Abstract
AIMS/BACKGROUND—To determine the epidemiological characteristics and risk factors predisposing to corneal ulceration in Madurai, south India, and to identify the specific pathogenic organisms responsible for infection. METHODS—All patients with suspected infectious central corneal ulceration presenting to the ocular microbiology and cornea service at Aravind Eye Hospital, Madurai, from 1 January to 31 March 1994 were evaluated. Sociodemographic data and information pertaining to risk factors were recorded, all patients were examined, and corneal cultures and scrapings were performed. RESULTS—In the 3 month period 434 patients with central corneal ulceration were evaluated. A history of previous corneal injury was present in 284 patients (65.4%). Cornea cultures were positive in 297 patients (68.4%). Of those individuals with positive cultures 140 (47.1%) had pure bacterial infections, 139 (46.8%) had pure fungal infections, 15 (5.1%) had mixed bacteria and fungi, and three (1.0%) grew pure cultures of Acanthamoeba. The most common bacterial pathogen isolated was Streptococcus pneumoniae, representing 44.3% of all positive bacterial cultures, followed by Pseudomonas spp (14.4%). The most common fungal pathogen isolated was Fusarium spp, representing 47.1% of all positive fungal cultures, followed by Aspergillus spp (16.1%). CONCLUSIONS—Central corneal ulceration is a common problem in south India and most often occurs after a superficial corneal injury with organic material. Bacterial and fungal infections occur in equal numbers with Streptococcus pneumoniae accounting for the majority of bacterial ulcers and Fusarium spp responsible for most of the fungal infections. These findings have important public health implications for the treatment and prevention of corneal ulceration in the developing world.
Full Text
The Full Text of this article is available as a PDF (112.4 KB).
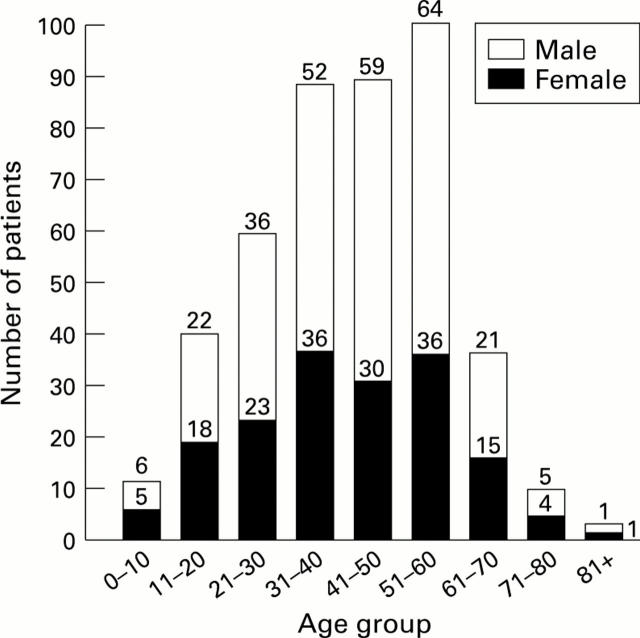
Figure 1 .
Age and sex distribution of patients with corneal ulceration in south India.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Brilliant L. B., Pokhrel R. P., Grasset N. C., Lepkowski J. M., Kolstad A., Hawks W., Pararajasegaram R., Brilliant G. E., Gilbert S., Shrestha S. R. Epidemiology of blindness in Nepal. Bull World Health Organ. 1985;63(2):375–386. [PMC free article] [PubMed] [Google Scholar]
- Carmichael T. R., Wolpert M., Koornhof H. J. Corneal ulceration at an urban African hospital. Br J Ophthalmol. 1985 Dec;69(12):920–926. doi: 10.1136/bjo.69.12.920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chirambo M. C., Benezra D. Causes of blindness among students in blind school institutions in a developing country. Br J Ophthalmol. 1976 Sep;60(9):665–668. doi: 10.1136/bjo.60.9.665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chirambo M. C., Tielsch J. M., West K. P., Jr, Katz J., Tizazu T., Schwab L., Johnson G., Swartwood J., Taylor H. R., Sommer A. Blindness and visual impairment in southern Malawi. Bull World Health Organ. 1986;64(4):567–572. [PMC free article] [PubMed] [Google Scholar]
- Courtright P., Lewallen S., Kanjaloti S., Divala D. J. Traditional eye medicine use among patients with corneal disease in rural Malawi. Br J Ophthalmol. 1994 Nov;78(11):810–812. doi: 10.1136/bjo.78.11.810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunlop A. A., Wright E. D., Howlader S. A., Nazrul I., Husain R., McClellan K., Billson F. A. Suppurative corneal ulceration in Bangladesh. A study of 142 cases examining the microbiological diagnosis, clinical and epidemiological features of bacterial and fungal keratitis. Aust N Z J Ophthalmol. 1994 May;22(2):105–110. doi: 10.1111/j.1442-9071.1994.tb00775.x. [DOI] [PubMed] [Google Scholar]
- Erie J. C., Nevitt M. P., Hodge D. O., Ballard D. J. Incidence of ulcerative keratitis in a defined population from 1950 through 1988. Arch Ophthalmol. 1993 Dec;111(12):1665–1671. doi: 10.1001/archopht.1993.01090120087027. [DOI] [PubMed] [Google Scholar]
- Gilbert C. E., Wood M., Waddel K., Foster A. Causes of childhood blindness in east Africa: results in 491 pupils attending 17 schools for the blind in Malawi, Kenya and Uganda. Ophthalmic Epidemiol. 1995 Jun;2(2):77–84. doi: 10.3109/09286589509057086. [DOI] [PubMed] [Google Scholar]
- Gonzales C. A., Srinivasan M., Whitcher J. P., Smolin G. Incidence of corneal ulceration in Madurai district, South India. Ophthalmic Epidemiol. 1996 Dec;3(3):159–166. doi: 10.3109/09286589609080122. [DOI] [PubMed] [Google Scholar]
- Hagan M., Wright E., Newman M., Dolin P., Johnson G. Causes of suppurative keratitis in Ghana. Br J Ophthalmol. 1995 Nov;79(11):1024–1028. doi: 10.1136/bjo.79.11.1024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones B. R. Principles in the management of oculomycosis. XXXI Edward Jackson memorial lecture. Am J Ophthalmol. 1975 May;79(5):719–751. doi: 10.1016/0002-9394(75)90730-8. [DOI] [PubMed] [Google Scholar]
- Katz N. N., Wadud S. A., Ayazuddin M. Corneal ulcer disease in Bangladesh. Ann Ophthalmol. 1983 Sep;15(9):834–836. [PubMed] [Google Scholar]
- Khan M. U., Haque E., Khan M. R. Prevalence & causes of blindness in rural Bangladesh. Indian J Med Res. 1985 Sep;82:257–262. [PubMed] [Google Scholar]
- Liesegang T. J., Forster R. K. Spectrum of microbial keratitis in South Florida. Am J Ophthalmol. 1980 Jul;90(1):38–47. doi: 10.1016/s0002-9394(14)75075-5. [DOI] [PubMed] [Google Scholar]
- Ormerod L. D. Causation and management of microbial keratitis in subtropical Africa. Ophthalmology. 1987 Dec;94(12):1662–1668. doi: 10.1016/s0161-6420(87)33235-x. [DOI] [PubMed] [Google Scholar]
- Rapoza P. A., West S. K., Katala S. J., Taylor H. R. Prevalence and causes of vision loss in central Tanzania. Int Ophthalmol. 1991 Mar;15(2):123–129. doi: 10.1007/BF00224465. [DOI] [PubMed] [Google Scholar]
- Rubinfeld R. S., Cohen E. J., Arentsen J. J., Laibson P. R. Diphtheroids as ocular pathogens. Am J Ophthalmol. 1989 Sep 15;108(3):251–254. doi: 10.1016/0002-9394(89)90114-1. [DOI] [PubMed] [Google Scholar]
- Smith G. T., Taylor H. R. Epidemiology of corneal blindness in developing countries. Refract Corneal Surg. 1991 Nov-Dec;7(6):436–439. [PubMed] [Google Scholar]
- Thylefors B. Epidemiological patterns of ocular trauma. Aust N Z J Ophthalmol. 1992 May;20(2):95–98. doi: 10.1111/j.1442-9071.1992.tb00718.x. [DOI] [PubMed] [Google Scholar]
- Thylefors B., Négrel A. D., Pararajasegaram R., Dadzie K. Y. Available data on blindness (update 1994) Ophthalmic Epidemiol. 1995 Mar;2(1):5–39. doi: 10.3109/09286589509071448. [DOI] [PubMed] [Google Scholar]
- Upadhyay M. P., Karmacharya P. C., Koirala S., Tuladhar N. R., Bryan L. E., Smolin G., Whitcher J. P. Epidemiologic characteristics, predisposing factors, and etiologic diagnosis of corneal ulceration in Nepal. Am J Ophthalmol. 1991 Jan 15;111(1):92–99. doi: 10.1016/s0002-9394(14)76903-x. [DOI] [PubMed] [Google Scholar]
- di Bisceglie A. M., Carmichael T. R. Factors predisposing to central corneal ulceration in a developing population. S Afr Med J. 1987 Jun 20;71(12):769–770. [PubMed] [Google Scholar]