Abstract
Background: A proportion of neonatal deaths from asphyxia have been shown to be associated with pre-existing brain injury.
Objectives: (a) To compare the epidemiology of infants displaying signs of birth asphyxia with those not showing signs; (b) to examine the neuropathology and determine if possible the timing of brain insult comparing asphyxiated with non-asphyxiated infants; (c) to compare the clinical features of those born with birth asphyxia with and without pre-labour damage.
Methods: Over a two year period, all 22 Scottish delivery units collected clinical details on early neonatal deaths. Requests for post mortem included separate requests for detailed neuropathological examination of the brain. Infants were classified into two groups: birth asphyxia and non-birth asphyxia. Clinicopathological correlation was used to attempt to define the time of brain insult.
Results: Detailed clinical data were available on 137 of 174 early neonatal deaths that met the inclusion criteria. Seventy of 88 parents who had agreed to post mortem examination consented to a detailed examination of additional samples from the brain; in 53 of these cases the infant was born in an asphyxiated condition. All asphyxiated and encephalopathic infants, 38% of mature and 52% of preterm infants with features of birth asphyxia but without encephalopathy, and only one of 12 infants without any signs of birth asphyxia showed damage consistent with onset before the start of labour.
Conclusions: In a large proportion of neonatal deaths, brain injury predates the onset of labour. This is more common in infants born in an asphyxiated condition.
Full Text
The Full Text of this article is available as a PDF (254.8 KB).
Figure 1.
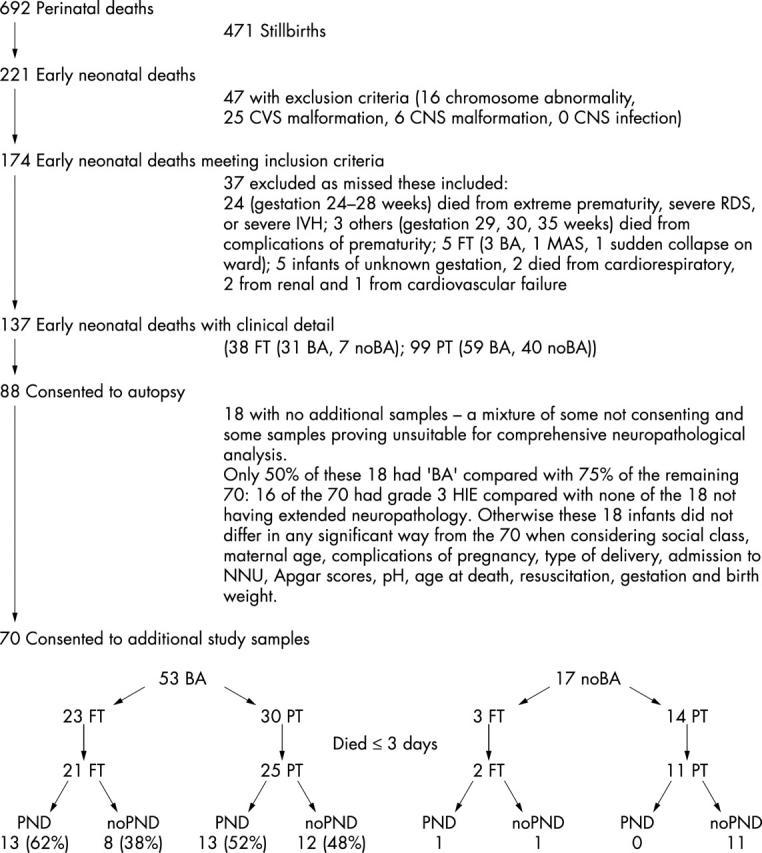
The Scottish perinatal deaths cohort. FT, full term; RDS, respiratory distress syndrome; PT, preterm < 37 weeks; IVH, intraventricular haemorrhage; BA, birth asphyxia; MAS, meconium aspiration syndrome; noBA, no birth asphyxia; HIE, hypoxic-ischaemic encephalopathy; PND, prenatal brain damage; NNU, neonatal unit; noPND, no prenatal brain damage; CVS, cardiovascular system; CNS, central nervous system.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Adamson S. J., Alessandri L. M., Badawi N., Burton P. R., Pemberton P. J., Stanley F. Predictors of neonatal encephalopathy in full-term infants. BMJ. 1995 Sep 2;311(7005):598–602. doi: 10.1136/bmj.311.7005.598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Altshuler G. Some placental considerations related to neurodevelopmental and other disorders. J Child Neurol. 1993 Jan;8(1):78–94. doi: 10.1177/088307389300800111. [DOI] [PubMed] [Google Scholar]
- Amato M., Gambon R. C., Von Muralt G. Accuracy of Apgar score and arterial cord-blood pH in diagnosis of perinatal brain-damage assessed by CK-BB isoenzyme measurement. J Perinat Med. 1986;14(5):335–338. doi: 10.1515/jpme.1986.14.5.335. [DOI] [PubMed] [Google Scholar]
- Badawi N., Kurinczuk J. J., Keogh J. M., Alessandri L. M., O'Sullivan F., Burton P. R., Pemberton P. J., Stanley F. J. Antepartum risk factors for newborn encephalopathy: the Western Australian case-control study. BMJ. 1998 Dec 5;317(7172):1549–1553. doi: 10.1136/bmj.317.7172.1549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Badawi N., Kurinczuk J. J., Keogh J. M., Alessandri L. M., O'Sullivan F., Burton P. R., Pemberton P. J., Stanley F. J. Intrapartum risk factors for newborn encephalopathy: the Western Australian case-control study. BMJ. 1998 Dec 5;317(7172):1554–1558. doi: 10.1136/bmj.317.7172.1554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bakketeig L. S. Only a minor part of cerebral palsy cases begin in labour. But still room for controversial childbirth issues in court. BMJ. 1999 Oct 16;319(7216):1016–1017. doi: 10.1136/bmj.319.7216.1016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banker B. Q. The neuropathological effects of anoxia and hypoglycemia in the newborn. Dev Med Child Neurol. 1967 Oct;9(5):544–550. doi: 10.1111/j.1469-8749.1967.tb02323.x. [DOI] [PubMed] [Google Scholar]
- Berkus M. D., Langer O., Samueloff A., Xenakis E. M., Field N. T., Ridgway L. E. Meconium-stained amniotic fluid: increased risk for adverse neonatal outcome. Obstet Gynecol. 1994 Jul;84(1):115–120. [PubMed] [Google Scholar]
- Blair E., Stanley F. J. Intrapartum asphyxia: a rare cause of cerebral palsy. J Pediatr. 1988 Apr;112(4):515–519. doi: 10.1016/s0022-3476(88)80161-6. [DOI] [PubMed] [Google Scholar]
- Blair E., Stanley F. When can cerebral palsy be prevented? The generation of causal hypotheses by multivariate analysis of a case-control study. Paediatr Perinat Epidemiol. 1993 Jul;7(3):272–301. doi: 10.1111/j.1365-3016.1993.tb00405.x. [DOI] [PubMed] [Google Scholar]
- Brandt-Niebelschütz S., Saling E. Indications for operative termination of labor on cardiotocography and fetal blood analysis: the reliability of these methods. J Perinat Med. 1994;22(1):19–27. doi: 10.1515/jpme.1994.22.1.19. [DOI] [PubMed] [Google Scholar]
- Cowan Frances, Rutherford Mary, Groenendaal Floris, Eken Paula, Mercuri Eugenio, Bydder Graeme M., Meiners Linda C., Dubowitz Lilly M. S., de Vries Linda S. Origin and timing of brain lesions in term infants with neonatal encephalopathy. Lancet. 2003 Mar 1;361(9359):736–742. doi: 10.1016/S0140-6736(03)12658-X. [DOI] [PubMed] [Google Scholar]
- Del Bigio M. R., Becker L. E. Microglial aggregation in the dentate gyrus: a marker of mild hypoxic-ischaemic brain insult in human infants. Neuropathol Appl Neurobiol. 1994 Apr;20(2):144–151. doi: 10.1111/j.1365-2990.1994.tb01173.x. [DOI] [PubMed] [Google Scholar]
- Edwards A. D., Nelson K. B. Neonatal encephalopathies. Time to reconsider the cause of encephalopathies. BMJ. 1998 Dec 5;317(7172):1537–1538. doi: 10.1136/bmj.317.7172.1537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellis W. G., Goetzman B. W., Lindenberg J. A. Neuropathologic documentation of prenatal brain damage. Am J Dis Child. 1988 Aug;142(8):858–866. doi: 10.1001/archpedi.1988.02150080064025. [DOI] [PubMed] [Google Scholar]
- Ellis W. G., Goetzman B. W., Lindenberg J. A. Neuropathologic documentation of prenatal brain damage. Am J Dis Child. 1988 Aug;142(8):858–866. doi: 10.1001/archpedi.1988.02150080064025. [DOI] [PubMed] [Google Scholar]
- Fields L. M., Entman S. S., Boehm F. H. Correlation of the one-minute Apgar score and the pH value of umbilical arterial blood. South Med J. 1983 Dec;76(12):1477–1479. doi: 10.1097/00007611-198312000-00005. [DOI] [PubMed] [Google Scholar]
- Friede R. L. Ponto-subicular lesions in perinatal anoxia. Arch Pathol. 1972 Oct;94(4):343–354. [PubMed] [Google Scholar]
- Gaffney G., Sellers S., Flavell V., Squier M., Johnson A. Case-control study of intrapartum care, cerebral palsy, and perinatal death. BMJ. 1994 Mar 19;308(6931):743–750. doi: 10.1136/bmj.308.6931.743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilles F. H., Leviton A., Golden J. A., Paneth N., Rudelli R. D. Groups of histopathologic abnormalities in brains of very low birthweight infants. J Neuropathol Exp Neurol. 1998 Nov;57(11):1026–1034. doi: 10.1097/00005072-199811000-00005. [DOI] [PubMed] [Google Scholar]
- Gilles F. H., Murphy S. F. Perinatal telencephalic leucoencephalopathy. J Neurol Neurosurg Psychiatry. 1969 Oct;32(5):404–413. doi: 10.1136/jnnp.32.5.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilstrap L. C., 3rd, Leveno K. J., Burris J., Williams M. L., Little B. B. Diagnosis of birth asphyxia on the basis of fetal pH, Apgar score, and newborn cerebral dysfunction. Am J Obstet Gynecol. 1989 Sep;161(3):825–830. doi: 10.1016/0002-9378(89)90410-9. [DOI] [PubMed] [Google Scholar]
- Golden J. A., Gilles F. H., Rudelli R., Leviton A. Frequency of neuropathological abnormalities in very low birth weight infants. J Neuropathol Exp Neurol. 1997 May;56(5):472–478. doi: 10.1097/00005072-199705000-00002. [DOI] [PubMed] [Google Scholar]
- Gunn A. J., Gunn T. R. Changes in risk factors for hypoxic-ischaemic seizures in term infants. Aust N Z J Obstet Gynaecol. 1997 Feb;37(1):36–39. doi: 10.1111/j.1479-828x.1997.tb02214.x. [DOI] [PubMed] [Google Scholar]
- Hall D. M. Birth asphyxia and cerebral palsy. BMJ. 1989 Jul 29;299(6694):279–282. doi: 10.1136/bmj.299.6694.279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson J. W., Richards D. S., Wagaman R. A. The case for routine umbilical blood acid-base studies at delivery. Am J Obstet Gynecol. 1990 Mar;162(3):621–625. doi: 10.1016/0002-9378(90)90970-i. [DOI] [PubMed] [Google Scholar]
- Josten B. E., Johnson T. R., Nelson J. P. Umbilical cord blood pH and Apgar scores as an index of neonatal health. Am J Obstet Gynecol. 1987 Oct;157(4 Pt 1):843–848. doi: 10.1016/s0002-9378(87)80069-8. [DOI] [PubMed] [Google Scholar]
- Kalter H. Five-decade international trends in the relation of perinatal mortality and congenital malformations: stillbirth and neonatal death compared. Int J Epidemiol. 1991 Mar;20(1):173–179. doi: 10.1093/ije/20.1.173. [DOI] [PubMed] [Google Scholar]
- Leviton A., Paneth N. White matter damage in preterm newborns--an epidemiologic perspective. Early Hum Dev. 1990 Oct;24(1):1–22. doi: 10.1016/0378-3782(90)90002-z. [DOI] [PubMed] [Google Scholar]
- Low J. A., Robertson D. M., Simpson L. L. Temporal relationships of neuropathologic conditions caused by perinatal asphyxia. Am J Obstet Gynecol. 1989 Mar;160(3):608–614. doi: 10.1016/s0002-9378(89)80040-7. [DOI] [PubMed] [Google Scholar]
- MacDonald D., Grant A., Sheridan-Pereira M., Boylan P., Chalmers I. The Dublin randomized controlled trial of intrapartum fetal heart rate monitoring. Am J Obstet Gynecol. 1985 Jul 1;152(5):524–539. doi: 10.1016/0002-9378(85)90619-2. [DOI] [PubMed] [Google Scholar]
- MacLennan A. A template for defining a causal relation between acute intrapartum events and cerebral palsy: international consensus statement. BMJ. 1999 Oct 16;319(7216):1054–1059. doi: 10.1136/bmj.319.7216.1054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marín-Padilla M. Developmental neuropathology and impact of perinatal brain damage. I: Hemorrhagic lesions of neocortex. J Neuropathol Exp Neurol. 1996 Jul;55(7):758–773. doi: 10.1097/00005072-199607000-00002. [DOI] [PubMed] [Google Scholar]
- Marín-Padilla M. Developmental neuropathology and impact of perinatal brain damage. II: white matter lesions of the neocortex. J Neuropathol Exp Neurol. 1997 Mar;56(3):219–235. doi: 10.1097/00005072-199703000-00001. [DOI] [PubMed] [Google Scholar]
- Marín-Padilla M. Developmental neuropathology and impact of perinatal brain damage. III: gray matter lesions of the neocortex. J Neuropathol Exp Neurol. 1999 May;58(5):407–429. doi: 10.1097/00005072-199905000-00001. [DOI] [PubMed] [Google Scholar]
- McShane M., Maguire S., McClure G., Halliday H., McC Reid M. Birth asphyxia, encephalopathy and outcome. Ir Med J. 1987 Dec;80(12):421–422. [PubMed] [Google Scholar]
- Mito T., Kamei A., Takashima S., Becker L. E. Clinicopathological study of pontosubicular necrosis. Neuropediatrics. 1993 Aug;24(4):204–207. doi: 10.1055/s-2008-1071540. [DOI] [PubMed] [Google Scholar]
- Nelson K. B., Leviton A. How much of neonatal encephalopathy is due to birth asphyxia? Am J Dis Child. 1991 Nov;145(11):1325–1331. doi: 10.1001/archpedi.1991.02160110117034. [DOI] [PubMed] [Google Scholar]
- Nelson K. B., Leviton A. How much of neonatal encephalopathy is due to birth asphyxia? Am J Dis Child. 1991 Nov;145(11):1325–1331. doi: 10.1001/archpedi.1991.02160110117034. [DOI] [PubMed] [Google Scholar]
- Nelson K. B. Relationship of intrapartum and delivery room events to long-term neurologic outcome. Clin Perinatol. 1989 Dec;16(4):995–1007. [PubMed] [Google Scholar]
- Nelson K. B. What proportion of cerebral palsy is related to birth asphyxia? J Pediatr. 1988 Apr;112(4):572–574. doi: 10.1016/s0022-3476(88)80169-0. [DOI] [PubMed] [Google Scholar]
- Niijima S., Levene M. I. Post-asphyxial encephalopathy in a preterm infant. Dev Med Child Neurol. 1989 Jun;31(3):395–397. doi: 10.1111/j.1469-8749.1989.tb04010.x. [DOI] [PubMed] [Google Scholar]
- Norenberg M. D. Astrocyte responses to CNS injury. J Neuropathol Exp Neurol. 1994 May;53(3):213–220. doi: 10.1097/00005072-199405000-00001. [DOI] [PubMed] [Google Scholar]
- Norman M. G. Antenatal neuronal loss and gliosis of the reticular formation, thalamus, and hypothalamus. A report of three cases. Neurology. 1972 Sep;22(9):910–916. doi: 10.1212/wnl.22.9.910. [DOI] [PubMed] [Google Scholar]
- Norman M. G. Perinatal brain damage. Perspect Pediatr Pathol. 1978;4:41–92. [PubMed] [Google Scholar]
- Paneth N., Fox H. E. The relationship of Apgar score to neurologic handicap: a survey of clinicians. Obstet Gynecol. 1983 May;61(5):547–550. [PubMed] [Google Scholar]
- Paneth N., Rudelli R., Monte W., Rodriguez E., Pinto J., Kairam R., Kazam E. White matter necrosis in very low birth weight infants: neuropathologic and ultrasonographic findings in infants surviving six days or longer. J Pediatr. 1990 Jun;116(6):975–984. doi: 10.1016/s0022-3476(05)80664-x. [DOI] [PubMed] [Google Scholar]
- Roessmann U., Gambetti P. Pathological reaction of astrocytes in perinatal brain injury. Immunohistochemical study. Acta Neuropathol. 1986;70(3-4):302–307. doi: 10.1007/BF00686088. [DOI] [PubMed] [Google Scholar]
- Rorke L. B. Anatomical features of the developing brain implicated in pathogenesis of hypoxic-ischemic injury. Brain Pathol. 1992 Jul;2(3):211–221. doi: 10.1111/j.1750-3639.1992.tb00694.x. [DOI] [PubMed] [Google Scholar]
- Ruth V. J., Raivio K. O. Perinatal brain damage: predictive value of metabolic acidosis and the Apgar score. BMJ. 1988 Jul 2;297(6640):24–27. doi: 10.1136/bmj.297.6640.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarnat H. B., Sarnat M. S. Neonatal encephalopathy following fetal distress. A clinical and electroencephalographic study. Arch Neurol. 1976 Oct;33(10):696–705. doi: 10.1001/archneur.1976.00500100030012. [DOI] [PubMed] [Google Scholar]
- Skullerud K., Westre B. Frequency and prognostic significance of germinal matrix hemorrhage, periventricular leukomalacia, and pontosubicular necrosis in preterm neonates. Acta Neuropathol. 1986;70(3-4):257–261. doi: 10.1007/BF00686080. [DOI] [PubMed] [Google Scholar]
- Squier M., Keeling J. W. The incidence of prenatal brain injury. Neuropathol Appl Neurobiol. 1991 Feb;17(1):29–38. doi: 10.1111/j.1365-2990.1991.tb00691.x. [DOI] [PubMed] [Google Scholar]
- Steer P. J., Eigbe F., Lissauer T. J., Beard R. W. Interrelationships among abnormal cardiotocograms in labor, meconium staining of the amniotic fluid, arterial cord blood pH, and Apgar scores. Obstet Gynecol. 1989 Nov;74(5):715–721. [PubMed] [Google Scholar]
- Sykes G. S., Molloy P. M., Johnson P., Gu W., Ashworth F., Stirrat G. M., Turnbull A. C. Do Apgar scores indicate asphyxia? Lancet. 1982 Feb 27;1(8270):494–496. doi: 10.1016/s0140-6736(82)91462-3. [DOI] [PubMed] [Google Scholar]
- Yudkin P. L., Johnson A., Clover L. M., Murphy K. W. Assessing the contribution of birth asphyxia to cerebral palsy in term singletons. Paediatr Perinat Epidemiol. 1995 Apr;9(2):156–170. doi: 10.1111/j.1365-3016.1995.tb00131.x. [DOI] [PubMed] [Google Scholar]
- Yudkin P. L., Johnson A., Clover L. M., Murphy K. W. Clustering of perinatal markers of birth asphyxia and outcome at age five years. Br J Obstet Gynaecol. 1994 Sep;101(9):774–781. doi: 10.1111/j.1471-0528.1994.tb11945.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


