Abstract
Objective: To investigate the relation between the measured intravascular blood volume (BV) and current methods of indirectly assessing BV status in sick preterm infants on the first day of life.
Methods: Thirty eight preterm infants of gestation 24–32 weeks (median 30) and weight 480–2060 g (median 1220) were studied. Red cell volume was measured by the fetal haemoglobin dilution method in six infants and by the biotin labelled autologous red cell dilution method in the remaining 32. Total BV was calculated by dividing red cell volume by packed cell volume. Indirect assessments of BV status using heart rate (HR), core-peripheral temperature difference, mean arterial pressure, base excess, and packed cell volume were recorded.
Results: The mean (SD) initial measured BV was 71 (12) ml/kg (range 53–105). The mean HR was 148 beats/min (range 130–180), which correlated positively (r = 0.39, p = 0.02) with BV (higher HR was associated with higher BV). The mean base excess was –3.19 mmol/l (range –18 to +6.2). The negative base excess correlated significantly positively (r = 0.41, p < 0.01) with BV (more acidotic babies tended to have higher BV). There was no significant correlation between core-peripheral temperature difference, mean arterial pressure, or packed cell volume and BV. Regression analysis showed that base excess and HR were significantly related to BV; base excess alone can predict variability in BV only to17%, and base excess with HR can predict variability in BV to 29%.
Conclusion: The conventional clinical and laboratory indices are poor predictors of measured blood volume.
Full Text
The Full Text of this article is available as a PDF (80.9 KB).
Figure 1.
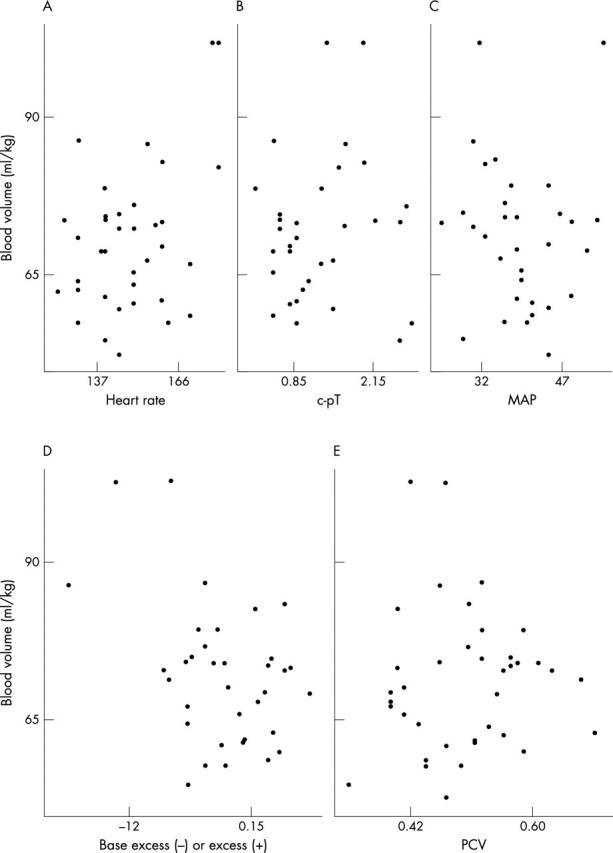
Plots of blood volume against each of the potential explanatory variables. c-pT, Core-peripheral temperature difference; MAP, mean arterial pressure; PCV, packed cell volume.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Anthony M. Y., Goodall S. R., Papouli M., Levene M. I. Measurement of plasma volume in neonates. Arch Dis Child. 1992 Jan;67(1 Spec No):36–40. doi: 10.1136/adc.67.1_spec_no.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bailey J. M., Levy J. H., Kopel M. A., Tobia V., Grabenkort W. R. Relationship between clinical evaluation of peripheral perfusion and global hemodynamics in adults after cardiac surgery. Crit Care Med. 1990 Dec;18(12):1353–1356. doi: 10.1097/00003246-199012000-00008. [DOI] [PubMed] [Google Scholar]
- Bauer R., Hoyer D., Walter B., Gaser E., Kluge H., Zwiener U. Changed systemic and cerebral hemodynamics and oxygen supply due to gradual hemorrhagic hypotension induced by an external PID-controller in newborn swine. Exp Toxicol Pathol. 1997 Dec;49(6):469–476. doi: 10.1016/S0940-2993(97)80139-X. [DOI] [PubMed] [Google Scholar]
- Cavill I., Trevett D., Fisher J., Hoy T. The measurement of the total volume of red cells in man: a non-radioactive approach using biotin. Br J Haematol. 1988 Dec;70(4):491–493. doi: 10.1111/j.1365-2141.1988.tb02522.x. [DOI] [PubMed] [Google Scholar]
- Faxelius G., Raye J., Gutberlet R., Swanstrom S., Tsiantos A., Dolanski E., Dehan M., Dyer N., Lindstrom D., Brill A. B. Red cell volume measurements and acute blood loss in high-risk newborn infants. J Pediatr. 1977 Feb;90(2):273–281. doi: 10.1016/s0022-3476(77)80650-1. [DOI] [PubMed] [Google Scholar]
- Hope P. Pump up the volume? The routine early use of colloid in very preterm infants. Arch Dis Child Fetal Neonatal Ed. 1998 May;78(3):F163–F165. doi: 10.1136/fn.78.3.f163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hudson I. R., Cavill I. A., Cooke A., Holland B. M., Hoy T. G., Trevett D., Turner T. L., Wardrop C. A. Biotin labeling of red cells in the measurement of red cell volume in preterm infants. Pediatr Res. 1990 Sep;28(3):199–202. doi: 10.1203/00006450-199009000-00006. [DOI] [PubMed] [Google Scholar]
- JAYKKA S. Capillary erection and the structural appearance of fetal and neonatl lungs. Acta Paediatr. 1958 Sep;47(5):484–500. doi: 10.1111/j.1651-2227.1958.tb07664.x. [DOI] [PubMed] [Google Scholar]
- Jones J. G., Holland B. M., Hudson I. R., Wardrop C. A. Total circulating red cells versus haematocrit as the primary descriptor of oxygen transport by the blood. Br J Haematol. 1990 Oct;76(2):288–294. doi: 10.1111/j.1365-2141.1990.tb07886.x. [DOI] [PubMed] [Google Scholar]
- Lambert H. J., Baylis P. H., Coulthard M. G. Central-peripheral temperature difference, blood pressure, and arginine vasopressin in preterm neonates undergoing volume expansion. Arch Dis Child Fetal Neonatal Ed. 1998 Jan;78(1):F43–F45. doi: 10.1136/fn.78.1.f43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linderkamp O., Strohhacker I., Versmold H. T., Klose H., Riegel K. P., Betke K. Peripheral circulation in the newborn: interaction of peripheral blood flow, blood pressure, blood volume, and blood viscosity. Eur J Pediatr. 1978 Sep 8;129(2):73–81. doi: 10.1007/BF00442366. [DOI] [PubMed] [Google Scholar]
- Linderkamp O., Versmold H. T., Fendel H., Riegel K. P., Betke K. Association of neonatal respiratory distress with birth asphyxia and deficiency of red cell mass in premature infants. Eur J Pediatr. 1978 Oct 12;129(3):167–173. doi: 10.1007/BF00442160. [DOI] [PubMed] [Google Scholar]
- MOLLISON P. L., VEALL N., CUTBUSH M. Red cell and plasma volume in newborn infants. Arch Dis Child. 1950 Sep;25(123):242–253. doi: 10.1136/adc.25.123.242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mock D. M., Bell E. F., Lankford G. L., Widness J. A. Hematocrit correlates well with circulating red blood cell volume in very low birth weight infants. Pediatr Res. 2001 Oct;50(4):525–531. doi: 10.1203/00006450-200110000-00017. [DOI] [PubMed] [Google Scholar]
- Mock D. M., Lankford G. L., Burmeister L. F., Strauss R. G. Circulating red cell volume and red cell survival can be accurately determined in sheep using the [14C]cyanate label. Pediatr Res. 1997 Jun;41(6):916–921. doi: 10.1203/00006450-199706000-00020. [DOI] [PubMed] [Google Scholar]
- Mock D. M., Lankford G. L., Widness J. A., Burmeister L. F., Kahn D., Strauss R. G. Measurement of circulating red cell volume using biotin-labeled red cells: validation against 51Cr-labeled red cells. Transfusion. 1999 Feb;39(2):149–155. doi: 10.1046/j.1537-2995.1999.39299154728.x. [DOI] [PubMed] [Google Scholar]
- Nelle M., Zilow E. P., Kraus M., Bastert G., Linderkamp O. The effect of Leboyer delivery on blood viscosity and other hemorheologic parameters in term neonates. Am J Obstet Gynecol. 1993 Jul;169(1):189–193. doi: 10.1016/0002-9378(93)90161-b. [DOI] [PubMed] [Google Scholar]
- Phillips H. M., Holland B. M., Abdel-Moiz A., Fayed S., Jones J. G., Turner T. L., Wardrop C. A., Cockburn F. Determination of red-cell mass in assessment and management of anaemia in babies needing blood transfusion. Lancet. 1986 Apr 19;1(8486):882–884. doi: 10.1016/s0140-6736(86)90988-8. [DOI] [PubMed] [Google Scholar]
- Ryan C. A., Soder C. M. Relationship between core/peripheral temperature gradient and central hemodynamics in children after open heart surgery. Crit Care Med. 1989 Jul;17(7):638–640. doi: 10.1097/00003246-198907000-00008. [DOI] [PubMed] [Google Scholar]
- Shippy C. R., Appel P. L., Shoemaker W. C. Reliability of clinical monitoring to assess blood volume in critically ill patients. Crit Care Med. 1984 Feb;12(2):107–112. doi: 10.1097/00003246-198402000-00005. [DOI] [PubMed] [Google Scholar]
- THEYE R. A., TUOHY G. F. HEMODYNAMICS AND BLOOD VOLUME DURING OPERATION WITH ETHER ANESTHESIA AND UNREPLACED BLOOD LOSS. Anesthesiology. 1964 Jan-Feb;25:6–14. doi: 10.1097/00000542-196401000-00003. [DOI] [PubMed] [Google Scholar]
- Tibby S. M., Hatherill M., Murdoch I. A. Capillary refill and core-peripheral temperature gap as indicators of haemodynamic status in paediatric intensive care patients. Arch Dis Child. 1999 Feb;80(2):163–166. doi: 10.1136/adc.80.2.163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woods I., Wilkins R. G., Edwards J. D., Martin P. D., Faragher E. B. Danger of using core/peripheral temperature gradient as a guide to therapy in shock. Crit Care Med. 1987 Sep;15(9):850–852. doi: 10.1097/00003246-198709000-00010. [DOI] [PubMed] [Google Scholar]


