Abstract
Aims: To study the frequency and reason for withdrawal/withholding of life sustaining treatment (LST) and do not resuscitate (DNR) orders in infants who died in a tertiary neonatal unit.
Methods: Infants who died at Homerton University Hospital between January 1998 and September 2001 were studied by retrospective analysis of patient records.
Results: The case notes of 71 (84%) of 85 infants who died were studied. Mode of death was withdrawal of LST in 28 (40%), DNR in 11 (15%), withholding of LST in two (3%), and natural in 30 (42%) infants. Withdrawal of LST was discussed with the parents of 39 seriously ill infants; 28 (72%) parents agreed. There was no difference in birth weight and gestational age of babies whose parents agreed or refused withdrawal of LST. White and Afro-Caribbean parents and those from the Indian subcontinent (20 of 23) were more likely to agree to withdrawal of LST than Black African or Jewish (eight of 16, p = 0.015) parents. The median age at withdrawal of LST was 4 days (range 1–57). The median duration between discussion and the parents agreeing to withdrawal of LST was 165 minutes (range 30–2160), and median duration between withdrawal of LST and death was 22 minutes (range 5–210). The most common reason for withdrawal of LST was complications of extreme prematurity (68%).
Conclusion: The most common mode of death was withdrawal of LST, and the most common reason was complications of extreme prematurity. The ethnic and cultural background of the parents influenced agreement to withdrawal of LST.
Full Text
The Full Text of this article is available as a PDF (98.2 KB).
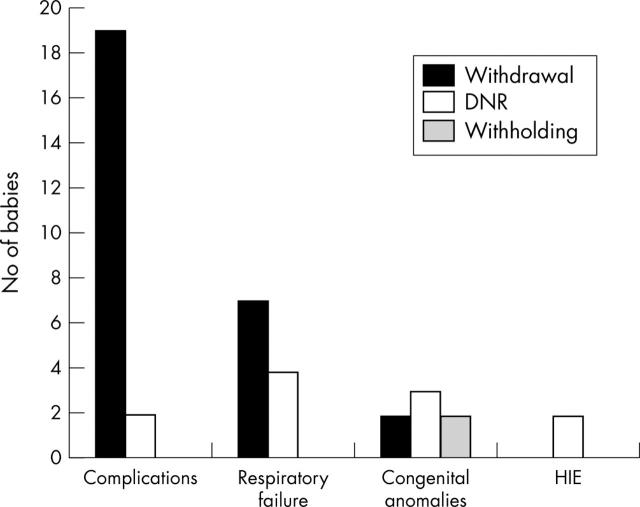
Figure 1.
Diagnosis in 41 babies who died after withdrawal or withholding of life sustaining treatment or do not resuscitate (DNR) orders. HIE, Hypoxic ischaemic encephalopathy; complications, complications of extreme prematurity.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Beckwith J. B. The value of the pediatric postmortem examination. Pediatr Clin North Am. 1989 Feb;36(1):29–36. doi: 10.1016/s0031-3955(16)36614-7. [DOI] [PubMed] [Google Scholar]
- Boréus L. O. Pain in the newborn--pharmacodynamic aspects. Dev Pharmacol Ther. 1990;15(3-4):142–148. doi: 10.1159/000457637. [DOI] [PubMed] [Google Scholar]
- Brodlie Malcolm, Laing Ian A., Keeling Jean W., McKenzie Kathryn J. Ten years of neonatal autopsies in tertiary referral centre: retrospective study. BMJ. 2002 Mar 30;324(7340):761–763. doi: 10.1136/bmj.324.7340.761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Côté J. J., Morse J. M., James S. G. The pain response of the postoperative newborn. J Adv Nurs. 1991 Apr;16(4):378–387. doi: 10.1111/j.1365-2648.1991.tb03426.x. [DOI] [PubMed] [Google Scholar]
- Doyal L., Larcher V. F. Drafting guidelines for the withholding or withdrawing of life sustaining treatment in critically ill children and neonates. Arch Dis Child Fetal Neonatal Ed. 2000 Jul;83(1):F60–F63. doi: 10.1136/fn.83.1.F60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doyal L., Wilsher D. Towards guidelines for withholding and withdrawal of life prolonging treatment in neonatal medicine. Arch Dis Child Fetal Neonatal Ed. 1994 Jan;70(1):F66–F70. doi: 10.1136/fn.70.1.f66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duff R. S., Campbell A. G. Moral and ethical dilemmas in the special-care nursery. N Engl J Med. 1973 Oct 25;289(17):890–894. doi: 10.1056/NEJM197310252891705. [DOI] [PubMed] [Google Scholar]
- Goh A. Y., Lum L. C., Chan P. W., Bakar F., Chong B. O. Withdrawal and limitation of life support in paediatric intensive care. Arch Dis Child. 1999 May;80(5):424–428. doi: 10.1136/adc.80.5.424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar P., Angst D. B., Taxy J., Mangurten H. H. Neonatal autopsies: a 10-year experience. Arch Pediatr Adolesc Med. 2000 Jan;154(1):38–42. [PubMed] [Google Scholar]
- Partridge J. C., Wall S. N. Analgesia for dying infants whose life support is withdrawn or withheld. Pediatrics. 1997 Jan;99(1):76–79. doi: 10.1542/peds.99.1.76. [DOI] [PubMed] [Google Scholar]
- Reynolds R. C. Autopsies--benefits to the family. Am J Clin Pathol. 1978 Feb;69(2 Suppl):220–222. [PubMed] [Google Scholar]
- Roy Pierre-Marie, Gras Emmanuelle. Images in clinical medicine. Cerebral venous thrombosis. N Engl J Med. 2003 Oct 30;349(18):1730–1730. doi: 10.1056/NEJMicm010862. [DOI] [PubMed] [Google Scholar]
- Scanlon J. W. Appreciating neonatal pain. Adv Pediatr. 1991;38:317–333. [PubMed] [Google Scholar]
- Snowdon C., Garcia J., Elbourne D. Making sense of randomization; responses of parents of critically ill babies to random allocation of treatment in a clinical trial. Soc Sci Med. 1997 Nov;45(9):1337–1355. doi: 10.1016/s0277-9536(97)00063-4. [DOI] [PubMed] [Google Scholar]
- Wall S. N., Partridge J. C. Death in the intensive care nursery: physician practice of withdrawing and withholding life support. Pediatrics. 1997 Jan;99(1):64–70. doi: 10.1542/peds.99.1.64. [DOI] [PubMed] [Google Scholar]
- Whitelaw A. Death as an option in neonatal intensive care. Lancet. 1986 Aug 9;2(8502):328–331. doi: 10.1016/s0140-6736(86)90014-0. [DOI] [PubMed] [Google Scholar]
- Wu Yvonne W., Hamrick Shannon E. G., Miller Steven P., Haward Marlyse F., Lai Michael C., Callen Peter W., Barkovich A. James, Ferriero Donna M. Intraventricular hemorrhage in term neonates caused by sinovenous thrombosis. Ann Neurol. 2003 Jul;54(1):123–126. doi: 10.1002/ana.10619. [DOI] [PubMed] [Google Scholar]
- Young E. W., Stevenson D. K. Limiting treatment for extremely premature, low-birth-weight infants (500 to 750 g). Am J Dis Child. 1990 May;144(5):549–552. doi: 10.1001/archpedi.1990.02150290043023. [DOI] [PubMed] [Google Scholar]
- deVeber G., Andrew M., Adams C., Bjornson B., Booth F., Buckley D. J., Camfield C. S., David M., Humphreys P., Langevin P. Cerebral sinovenous thrombosis in children. N Engl J Med. 2001 Aug 9;345(6):417–423. doi: 10.1056/NEJM200108093450604. [DOI] [PubMed] [Google Scholar]