Abstract
AIMS—The aims of this study were to examine the influence of advanced recipient and donor age on the long term outcome of corneal transplantation. METHODS—Records of 1036 penetrating corneal grafts in recipients aged ⩾80 years at surgery (defined as the elderly subset) and 8092 donor corneas used for transplantation were obtained from the Australian Corneal Graft Register database. Kaplan-Meier graft survival plots were compared using log rank statistics. RESULTS—Elderly recipients constituted 15% of the recipient pool. The major indication for corneal transplantation in the elderly was bullous keratopathy. Graft survival fell with increasing recipient age (p < 0.00001); the major cause of graft failure was rejection (33%). The desired outcome in 51% of cases was to improve vision and in 42% of cases to relieve pain; 23% of elderly recipients achieved a Snellen acuity of 6/18 or better in the grafted eye and 66% recorded improved acuity after transplantation. Elderly recipients suffered more complications and comorbidities in the grafted eye than did younger recipients. Donor age (stratified in 10 year intervals) did not influence corneal graft survival significantly (p = 0.10). CONCLUSIONS—Elderly graft recipients fared less well after corneal transplantation than did younger recipients, but outcomes in terms of long term graft survival and visual rehabilitation were still good. Donor age did not affect graft survival.
Full Text
The Full Text of this article is available as a PDF (111.4 KB).
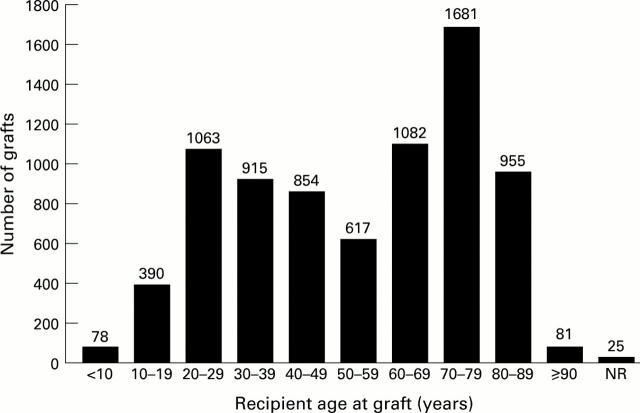
Figure 1 .
Distribution of recipient ages at graft in a cohort of 7741 patients undergoing penetrating corneal transplantation. NR = not recorded.
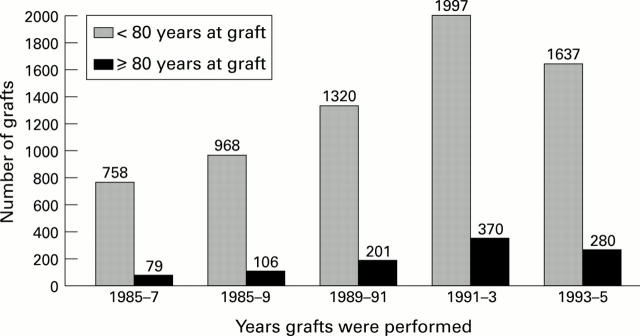
Figure 2 .
Number of corneal grafts in elderly recipients aged ⩾80 years at the time of graft compared with those age <80 years, showing the influence of calendar years in which the grafts were performed.
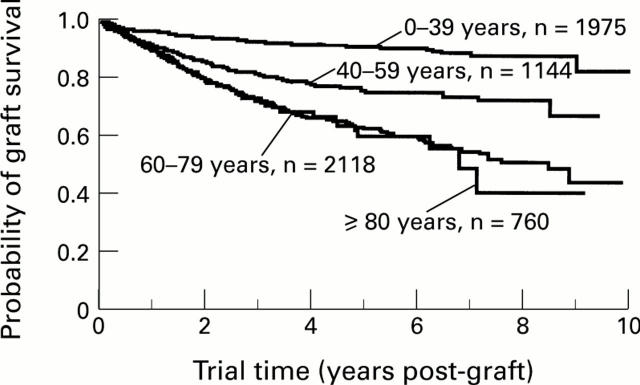
Figure 3 .
Kaplan-Meier corneal graft survival plots stratified according to recipient age at graft. For each curve, n = number initially at risk.
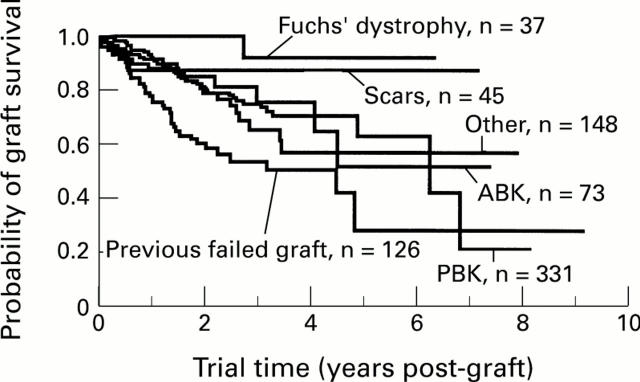
Figure 4 .
Kaplan-Meier graft survival plots in recipients aged ⩾80 years at graft, stratified according to the most common indications for transplantation in this subset. For each curve, n = number initially at risk. Scars = corneal scars and opacities; ABK = aphakic bullous keratopathy; PBK = pseudophakic bullous keratopathy.
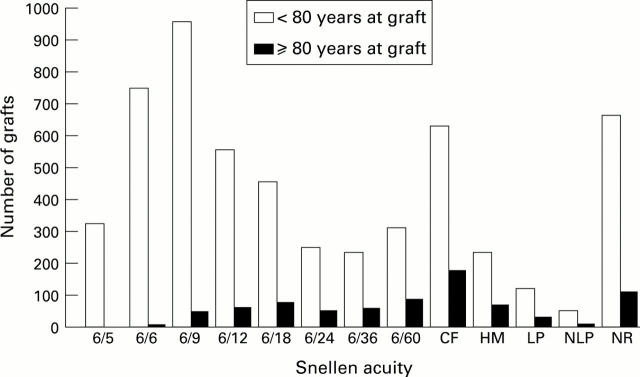
Figure 5 .
Snellen acuity at the time of most recent follow up for elderly corneal graft recipients (⩾80 years) and for younger recipients (<80 years). CF = counting fingers at 1 metre; HM = hand movements; LP = light perception; NLP = no light perception; NR= not recorded.
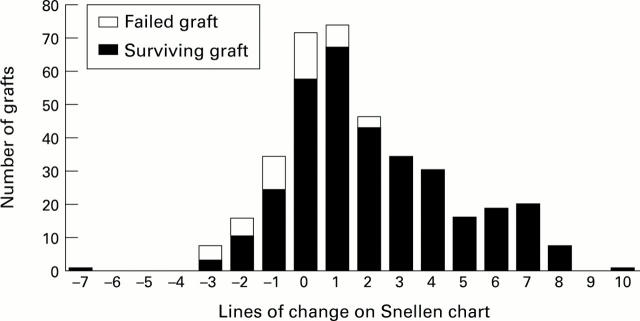
Figure 6 .
Number of lines of change on the Snellen chart at the time of most recent follow up, compared with Snellen acuity immediately before corneal transplantation, for elderly corneal graft recipients (⩾80 years).
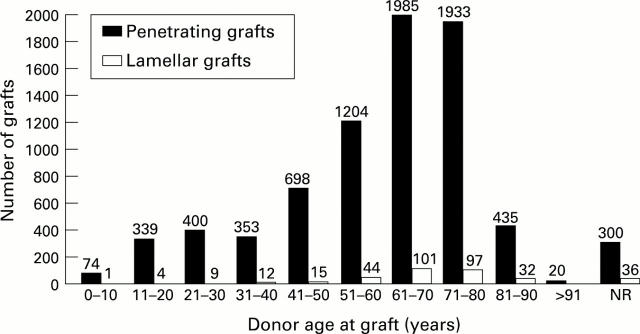
Figure 7 .
Number of penetrating and lamellar corneal grafts performed using tissue from corneal donors of different ages, stratified in 10 year intervals. NR = not recorded.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Ashcroft G. S., Horan M. A., Ferguson M. W. The effects of ageing on cutaneous wound healing in mammals. J Anat. 1995 Aug;187(Pt 1):1–26. [PMC free article] [PubMed] [Google Scholar]
- Bourne W. M., Hodge D. O., Nelson L. R. Corneal endothelium five years after transplantation. Am J Ophthalmol. 1994 Aug 15;118(2):185–196. doi: 10.1016/s0002-9394(14)72898-3. [DOI] [PubMed] [Google Scholar]
- Cavanagh H. D. Eye banking 1995: danger and opportunity. Cornea. 1995 Nov;14(6):545–546. [PubMed] [Google Scholar]
- Cerimele D., Celleno L., Serri F. Physiological changes in ageing skin. Br J Dermatol. 1990 Apr;122 (Suppl 35):13–20. doi: 10.1111/j.1365-2133.1990.tb16120.x. [DOI] [PubMed] [Google Scholar]
- Chandra R. K. Effect of vitamin and trace-element supplementation on immune responses and infection in elderly subjects. Lancet. 1992 Nov 7;340(8828):1124–1127. doi: 10.1016/0140-6736(92)93151-c. [DOI] [PubMed] [Google Scholar]
- Chu W., Dahl P., O'Neill M. J. Benefits of specular microscopy in evaluating eye donors aged 66 and older. Cornea. 1995 Nov;14(6):568-70, 634. [PubMed] [Google Scholar]
- Kliger C. H. Use of ethical criteria in medical decision making. Corneal transplantation. Arch Ophthalmol. 1995 Aug;113(8):988–993. doi: 10.1001/archopht.1995.01100080038027. [DOI] [PubMed] [Google Scholar]
- Maguire M. G., Stark W. J., Gottsch J. D., Stulting R. D., Sugar A., Fink N. E., Schwartz A. Risk factors for corneal graft failure and rejection in the collaborative corneal transplantation studies. Collaborative Corneal Transplantation Studies Research Group. Ophthalmology. 1994 Sep;101(9):1536–1547. doi: 10.1016/s0161-6420(94)31138-9. [DOI] [PubMed] [Google Scholar]
- Mattern R. M., Heck E. L., Cavanagh H. D. The impact on tissue utilization of screening donor corneas by specular microscopy at the University of Texas Southwestern Medical Center. Cornea. 1995 Nov;14(6):562–567. [PubMed] [Google Scholar]
- Moyes A. L., Holland E. J., Palmon F. E., Dvorak J. A., Doughman D. J. Tissue utilization at the Minnesota Lions' Eye Bank. Cornea. 1995 Nov;14(6):571–577. [PubMed] [Google Scholar]
- Murphy C., Alvarado J., Juster R., Maglio M. Prenatal and postnatal cellularity of the human corneal endothelium. A quantitative histologic study. Invest Ophthalmol Vis Sci. 1984 Mar;25(3):312–322. [PubMed] [Google Scholar]
- Paganelli R., Quinti I., Fagiolo U., Cossarizza A., Ortolani C., Guerra E., Sansoni P., Pucillo L. P., Scala E., Cozzi E. Changes in circulating B cells and immunoglobulin classes and subclasses in a healthy aged population. Clin Exp Immunol. 1992 Nov;90(2):351–354. doi: 10.1111/j.1365-2249.1992.tb07954.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peto R., Pike M. C., Armitage P., Breslow N. E., Cox D. R., Howard S. V., Mantel N., McPherson K., Peto J., Smith P. G. Design and analysis of randomized clinical trials requiring prolonged observation of each patient. I. Introduction and design. Br J Cancer. 1976 Dec;34(6):585–612. doi: 10.1038/bjc.1976.220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peto R., Pike M. C., Armitage P., Breslow N. E., Cox D. R., Howard S. V., Mantel N., McPherson K., Peto J., Smith P. G. Design and analysis of randomized clinical trials requiring prolonged observation of each patient. II. analysis and examples. Br J Cancer. 1977 Jan;35(1):1–39. doi: 10.1038/bjc.1977.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tuft S. J., Coster D. J. The corneal endothelium. Eye (Lond) 1990;4(Pt 3):389–424. doi: 10.1038/eye.1990.53. [DOI] [PubMed] [Google Scholar]
- Vail A., Gore S. M., Bradley B. A., Easty D. L., Rogers C. A., Armitage W. J. Influence of donor and histocompatibility factors on corneal graft outcome. Transplantation. 1994 Dec 15;58(11):1210–1216. [PubMed] [Google Scholar]
- Williams K. A., Roder D., Esterman A., Muehlberg S. M., Coster D. J. Factors predictive of corneal graft survival. Report from the Australian Corneal Graft Registry. Ophthalmology. 1992 Mar;99(3):403–414. doi: 10.1016/s0161-6420(92)31960-8. [DOI] [PubMed] [Google Scholar]