Abstract
Background: Calprotectin, a major component of soluble cytosolic proteins in human neutrophil granulocytes, is excreted in excess in stools during inflammatory bowel disease in adults and children. Faecal calprotectin concentrations are also higher during the first year of life than in adults.
Objectives: To measure faecal calprotectin concentrations in the neonatal period and define reference values according to the mode of feeding: standard infant formula, prebiotic infant formula (Calisma, Blédina SA, France), or breast feeding.
Patients and methods: A prospective study was carried out over three months in 69 full term, healthy newborns with a median gestational age of 39.8 weeks (range 37–41.5) and a birth weight of 3300 g (range 2600–4460). Three groups were formed depending on the mode of feeding: group 1 (n = 18) received a standard infant formula, group 2 (n = 19) the prebiotic infant formula, and group 3 (n = 32) was breast fed. One stool sample was taken from each newborn on day 4 (3–7), and faecal calprotectin analysed using a commercial enzyme linked immunoassay (Calprest, Eurospital, Italy).
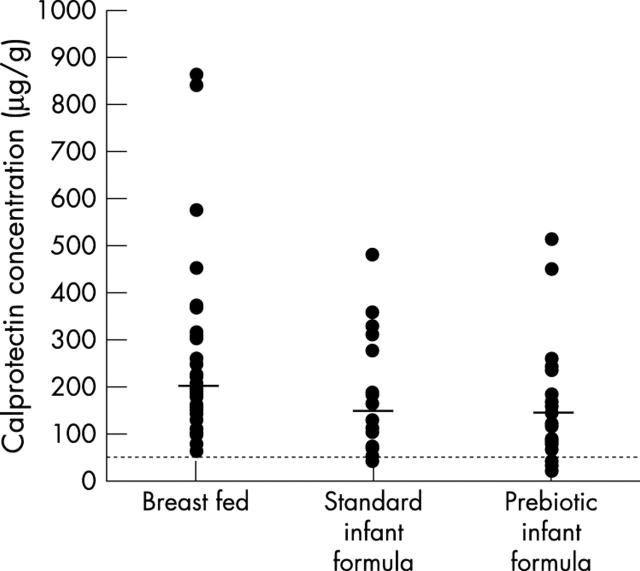
Results: Faecal calprotectin concentrations (median 167 µg/g) were higher than reference values in healthy adults. The concentration was below the upper reference limit for adults (50 µg/g) for three infants only, one fed the standard formula and two fed the prebiotic formula. Concentrations did not differ significantly according to method of feeding.
Conclusions: Compared with healthy adults, newborns have high calprotectin concentrations in the first days of life. There is no obvious influence of the mode of feeding.
Full Text
The Full Text of this article is available as a PDF (67.0 KB).
Figure 1.
Faecal calprotectin concentrations in newborns fed by three different methods. Solid lines indicate median concentrations, and the dotted line indicates the upper reference limit of calprotectin concentration in adults (50 µg/g).
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Berstad A., Arslan G., Folvik G. Relationship between intestinal permeability and calprotectin concentration in gut lavage fluid. Scand J Gastroenterol. 2000 Jan;35(1):64–69. doi: 10.1080/003655200750024551. [DOI] [PubMed] [Google Scholar]
- Bjarnason I., MacPherson A., Hollander D. Intestinal permeability: an overview. Gastroenterology. 1995 May;108(5):1566–1581. doi: 10.1016/0016-5085(95)90708-4. [DOI] [PubMed] [Google Scholar]
- Bjarnason I., Sherwood R. Fecal calprotectin: a significant step in the noninvasive assessment of intestinal inflammation. J Pediatr Gastroenterol Nutr. 2001 Jul;33(1):11–13. doi: 10.1097/00005176-200107000-00002. [DOI] [PubMed] [Google Scholar]
- Bunn S. K., Bisset W. M., Main M. J., Golden B. E. Fecal calprotectin as a measure of disease activity in childhood inflammatory bowel disease. J Pediatr Gastroenterol Nutr. 2001 Feb;32(2):171–177. doi: 10.1097/00005176-200102000-00015. [DOI] [PubMed] [Google Scholar]
- Bunn S. K., Bisset W. M., Main M. J., Gray E. S., Olson S., Golden B. E. Fecal calprotectin: validation as a noninvasive measure of bowel inflammation in childhood inflammatory bowel disease. J Pediatr Gastroenterol Nutr. 2001 Jul;33(1):14–22. doi: 10.1097/00005176-200107000-00003. [DOI] [PubMed] [Google Scholar]
- Carroll Daniel, Corfield Anthony, Spicer Richard, Cairns Pamela. Faecal calprotectin concentrations and diagnosis of necrotising enterocolitis. Lancet. 2003 Jan 25;361(9354):310–311. doi: 10.1016/S0140-6736(03)12333-1. [DOI] [PubMed] [Google Scholar]
- Collins M. D., Gibson G. R. Probiotics, prebiotics, and synbiotics: approaches for modulating the microbial ecology of the gut. Am J Clin Nutr. 1999 May;69(5):1052S–1057S. doi: 10.1093/ajcn/69.5.1052s. [DOI] [PubMed] [Google Scholar]
- Olafsdottir E., Aksnes L., Fluge G., Berstad A. Faecal calprotectin levels in infants with infantile colic, healthy infants, children with inflammatory bowel disease, children with recurrent abdominal pain and healthy children. Acta Paediatr. 2002;91(1):45–50. doi: 10.1080/080352502753457932. [DOI] [PubMed] [Google Scholar]
- Romond M. B., Ais A., Guillemot F., Bounouader R., Cortot A., Romond C. Cell-free whey from milk fermented with Bifidobacterium breve C50 used to modify the colonic microflora of healthy subjects. J Dairy Sci. 1998 May;81(5):1229–1235. doi: 10.3168/jds.S0022-0302(98)75683-8. [DOI] [PubMed] [Google Scholar]
- Rugtveit Jarle, Fagerhol Magne K. Age-dependent variations in fecal calprotectin concentrations in children. J Pediatr Gastroenterol Nutr. 2002 Mar;34(3):323–325. doi: 10.1097/00005176-200203000-00022. [DOI] [PubMed] [Google Scholar]
- Røseth A. G., Fagerhol M. K., Aadland E., Schjønsby H. Assessment of the neutrophil dominating protein calprotectin in feces. A methodologic study. Scand J Gastroenterol. 1992 Sep;27(9):793–798. doi: 10.3109/00365529209011186. [DOI] [PubMed] [Google Scholar]
- Steinbakk M., Naess-Andresen C. F., Lingaas E., Dale I., Brandtzaeg P., Fagerhol M. K. Antimicrobial actions of calcium binding leucocyte L1 protein, calprotectin. Lancet. 1990 Sep 29;336(8718):763–765. doi: 10.1016/0140-6736(90)93237-j. [DOI] [PubMed] [Google Scholar]
- Summerton Christopher B., Longlands Michael G., Wiener Keith, Shreeve David R. Faecal calprotectin: a marker of inflammation throughout the intestinal tract. Eur J Gastroenterol Hepatol. 2002 Aug;14(8):841–845. doi: 10.1097/00042737-200208000-00005. [DOI] [PubMed] [Google Scholar]
- Tibble J., Teahon K., Thjodleifsson B., Roseth A., Sigthorsson G., Bridger S., Foster R., Sherwood R., Fagerhol M., Bjarnason I. A simple method for assessing intestinal inflammation in Crohn's disease. Gut. 2000 Oct;47(4):506–513. doi: 10.1136/gut.47.4.506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tøn H., Brandsnes, Dale S., Holtlund J., Skuibina E., Schjønsby H., Johne B. Improved assay for fecal calprotectin. Clin Chim Acta. 2000 Feb 25;292(1-2):41–54. doi: 10.1016/s0009-8981(99)00206-5. [DOI] [PubMed] [Google Scholar]
- Weaver L. T., Laker M. F., Nelson R. Intestinal permeability in the newborn. Arch Dis Child. 1984 Mar;59(3):236–241. doi: 10.1136/adc.59.3.236. [DOI] [PMC free article] [PubMed] [Google Scholar]