DOI] [PubMed] [Google Scholar]
- Zafar A. B., Butler R. C., Reese D. J., Gaydos L. A., Mennonna P. A. Use of 0.3% triclosan (Bacti-Stat) to eradicate an outbreak of methicillin-resistant Staphylococcus aureus in a neonatal nursery. Am J Infect Control. 1995 Jun;23(3):200–208. doi: 10.1016/0196-6553(95)90042-x. [DOI] [PubMed] [Google Scholar]