Abstract
Background: The role of nasal continuous positive airways pressure (nCPAP) in the management of respiratory distress syndrome in preterm infants is not completely defined.
Objective: To evaluate the benefits and risks of prophylactic nCPAP in infants of 28–31 weeks gestation.
Design: Multicentre randomised controlled clinical trial.
Setting: Seventeen Italian neonatal intensive care units.
Patients: A total of 230 newborns of 28–31 weeks gestation, not intubated in the delivery room and without major malformations, were randomly assigned to prophylactic or rescue nCPAP.
Interventions: Prophylactic nCPAP was started within 30 minutes of birth, irrespective of oxygen requirement and clinical status. Rescue nCPAP was started when FIO2 requirement was > 0.4, for more than 30 minutes, to maintain transcutaneous oxygen saturation between 93% and 96%. Exogenous surfactant was given when FIO2 requirement was > 0.4 in nCPAP in the presence of radiological signs of respiratory distress syndrome.
Main outcome measures: Primary end point: need for exogenous surfactant. Secondary end points: need for mechanical ventilation and incidence of air leaks.
Results: Surfactant was needed by 22.6% in the prophylaxis group and 21.7% in the rescue group. Mechanical ventilation was required by 12.2% in both the prophylaxis and rescue group. The incidence of air leaks was 2.6% in both groups. More than 80% of both groups had received prenatal steroids.
Conclusions: In newborns of 28–31 weeks gestation, there is no greater benefit in giving prophylactic nCPAP than in starting nCPAP when the oxygen requirement increases to a FIO2 > 0.4.
Full Text
The Full Text of this article is available as a PDF (95.4 KB).
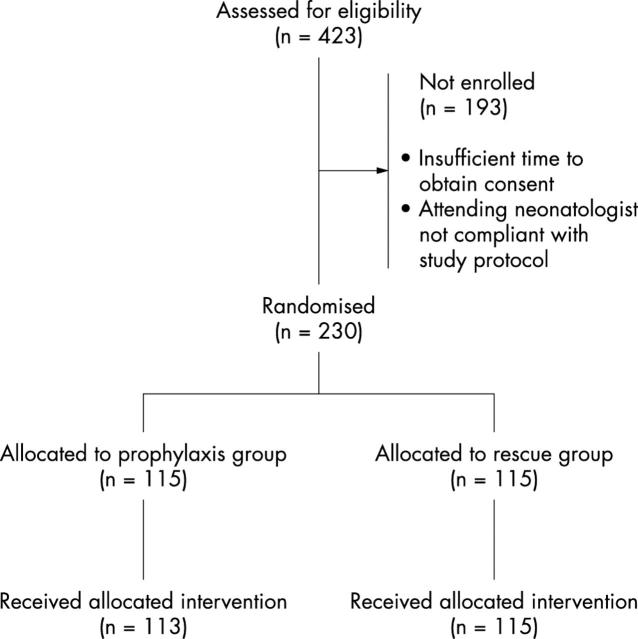
Figure 1.
Flow diagram of eligible newborns. The number of infants not randomised and the reasons for non-enrolment are provided. Two infants in the prophylaxis group did not receive the allocated treatment (both infants requiring surfactant were firstly mechanically ventilated and then given surfactant). Statistical analysis was by "intention to treat".
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Anand K. J., Barton B. A., McIntosh N., Lagercrantz H., Pelausa E., Young T. E., Vasa R. Analgesia and sedation in preterm neonates who require ventilatory support: results from the NOPAIN trial. Neonatal Outcome and Prolonged Analgesia in Neonates. Arch Pediatr Adolesc Med. 1999 Apr;153(4):331–338. doi: 10.1001/archpedi.153.4.331. [DOI] [PubMed] [Google Scholar]
- Blennow M., Jonsson B., Dahlström A., Sarman I., Bohlin K., Robertson B. Lungfunktionen kan förbättras hos för tidigt födda barn. Surfaktantbehandling och CPAP minskar behovet av respiratorvård. Lakartidningen. 1999 Mar 31;96(13):1571–1576. [PubMed] [Google Scholar]
- Bomsel F. Contribution à l'étude radiologique de la maladie des membranes hyalines: à propos de 110 cas. J Radiol Electrol Med Nucl. 1970 May;51(5):259–268. [PubMed] [Google Scholar]
- Caliumi-Pellegrini G., Agostino R., Orzalesi M., Nodari S., Marzetti G., Savignoni P. G., Bucci G. Twin nasal cannula for administration of continuous positive airway pressure to newborn infants. Arch Dis Child. 1974 Mar;49(3):228–230. doi: 10.1136/adc.49.3.228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Courtney S. E., Pyon K. H., Saslow J. G., Arnold G. K., Pandit P. B., Habib R. H. Lung recruitment and breathing pattern during variable versus continuous flow nasal continuous positive airway pressure in premature infants: an evaluation of three devices. Pediatrics. 2001 Feb;107(2):304–308. doi: 10.1542/peds.107.2.304. [DOI] [PubMed] [Google Scholar]
- Gittermann M. K., Fusch C., Gittermann A. R., Regazzoni B. M., Moessinger A. C. Early nasal continuous positive airway pressure treatment reduces the need for intubation in very low birth weight infants. Eur J Pediatr. 1997 May;156(5):384–388. doi: 10.1007/s004310050620. [DOI] [PubMed] [Google Scholar]
- Gregory G. A., Kitterman J. A., Phibbs R. H., Tooley W. H., Hamilton W. K. Treatment of the idiopathic respiratory-distress syndrome with continuous positive airway pressure. N Engl J Med. 1971 Jun 17;284(24):1333–1340. doi: 10.1056/NEJM197106172842401. [DOI] [PubMed] [Google Scholar]
- Han V. K., Beverley D. W., Clarson C., Sumabat W. O., Shaheed W. A., Brabyn D. G., Chance G. W. Randomized controlled trial of very early continuous distending pressure in the management of preterm infants. Early Hum Dev. 1987 Jan;15(1):21–32. doi: 10.1016/0378-3782(87)90097-1. [DOI] [PubMed] [Google Scholar]
- Jacobsen T., Grønvall J., Petersen S., Andersen G. E. "Minitouch" treatment of very low-birth-weight infants. Acta Paediatr. 1993 Nov;82(11):934–938. doi: 10.1111/j.1651-2227.1993.tb12603.x. [DOI] [PubMed] [Google Scholar]
- Jónsson B., Katz-Salamon M., Faxelius G., Broberger U., Lagercrantz H. Neonatal care of very-low-birthweight infants in special-care units and neonatal intensive-care units in Stockholm. Early nasal continuous positive airway pressure versus mechanical ventilation: gains and losses. Acta Paediatr Suppl. 1997 Apr;419:4–10. doi: 10.1111/j.1651-2227.1997.tb18303.x. [DOI] [PubMed] [Google Scholar]
- Kamper J., Ringsted C. Early treatment of idiopathic respiratory distress syndrome using binasal continuous positive airway pressure. Acta Paediatr Scand. 1990 Jun-Jul;79(6-7):581–586. doi: 10.1111/j.1651-2227.1990.tb11520.x. [DOI] [PubMed] [Google Scholar]
- Kattwinkel J., Fleming D., Cha C. C., Fanaroff A. A., Klaus M. H. A device for administration of continuous positive airway pressure by the nasal route. Pediatrics. 1973 Jul;52(1):131–134. [PubMed] [Google Scholar]
- Kavvadia V., Greenough A., Dimitriou G. Effect on lung function of continuous positive airway pressure administered either by infant flow driver or a single nasal prong. Eur J Pediatr. 2000 Apr;159(4):289–292. doi: 10.1007/s004310050072. [DOI] [PubMed] [Google Scholar]
- Klausner J. F., Lee A. Y., Hutchison A. A. Decreased imposed work with a new nasal continuous positive airway pressure device. Pediatr Pulmonol. 1996 Sep;22(3):188–194. doi: 10.1002/(SICI)1099-0496(199609)22:3<188::AID-PPUL8>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- Morley C. Continuous distending pressure. Arch Dis Child Fetal Neonatal Ed. 1999 Sep;81(2):F152–F156. doi: 10.1136/fn.81.2.f152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paky F., Koeck C. M. Pulse oximetry in ventilated preterm newborns: reliability of detection of hyperoxaemia and hypoxaemia, and feasibility of alarm settings. Acta Paediatr. 1995 Jun;84(6):613–616. doi: 10.1111/j.1651-2227.1995.tb13709.x. [DOI] [PubMed] [Google Scholar]
- Pandit P. B., Courtney S. E., Pyon K. H., Saslow J. G., Habib R. H. Work of breathing during constant- and variable-flow nasal continuous positive airway pressure in preterm neonates. Pediatrics. 2001 Sep;108(3):682–685. doi: 10.1542/peds.108.3.682. [DOI] [PubMed] [Google Scholar]
- Pedersen J. E., Nielsen K. Oropharyngeal and esophageal pressure during mono- and binasal CPAP in neonates. Acta Paediatr. 1994 Feb;83(2):143–149. doi: 10.1111/j.1651-2227.1994.tb13038.x. [DOI] [PubMed] [Google Scholar]
- Poets C. F., Southall D. P. Noninvasive monitoring of oxygenation in infants and children: practical considerations and areas of concern. Pediatrics. 1994 May;93(5):737–746. [PubMed] [Google Scholar]
- Stevenson D. K., Verter J., Fanaroff A. A., Oh W., Ehrenkranz R. A., Shankaran S., Donovan E. F., Wright L. L., Lemons J. A., Tyson J. E. Sex differences in outcomes of very low birthweight infants: the newborn male disadvantage. Arch Dis Child Fetal Neonatal Ed. 2000 Nov;83(3):F182–F185. doi: 10.1136/fn.83.3.F182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Varvarigou A., Bardin C. L., Beharry K., Chemtob S., Papageorgiou A., Aranda J. V. Early ibuprofen administration to prevent patent ductus arteriosus in premature newborn infants. JAMA. 1996 Feb 21;275(7):539–544. [PubMed] [Google Scholar]
- Verder H., Robertson B., Greisen G., Ebbesen F., Albertsen P., Lundstrøm K., Jacobsen T. Surfactant therapy and nasal continuous positive airway pressure for newborns with respiratory distress syndrome. Danish-Swedish Multicenter Study Group. N Engl J Med. 1994 Oct 20;331(16):1051–1055. doi: 10.1056/NEJM199410203311603. [DOI] [PubMed] [Google Scholar]
- de Courcy-Wheeler R. H., Wolfe C. D., Fitzgerald A., Spencer M., Goodman J. D., Gamsu H. R. Use of the CRIB (clinical risk index for babies) score in prediction of neonatal mortality and morbidity. Arch Dis Child Fetal Neonatal Ed. 1995 Jul;73(1):F32–F36. doi: 10.1136/fn.73.1.f32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Vries L. S., Eken P., Dubowitz L. M. The spectrum of leukomalacia using cranial ultrasound. Behav Brain Res. 1992 Jul 31;49(1):1–6. doi: 10.1016/s0166-4328(05)80189-5. [DOI] [PubMed] [Google Scholar]