Abstract
Aims: To establish a practical postnatal reference range for cardiac troponin T in neonates and to investigate concentrations in neonates with respiratory distress.
Methods: Prospective investigation in a tertiary neonatal unit, recruiting infants with and without respiratory distress (sick and healthy infants respectively). Concentrations of cardiac troponin T were compared between sick and healthy infants, accounting for confounding variables.
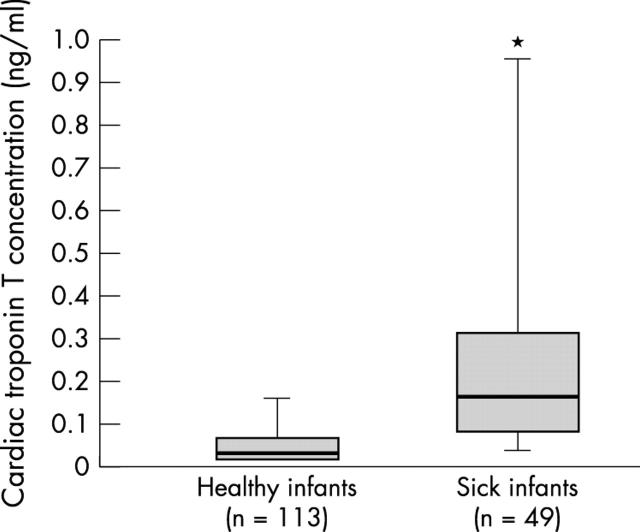
Results: A total of 162 neonates (113 healthy and 49 sick infants) had samples taken. The median (interquartile range) cardiac troponin T concentration in the healthy infants was 0.025 (0.01–0.062) ng/ml, and the 95th centile was 0.153 ng/ml. There were no significant relations between cardiac troponin T and various variables. The median (interquartile range) cardiac troponin T concentration in the sick infants was 0.159 (0.075–0.308) ng/ml. This was significantly higher (p < 0.0001) than in the healthy infants. In a linear regression model, the use of inotropes and oxygen requirement were significant associations independent of other basic and clinical variables in explaining the variation in cardiac troponin T concentrations.
Conclusions: Cardiac troponin T is detectable in the blood of many healthy neonates, but no relation with important basic and clinical variables was found. Sick infants have significantly higher concentrations than healthy infants. The variations in cardiac troponin T concentration were significantly associated with oxygen requirement or the use of inotropic support in a regression model. Cardiac troponin T may be a useful marker of neonatal and cardiorespiratory morbidity.
Full Text
The Full Text of this article is available as a PDF (89.7 KB).
Figure 1.
Distribution of postnatal cardiac troponin T concentrations for sick and healthy infants. Whiskers are 5th and 95th centiles. The grey box is the interquartile range, and the dark line in the middle of the grey box is the median value. *p < 0.0001 compared with healthy infants.
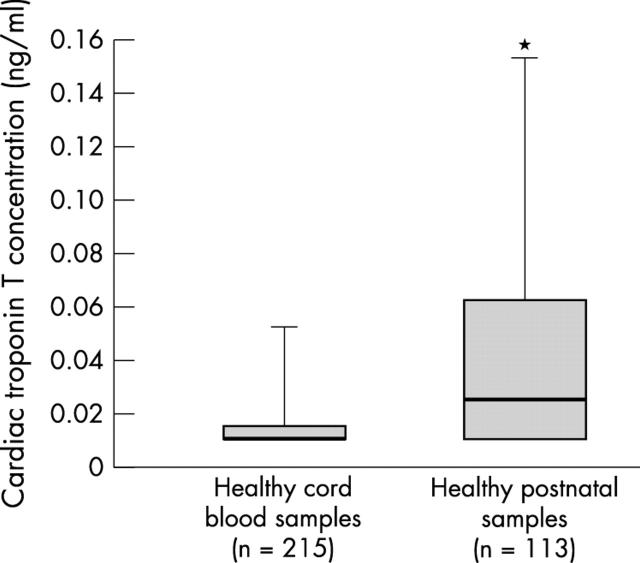
Figure 2.
Distribution of cardiac troponin T concentrations for healthy infants with cord blood samples on the left and healthy postnatal samples on the right. Whiskers are 5th and 95th centiles. The grey box is the interquartile range and the dark line in the middle of the grey box is the median value. *p < 0.0001 compared with healthy cord blood samples.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Adamcová M., Kokstein Z., Palicka V., Podholová M., Kostál M. Troponin T levels in the cord blood of healthy term neonates. Physiol Res. 1995;44(2):99–104. [PubMed] [Google Scholar]
- Adamcová M., Kokstein Z., Palicka V., Vávrová J., Kostál M., Podholová M., Kalous P. Cardiac troponin T in pregnant women having intravenous tocolytic therapy. Arch Gynecol Obstet. 1999;262(3-4):121–126. doi: 10.1007/s004040050239. [DOI] [PubMed] [Google Scholar]
- Bhayana V., Henderson A. R. Biochemical markers of myocardial damage. Clin Biochem. 1995 Feb;28(1):1–29. doi: 10.1016/0009-9120(94)00065-4. [DOI] [PubMed] [Google Scholar]
- Bodor G. S., Survant L., Voss E. M., Smith S., Porterfield D., Apple F. S. Cardiac troponin T composition in normal and regenerating human skeletal muscle. Clin Chem. 1997 Mar;43(3):476–484. [PubMed] [Google Scholar]
- Clark S. J., Newland P., Yoxall C. W., Subhedar N. V. Cardiac troponin T in cord blood. Arch Dis Child Fetal Neonatal Ed. 2001 Jan;84(1):F34–F37. doi: 10.1136/fn.84.1.F34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collinson P. O., Premachandram S., Hashemi K. Prospective audit of incidence of prognostically important myocardial damage in patients discharged from emergency department. BMJ. 2000 Jun 24;320(7251):1702–1705. doi: 10.1136/bmj.320.7251.1702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham S., Symon A. G., Elton R. A., Zhu C., McIntosh N. Intra-arterial blood pressure reference ranges, death and morbidity in very low birthweight infants during the first seven days of life. Early Hum Dev. 1999 Dec;56(2-3):151–165. doi: 10.1016/s0378-3782(99)00038-9. [DOI] [PubMed] [Google Scholar]
- Finley J. P., Howman-Giles R. B., Gilday D. L., Bloom K. R., Rowe R. D. Transient myocardial ischemia of the newborn infant demonstrated by thallium myocardial imaging. J Pediatr. 1979 Feb;94(2):263–270. doi: 10.1016/s0022-3476(79)80841-0. [DOI] [PubMed] [Google Scholar]
- Gill A. B., Weindling A. M. Echocardiographic assessment of cardiac function in shocked very low birthweight infants. Arch Dis Child. 1993 Jan;68(1 Spec No):17–21. doi: 10.1136/adc.68.1_spec_no.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein R. F., Thompson R. J., Jr, Oehler J. M., Brazy J. E. Influence of acidosis, hypoxemia, and hypotension on neurodevelopmental outcome in very low birth weight infants. Pediatrics. 1995 Feb;95(2):238–243. [PubMed] [Google Scholar]
- Hetland O., Dickstein K. Cardiac troponins I and T in patients with suspected acute coronary syndrome: a comparative study in a routine setting. Clin Chem. 1998 Jul;44(7):1430–1436. [PubMed] [Google Scholar]
- James P., Ellis C. J., Whitlock R. M., McNeil A. R., Henley J., Anderson N. E. Relation between troponin T concentration and mortality in patients presenting with an acute stroke: observational study. BMJ. 2000 Jun 3;320(7248):1502–1504. doi: 10.1136/bmj.320.7248.1502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miall-Allen V. M., de Vries L. S., Whitelaw A. G. Mean arterial blood pressure and neonatal cerebral lesions. Arch Dis Child. 1987 Oct;62(10):1068–1069. doi: 10.1136/adc.62.10.1068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Möller J. C., Thielsen B., Schaible T. F., Reiss I., Kohl M., Welp T., Gortner L. Value of myocardial hypoxia markers (creatine kinase and its MB-fraction, troponin-T, QT-intervals) and serum creatinine for the retrospective diagnosis of perinatal asphyxia. Biol Neonate. 1998;73(6):367–374. doi: 10.1159/000013999. [DOI] [PubMed] [Google Scholar]
- Narin N., Cetin N., Kiliç H., Başbuğ M., Narin F., Kafali M., Uzüm K., Genç E., Ustünbaş H. B. Diagnostic value of troponin T in neonates of mild pre-eclamptic mothers. Biol Neonate. 1999;75(2):137–142. doi: 10.1159/000014089. [DOI] [PubMed] [Google Scholar]
- Primhak R. A., Jedeikin R., Ellis G., Makela S. K., Gillan J. E., Swyer P. R., Rowe R. D. Myocardial ischaemia in asphyxia neonatorum. Electrocardiographic, enzymatic and histological correlations. Acta Paediatr Scand. 1985 Jul;74(4):595–600. doi: 10.1111/j.1651-2227.1985.tb11036.x. [DOI] [PubMed] [Google Scholar]
- Sasse S., Brand N. J., Kyprianou P., Dhoot G. K., Wade R., Arai M., Periasamy M., Yacoub M. H., Barton P. J. Troponin I gene expression during human cardiac development and in end-stage heart failure. Circ Res. 1993 May;72(5):932–938. doi: 10.1161/01.res.72.5.932. [DOI] [PubMed] [Google Scholar]
- Shelton S. D., Fouse B. L., Holleman C. M., Sedor F. A., Herbert W. N. Cardiac troponin T levels in umbilical cord blood. Am J Obstet Gynecol. 1999 Nov;181(5 Pt 1):1259–1262. doi: 10.1016/s0002-9378(99)70119-5. [DOI] [PubMed] [Google Scholar]
- Thiru Y., Pathan N., Bignall S., Habibi P., Levin M. A myocardial cytotoxic process is involved in the cardiac dysfunction of meningococcal septic shock. Crit Care Med. 2000 Aug;28(8):2979–2983. doi: 10.1097/00003246-200008000-00049. [DOI] [PubMed] [Google Scholar]
- Trevisanuto D., Lachin M., Zaninotto M., Pellegrino P. A., Plebani M., Cantarutti F., Zanardo V. Cardiac troponin T in newborn infants with transient myocardial ischemia. Biol Neonate. 1998;73(3):161–165. doi: 10.1159/000013973. [DOI] [PubMed] [Google Scholar]
- Trevisanuto D., Zaninotto M., Altinier S., Plebani M., Zanardo V. High serum cardiac troponin T concentrations in preterm infants with respiratory distress syndrome. Acta Paediatr. 2000 Sep;89(9):1134–1136. doi: 10.1080/713794580. [DOI] [PubMed] [Google Scholar]
- Van Bel F., Walther F. J. Myocardial dysfunction and cerebral blood flow velocity following birth asphyxia. Acta Paediatr Scand. 1990 Aug-Sep;79(8-9):756–762. doi: 10.1111/j.1651-2227.1990.tb11551.x. [DOI] [PubMed] [Google Scholar]
- Walther F. J., Siassi B., Ramadan N. A., Wu P. Y. Cardiac output in newborn infants with transient myocardial dysfunction. J Pediatr. 1985 Nov;107(5):781–785. doi: 10.1016/s0022-3476(85)80417-0. [DOI] [PubMed] [Google Scholar]